Impact of obesity on aortic root calcification and coronary calcification using multi-detector CT
- DOI
- 10.1016/j.artres.2014.12.001How to use a DOI?
- Keywords
- Obesity; BMI; Coronary calcification; Aortic root calcification; MDCT
- Abstract
Objective: The impact of obesity measured by BMI on cardiovascular diseases remains controversial. We investigated the impact of obesity measured by BMI on the prevalence and correlation of aortic root calcification (ARC) and coronary artery calcification (CAC) in patients assessed by multi-detector CT (MDCT) angiography.
Materials and methods: A total of 175 patients with intermediate pretest probability of ischemic heart disease based on age, sex, and symptoms who referred from cardiology clinic to 64-MDCT angiography examination for assessment of coronary artery disease were eligible for enrollment in this cross sectional study. The patients were divided into 2 groups according to their BMI. Non obese group (BMI < 25) composed of 73 (42%) patients (male 41 (56%), female 32 (44%) with a mean age 55 ± 8 years. Obese group (BMI ≥ 25) composed of 102 (58%) patients (male 45 (44%), female 58 (56%) with mean age 56 ± 7 years).
Results: ARC was significantly associated with coronary artery calcification pattern in both non obese and obese groups (r = 461, P = 0.000) and (r = 0.358, P = 0.000) respectively. The significant association between ARC and CAC persisted even after adjustment for age, hypertension, smoking, hyperlipdemia and presence of multiple cardiac risk factor in both non obese and obese groups (95% C.I. = 0.106, 0.259, P = 0.000) and (95% C.I. = 0.108, 0.610, P = 0.006) respectively.
Conclusion: ARC was significantly correlated with CAC irrespective of BMI status.
- Copyright
- © 2014 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
The prevalence of obesity has been risen dramatically over the last decade and the obesity now is the sixth most common risk factor for worldwide disease burden. The prevalence rate of obesity in some Arabic countries is higher than European countries or about the same as United State according to WHO estimates.1
BMI is the most commonly used anthropometric measure to define the overall adiposity and report its association with cardiovascular diseases burden and progression.2
Recently, coronary artery calcification (CAC) as a marker of subclinical atherosclerosis, has an incremental prognostic role beyond traditional cardiac risk factors and that CAC has been associated with a higher cardiovascular burden and improved risk stratification especially in intermediate risk patients.3
Multiple studies have shown a significant association between aortic arch, thoracic and abdominal aorta with coronary artery disease and calcification.4–7
According to our knowledge, there are limited data regarding the importance of aortic root calcification in cardiovascular disease or its association with CAC pattern.
Main aim of this study was to investigate the impact of obesity measured by BMI on the prevalence and correlation of ARC and CAC in patients with intermediate pretest probability of ischemic heart disease assessed by multi-detector CT (MDCT) angiography.
Methods
This cross sectional study was carried out in the Cardiology center at our Teaching Hospital between January and December 2013. All patients provided written informed consent to participate in the study and the study was approved by the Ethical Committee of our institution.
We recruited 196 consecutive Iraqi patients with intermediate pretest probability of ischemic heart disease based on age, sex, and symptoms who referred from cardiology clinic to 64-MDCT angiography examination for assessment of coronary artery disease. Twenty-one patients were excluded because of poor examination technique or motion artifact (8), aortic root anomalies or dissection (6), prior history of implanted stent in a coronary artery or coronary revascularization (4),morbid obesity (BMI > 40) (2) and missing data (1).
A total of 175 patients were eligible for enrollment in this study. Referral symptoms for MDCT examination were chest pain (n = 125, 71.5%), dyspnea (n = 32, 18%) syncope (n = 11, 6.3%), equivocal exercise tolerance test (n = 4, 2.5%) and others (n = 3, 1.7%).
According to body mass index (BMI), the patients were classified into non obese group (BMI 18–24.9) and obese group (BMI 25–40). BMI was calculated as body weight in kilograms divided by height in meters squared (kg/m2).
Using standard physician-based questionnaires, a history of conventional cardiac risk factors for coronary artery disease was obtained from each patient at the time of the coronary MDCT angiography examination including a positive family history of premature CAD (occurring in men before 55 years of age and before 65 years of age in women); current smoking history (>10 cigarettes per day in the last year); a history of hypertension or use of anti-hypertension medications; hyperlipidemia, defined as total cholesterol ≥ 200 mg/dl or triglyceride levels ≥ 150 mg/dl or the use of lipid-lowering drugs and a history of diabetes mellitus or the use of insulin or glucose-lowering drugs. Patient with two or more cardiac risk factors was labeled as having multiple risk factors.
Calcium score was categorized as < 10 (no or minimal calcification), 10–99 (mild), 100–399 (moderate), and ≥400 (extensive calcification).calcium score above 10 was used to define the presence of calcification in both coronary artery and aortic root.
MDCT scan protocol
CT coronary angiography was performed with a 64-slice scanner (Aquillon 64, V4.51 ER 010, Toshiba Medical Systems, Tochigi, Japan) with retrospective ECG gating. Before multi-slice CT angiography, a non-contrast CT was acquired to measure the calcium score according to the Agatston method for the entire heart (total heart calcium) using sequential scans with a slice thickness of 3 mm. The aortic root was defined as the section of the aorta lying within 3 cm of the caudal aspect of the aortic annulus containing the sinuses of Valsalva and the sinotubular junction. The total calcium score of the aortic root was calculated using the Agatston method. The scan was obtained from the aortic arch to the level of the diaphragm during a single breath-hold. The following parameters were used during the ECG-triggered scanning protocol: 32.5 × 32.5 cm collimation width, 0.5 mm slice thickness, 0.35 s rotation time, 120 kV tube voltage, 150 mAs effective tube current, and a table feed of 0.3 mm/rotation at 75% of the R–R cardiac cycle. The examination time was approximately 10 s.
CT images were reconstructed using a smooth kernel (B25f) with a slice thickness of 0.5 mm in 0.3 mm increments). CT data sets were transferred to a dedicated workstation (Vitrea 2 Workstation, Vital Images, Plymouth, Minnesota, USA) for image analysis.
All MDCT images were assessed by two independent radiologists with more than 5 years’ experience in coronary MDCT angiography interpretation.
Statistical analysis
Data are presented as mean ± standard deviation or as number with percentages. Categorical data are expressed as frequencies and were compared using Pearson’s chi-square test. Pearson’s correlation was used to test the significance of the correlation between the aortic root calcification and coronary artery calcification. Multiple linear regression was used as appropriate. SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. P < 0.05 was considered statistically significant.
Results
One hundred and seventy five patients {female 89 (51%), male 86 (49%) with a mean age 56.3 ± 6 years} were enrolled in this study. The patients were divided into 2 groups according to their BMI.
Non obese group (BMI < 25) composed of 73 (42%) patients (male 41 (56%), female 32 (44%) with a mean age 55 ± 8 years. Obese group (BMI 27–40) composed of 102 (58%) patients (male 45 (44%), female 58 (56%) with mean age 56 ± 7 years). Patients characteristics are summarized in Table 1. There were no statistically significant differences in the distribution of clinical risk factors reported between obese and non-obese groups (P > 0.5). Also, no statistically significant differences were observed in the prevalence of CAC and ARC between obese and non-obese groups except at moderate calcification group of ARC in which the prevalence of calcification was more significant in non obese group (p = 0.024).
| Parameter | Non obese | Obese | P Value |
|---|---|---|---|
| Age | 55 ± 8 years | 56 ± 7 years | |
| Male | 41 (56%) | 45 (44%) | 0.11 |
| Female | 32 (44%) | 57 (56%) | 0.11 |
| Risk factors | |||
| Hypertension | 43 (59%) | 51 (50%) | 0.24 |
| Smoking | 25 (34%) | 28 (27.5%) | 0.33 |
| hyperlipidemia | 10 (13.5%) | 23 (22.5%) | 0.14 |
| Diabetes | 7 (9.5%) | 12 (12%) | 0.64 |
| Family history | 10 (13.5%) | 10 (10%) | 0.42 |
| Multiple | 28 (38%) | 30 (29.5%) | 0.21 |
| CAC | |||
| 0–9 | 51 (70%) | 71 (70%) | 0.97 |
| 10–99 | 9 (12%) | 8 (8%) | 0.32 |
| 100–399 | 9 (12%) | 16 (15%) | 0.53 |
| ≥400 | 4 (6%) | 7 (7%) | 0.71 |
| ARC | |||
| 0–9 | 60 (82%) | 83 (81%) | 0.89 |
| 10–99 | 5 (7%) | 12 (12%) | 0.27 |
| 100–399 | 7 (9.5%) | 2 (2%) | 0.024 |
| ≥400 | 1 (1.5%) | 5 (5%) | 0.2 |
Patients characteristics.
Non obese group: The prevalence of aortic root calcification was 18% (calcium score ≥ 10) while total coronary artery calcification prevalence was 30% (calcium score ≥ 10).
ARC was significantly associated with coronary artery calcification pattern (r = 461, P = 0.000) as in Fig. 1.
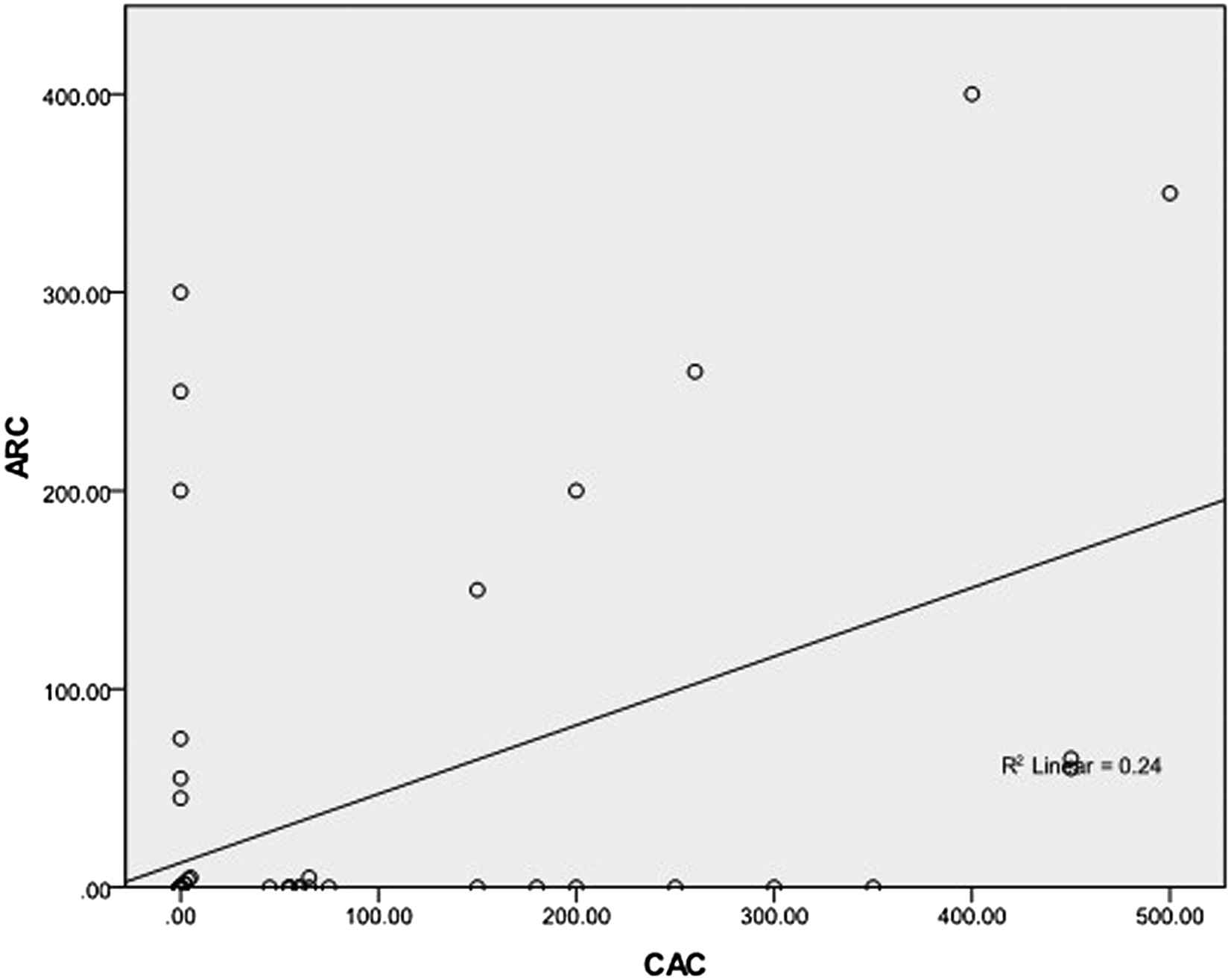
Significant correlation was observed between ARC and CAC pattern in non obese group (r = 461, P = 0.000).
The significant association between ARC and CAC persisted even after adjustment for age, hypertension, smoking, hyperlipdemia and presence of multiple cardiac risk factor (95% C.I. = 0.106, 0.259, P = 0.000).
In non obese male patients, the prevalence of ARC and CAC were 12% and 24.3% respectively and ARC was significantly associated with CAC (r = 636, P = 0.000) as in Fig. 2A.
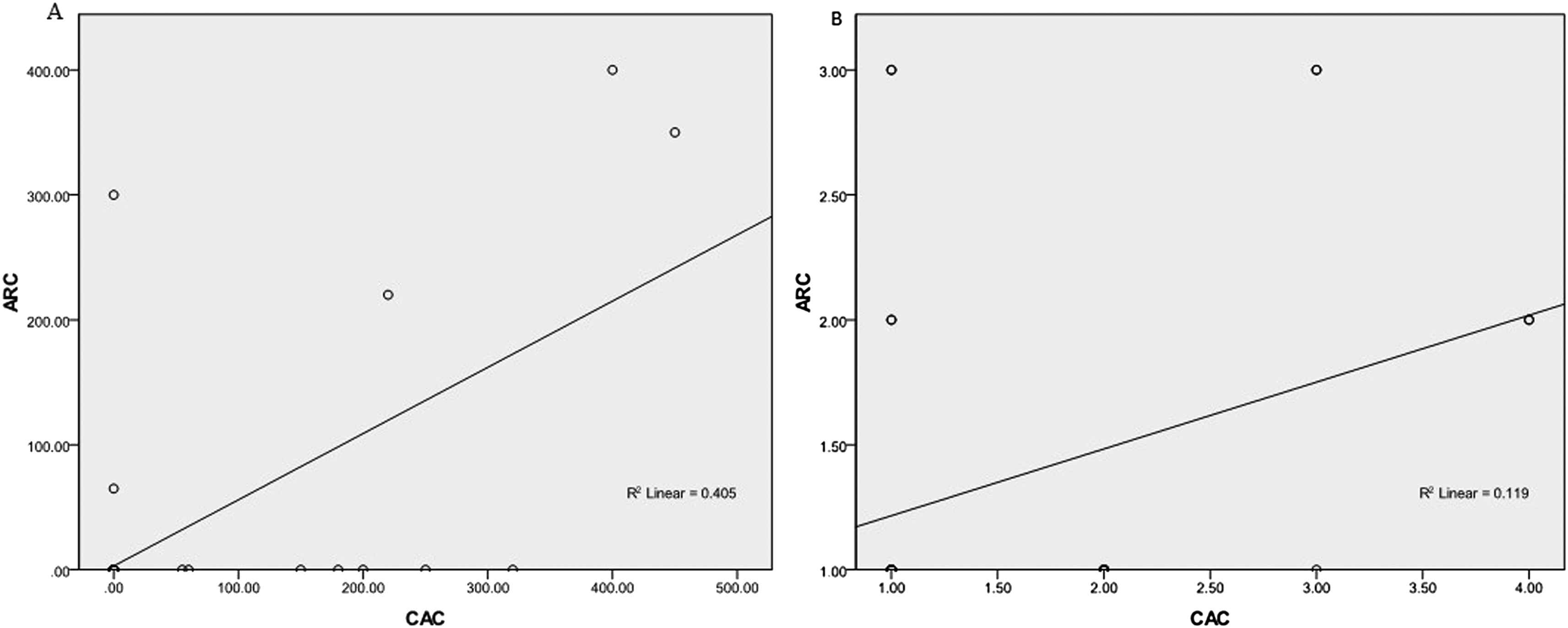
A Significant correlation was observed between ARC and CAC pattern in non obese male (r = 636, P = 0.000). B Significant correlation was observed between ARC and CAC pattern in non obese female (r = 0.344, P = 0.05).
While in non obese female patients, the prevalence of ARC and CAC were 25% and 37.5% respectively and there was a weak positive correlation between ARC and CAC (r = 0.344, P = 0.05) as in Fig. 2B.
Obese group: the prevalence of ARC was 19% (calcium score ≥ 10) while total coronary artery calcification was 30% (calcium score ≥ 10).
ARC was significantly associated with CAC pattern (r = 0.358, P = 0.000) as in Fig. 3.
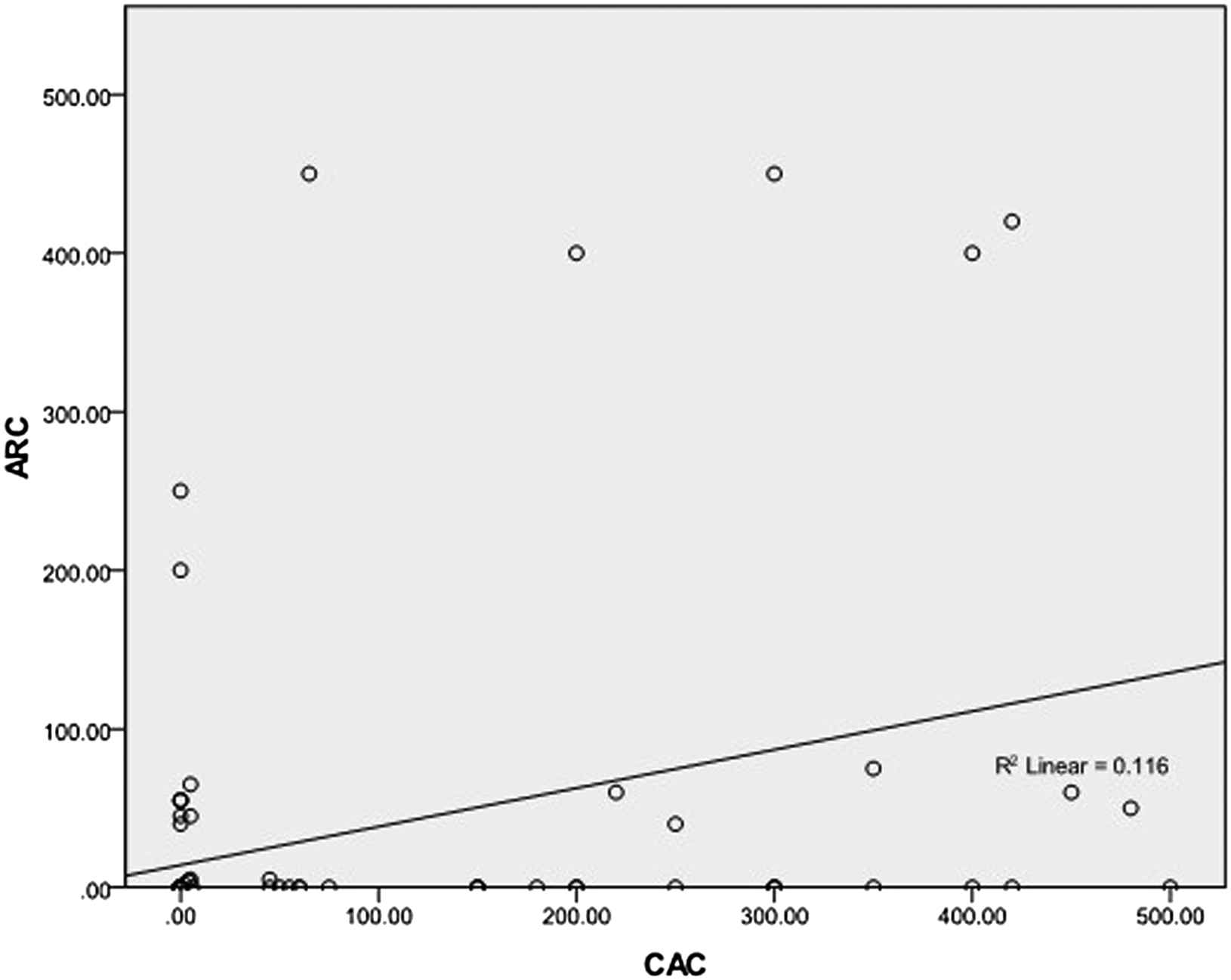
Significant correlation was observed between ARC and CAC pattern in obese group (r = 0.358, P = 0.000).
The significant association between ARC with CAC persisted even after adjustment for age, hypertension, smoking, hyperlipidemia and presence of multiple risk factors (95% C.I. = 0.108, 0.610, P = 0.006).
Regarding obese male patients, the prevalence of ARC and CAC were 20% and 42% respectively and ARC was correlated with CAC pattern (r = 0.319, P = 0.03) as in Fig. 4A.
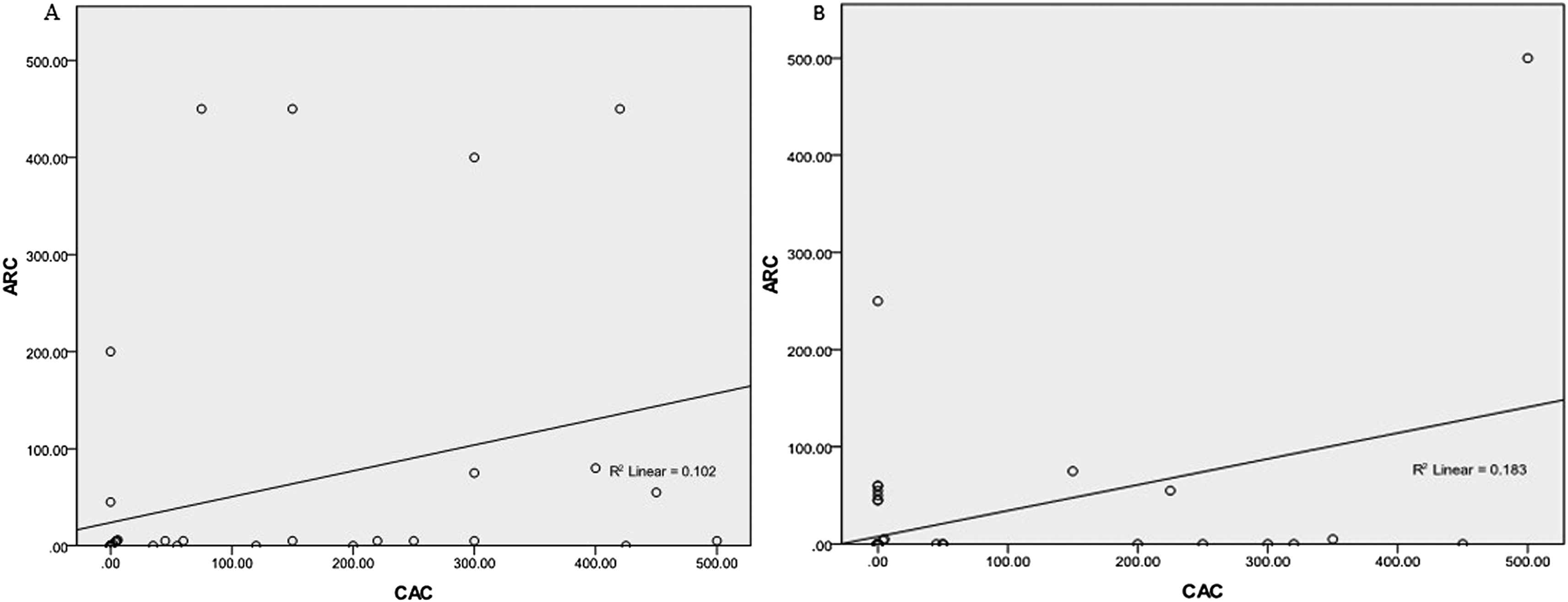
A Significant correlation was observed between ARC and CAC pattern in obese male (r = 0.319, P = 0.03). B Significant correlation was observed between ARC and CAC pattern in obese female (r = 0.427, P = 0.001).
Regarding obese female patients, the prevalence of ARC and CAC were 17.5% and 21% respectively and ARC was significantly associated with CAC pattern (r = 0.427, P = 0.001) as in Fig. 4B.
Discussion
A major finding of our study is that ARC was significantly correlated with CAC pattern in both obese and non obese groups and the obesity (according to our classification based on BMI) did not influence the correlation between ARC and CAC pattern.
Also, the prevalence rate of ARC and CAC were approximately similar in both obese and non obese groups except at moderate calcification group of ARC.
The importance of the aortic root arises from its close proximity to the cardiac chambers and the ostial origins of the right and left coronary arteries. The aortic root can also be evaluated by MDCT without additional radiation exposure or the use of contrast. Nowadays, assessment of the aortic root has been used increasingly to evaluate the morphology of the aorta prior to trans-catheter aortic valve implantation and in the screening of low-dose chest CT examination.8
Recently, arterial calcification is accepted as a valuable predictor of coronary artery disease and it has been reported that arterial calcification is a systemic pathological process impairing cardiovascular hemodynamic occurring in the early stages of atherosclerosis leading to increased cardiac mortality and morbidity.9
Moreover, the presence of coronary calcification in asymptomatic individuals has been shown to be associated with an increased risk for cardiovascular hard events. Thus, the presence of vascular calcification can be seen as an additional risk factor for cardiovascular hard events.9,10
The impact of obesity measured by BMI on cardiovascular disease particularly in elderly patients remains controversial.
There has been some concerns regarding the most accurate BMI cutoff values for the definition of obesity. Thus, a lower cutoff value for Asian population was reported for obesity definition (BMI > 25) as the health-related risk factors associated with obesity occur more frequently at a lower BMI in Asian populations than in other ethnic groups suggesting that BMI may not estimate the true body fat distribution.11
Recent prospective follow up studies using BMI cutoff value similar to our study have demonstrated that obese patients are not at increased risk of cardiac events compared to non obese patients suggesting that BMI per se has a weak discriminatory power to distinguish between fat and lean tissue.12
Cho et al. have investigated the association of obesity measured by BMI and waist to hip ratio with CAC in 530 Korean patients (mean age 56 years) with type 2 diabetes mellitus and found no significant difference in CAC levels between obese and non obese groups indicating that abdominal obesity measured by waist to hip ratio is associated with coronary atherosclerosis and provide additional information beyond BMI in predicting the risk of atherosclerosis.13
Furthermore, Kovacic et al. have assessed coronary calcification severity and BMI in 9993 patients with clinically significant coronary disease that underwent PCI and found an inverse relationship between BMI and CAC pattern suggesting more complicated relationship between BMI and CAC than previously thought.14
Interestingly, CAC was significantly higher in metabolically unhealthy subjects compared with metabolically healthy subjects regardless of obesity status in a large, health-screening population.15
In addition, non-obese but metabolically unhealthy subjects showed CAC similar to metabolically unhealthy obese subjects suggesting that metabolic health is more closely associated with subclinical atherosclerosis than obesity as assessed by CAC.15
Several studies have supported the concept that visceral fat deposit, rather than subcutaneous fat, has an important role in metabolic diseases and coronary atherosclerosis as many individuals with metabolic diseases have normal body weights in the clinical setting highlighting the idea that BMI may not be the accurate marker of increased risk of hypertension, coronary atherosclerosis or insulin resistance.13,16
Therefore, obesity per se is not necessarily equivalent to poor metabolic health.
In our study, the correlation of ARC and CAC was less prominent in non obese female (r = 0.344, P = 0.05).
Generally,the prevalence of vascular calcification was higher in men except after the age of 70.10
This pattern of prevalence can be explained by the protective role of menstrual cycle on the cardiovascular system leading to vascular calcification to occur at an older age in women.10
It has been reported that central obesity measures, waist circumference and waist-hip ratio, compared with BMI were better predictors of cardiovascular risk and waist circumference was the most predictive of cardiovascular risk particularly among Asian women.17
Waist circumference is recommended as the most practical tool to assess abdominal fat or central obesity in women which predicts risk of coronary artery disease independent of BMI and this has been supported by studies using computed tomography (CT).18
Allison et al. have examined 3028 self-referred individuals and found that visceral adipose thickness was associated with CAC in men, but not women.19
There were several limitations in our study. First, the population was not randomly selected because it involved only patients with an intermediate pretest probability of ischemic heart disease, creating the possibility of selection bias. Second, the number of patients was relatively small. Third, this is a cross sectional study, so that causality cannot be inferred. Fourth, we didn’t evaluate the progression of CAC and ARC as the obesity may be associated with arterial calcification progression.
Larger follow-up studies are needed to further investigate the impact of obesity measured by BMI on the CAC and ARC progression.
In conclusion, ARC was significantly correlated with CAC irrespective of BMI status. This correlation persisted in obese and non obese groups even after adjusted to age, hypertension, hyperlipidemia, smoking and presence of multiple risk factors.
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Sources of funding
There were no external funding sources for this study.
References
Cite this article
TY - JOUR AU - Hussein Nafakhi AU - Hasan A. Al-Nafakh AU - Abdulameer A. Al-Mosawi PY - 2014 DA - 2014/12/24 TI - Impact of obesity on aortic root calcification and coronary calcification using multi-detector CT JO - Artery Research SP - 27 EP - 32 VL - 9 IS - C SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2014.12.001 DO - 10.1016/j.artres.2014.12.001 ID - Nafakhi2014 ER -
