The acute effects of mental arithmetic, cold pressor and maximal voluntary contraction on arterial stiffness in young healthy subjects
Deceased.
- DOI
- 10.1016/j.artres.2014.02.002How to use a DOI?
- Keywords
- Mental stress; Cold pressor; Dynamic exercise; Blood pressure; Augmentation index; Pulse wave velocity
- Abstract
Background: Mental stress, dynamic exercise and cold pressor stimulation all increase blood pressure (BP); however, their effects on arterial stiffness are not well described.
Methods: Twenty-three young healthy subjects (14 female/9 males), aged 18–30 years (23 ± 3 years), underwent mental arithmetic stress (mental arithmetic test [MAT]), cold presser test (CPT) and dynamic exercise (30% of maximal voluntary contraction [30% MVC]). Blood pressure and indices of arterial stiffness, pulse wave velocity (PWV; m/sec) and augmentation index (AIx; %) were measured at baseline, during the intervention (MAT, CPT and 30% MVC), and at 5 min and 10 min after the end of the intervention on separate days within a 3-week period. All values are given as means and standard deviations; statistical analysis was carried out using JMP software (Version 7).
Results: During MAT, CPT and 30% MVC there were respective increases in heart rate (HR/min) 27%, 16% and 10% (P < 0.001); systolic BP 16%, 17% and 12% (P < 0.01); diastolic BP 15%, 23% and 15% (P < 0.01); AIx 13%, 29% and 30% (P < 0.05); and PWV 14%, 12% and 16% (P < 0.01). When the model was corrected for HR, systolic BP and diastolic BP the changes both in PWV and AIx remained significant (P < 0.01).
Conclusions: MAT, CPT and 30% MVC each increase the indices of arterial stiffness independently of HR and baseline blood pressure levels.
- Copyright
- © 2014 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
Aortic stiffness and wave reflections affect left ventricular function, coronary blood flow and the mechanical integrity of arteries.1 Arterial stiffness and its hemodynamic consequences are now established as predictors of adverse cardiovascular outcome.2 Pulse wave velocity and augmentation index are increasingly used in the clinical assessment of patients with hypertension and various cardiovascular (CV) risk factors.3 Arterial elastic properties and wave reflections are altered in the presence of cardiovascular risk factors such as smoking,3 diabetes mellitus,5 hypertension,6 obesity,7 hypercholesterolemia,8 and a family history of premature coronary artery disease.9 Also, they are modified by several pharmacologic and non-pharmacologic means such as nutritional products and lifestyle habits, including smoking cessation,4 caffeine intake,10 weight reduction and regular exercise.11
Measurement of arterial stiffness provides direct evidence of target organ damage and is now commonly made in assessing cardiovascular risk and is recommended in current ESH hypertension guidelines.12 Given the prognostic importance and therapeutic implications of a ‘single measure’ it is essential that such measurements are accurate. It is important to understand how common experiences e.g. stress, may influence such measurements. Furthermore, as with other hemodynamic responses, it is important to know if arterial stiffness changes acutely in response to physiological stimuli.
Mental stress, physical activity and environmental temperature adjustment are common in everyday life. Stress has been shown recently to be an important factor in predicting various physical and mental health outcomes, including cardiovascular morbidity. Atherosclerosis and coronary artery disease are associated with chronic mental stress. Acute stress may induce myocardial ischemia,13 left ventricular dysfunction14 and may even lead to sudden cardiac death.15 Both mental and physical stress release catecholamines16 they may also contribute to endothelial dysfunction.17 Both catecholamine levels and endothelial function are regulators of arterial stiffness and wave reflections.18
Arterial responses to the cold pressor test (CPT) are due to sympathetic activation and the CPT is widely used for the assessment of cardiovascular responses, particularly vasoconstriction.19 Our bodies respond to cold temperature by vasoconstriction to reduce heat loss to the surrounding environment. Being modulated by activation of the sympathetic nervous system, vasoconstriction is thus also related to the level of catecholamines in the blood.20
Constantly maintained hand-grip tension will also activate the sympathetic nervous system and increase blood pressure. The cortical impulses that initiate voluntary muscle contractions (the so-called central command) contribute to the increase in sympathetic tone. Local mechanisms also play a pivotal role in the triggering of this reflex. Muscle contraction activates afferent nerves sensitive to mechanical deformation (mechanoreceptors). The increase in muscle metabolism and the relative ischemia resulting from compression of blood vessels by the contracting muscle generates metabolic products that then activate chemo-sensitive afferent nerves (chemoreceptor or metaboreceptor). These chemoreceptors constitute the afferent limb of a reflex that results in sympathetic activation and increased blood pressure.21
We therefore examined hemodynamic and arterial responses to mental stress, cold pressor and isometric hand grip exercise (maximal voluntary contraction) in a group of healthy volunteers.
Materials and methods
The study included 23 young, healthy normotensive subjects who were not on any medication or agents that influence blood pressure such as oral contraceptives, steroids, or hormone replacement therapy. None of them had a history of high blood pressure, evidence of any vascular disease, cerebrovascular accident, coronary artery disease, valvular heart disease, dysrhythmias, diabetes mellitus, heart failure or any other significant medical condition.
All measurements were made in the same temperature-controlled room (22 °C). Subjects gave informed consent and the study had institutional ethics committee permission.
Study protocol
All subjects were studied on 4 occasions on separate days within a 3-week period. Subjects were asked to avoid smoking, caffeine-containing drinks, chocolate/sweets and heavy exercise for 24 h preceding each study. The subjects rested, supine, for 10 min before baseline measurements of heart rate (HR/min), systolic blood pressure (BP, mm Hg), diastolic BP (mm Hg), pulse wave velocity (PWV, m/sec) and augmentation index (AIx, %) were made. The arterial stiffness indices were measured by The Arteriograph (TensioMed Ltd), a recently developed and validated computerized device using an oscillometric method to determine PWV and AIx.22,23 Oscillometric pressure curves (pulsatile pressure changes in the brachial artery) registered in the upper arm, are detected by plethysmography. Pulsatile changes in pressure in the artery beneath an inflated pressure cuff induce pressure changes in the cuff, which become an indirect measure for the pulsatile pressure changes in the artery beneath.22 The Arteriograph, which yields a simultaneous measure of brachial blood pressure (mmHg), PWV (m/sec) and AIx (%), has recently been validated against the Complior and the SphygmoCor, largely in a healthy population.22
Blood pressure measurements
Brachial blood pressure and heart rate were measured in the left arm with an automated digital oscillometric sphygmomanometer (Omron, Model HEM 705-CP, Omron Corporation). Three readings separated by 1-min intervals were taken; the mean was used for analysis. Peripheral pulse pressure was calculated as the difference between brachial systolic and diastolic BP.
Measures of arterial stiffness and wave reflection
At each visit, after resting in a supine position for 10 min in a quiet room, an Arteriograph measurement cuff was applied to the left upper arm; blood pressure (BP [mm Hg]), pulse wave velocity (PWV [m/sec]) and augmentation index (AIx [%]) were recorded with the computerized Arteriograph (TensioMed Ltd).
PWV (m/s) was calculated by dividing twice the distance between the supra-sternal notch and the symphysis pubis by the time interval between the beginning of the first wave and the beginning of the second (reflected) wave. The augmentation index was calculated as the pressure difference between the second (P2) and first (P1) systolic peaks of the arterial waveform divided by the (total) pulse pressure, expressed as a percentage. The Arteriograph gives the brachial AIx without applying a transfer function. The inflection point indicates the return of the reflected wave, which in turn provides a measure of the transit time to and from the aorto-iliac bifurcation, presumed to be the principal reflectance site.22
Maximal voluntary contraction
After baseline hemodynamic measurements, the Maximal Voluntary Contraction (MVC) was recorded using a calibrated hand-grip dynamometer (HK51020; Suncrea, Tokyo, Japan). To familiarize the subject and overcome learning phenomena, the MVC of the dominant hand was determined one day prior to the study, with the arm positioned at right angles and the elbow by the side of the body. The handle of the dynamometer was adjusted according to subject’s handedness. The base was made to rest on the first metacarpal (heel of palm), while the handle rested on the middle of four fingers. The subjects squeezed the dynamometer with maximum isometric effort twice, with a 2 min time interval, the larger of which was used to define the MVC. No other body movement was allowed and Valsalva maneuver was avoided to prevent the recruitment of accessory muscles.
Testing schedule
Baseline Arteriograph measurements were made at the beginning of each subsequent visit. On the first visit, the subjects maintained a hand grip at 30% of MVC; on the second visit, the subjects immersed their right hand in cold water at 3–4 °C; and on the third visit, they performed difficult mental arithmetic for 3 min while distracting by auditory stimuli took place in the background. Blood pressure and arterial stiffness indices were recorded serially on each visit: during the intervention and at 5 and 10 min after the end of the intervention.
Statistical analysis
All values are given as a mean and standard deviation (Mean ± SD) or percentage (%) and statistical analysis was carried out using JMP software (Version 7). Bivariate relationships were examined; Student’s t test and ANOVA were used to test the significance of mean differences between continuous variables. P < 0.05 was taken to be significant. Multivariate analysis then was performed to assess the difference in PWV and AIx during intervention, 5 and 10 min afterwards after correction for heart rate, systolic and diastolic blood pressure.
Results
Overall, the study comprised of 23 young, healthy, normotensive subjects with a mean age of 23 years (range 18–30 years); 14 were female. The subjects’ height was 171 ± 9 cm; weight, 68 ± 12 kg; hip circumference, 102 ± 7 cm; and waist, 78 ± 9 cm.
Maximal voluntary contraction
The baseline maximum voluntary contraction (MVC) was 34.8 ± 4 dyn; 30% of MVC was 10.4 ± 2.8 dyn. During 30% MVC testing there were significant increases from baseline in HR, systolic BP, diastolic BP and mean arterial pressure (P < 0.01). PWV was significantly increased from 6.7 ± 0.8 to 7.8 ± 0.8 m/sec (P < 0.01); and AIx −73 ± 12 to −51 ± 25. The values 5 min following and 10 min after 30% MVC were almost similar to as baseline as shown (Table 1 and Fig. 1(A and B). When the model was corrected for HR, systolic BP and diastolic BP the changes both in PWV and AIx remained significant (P < 0.001), see Table 2.
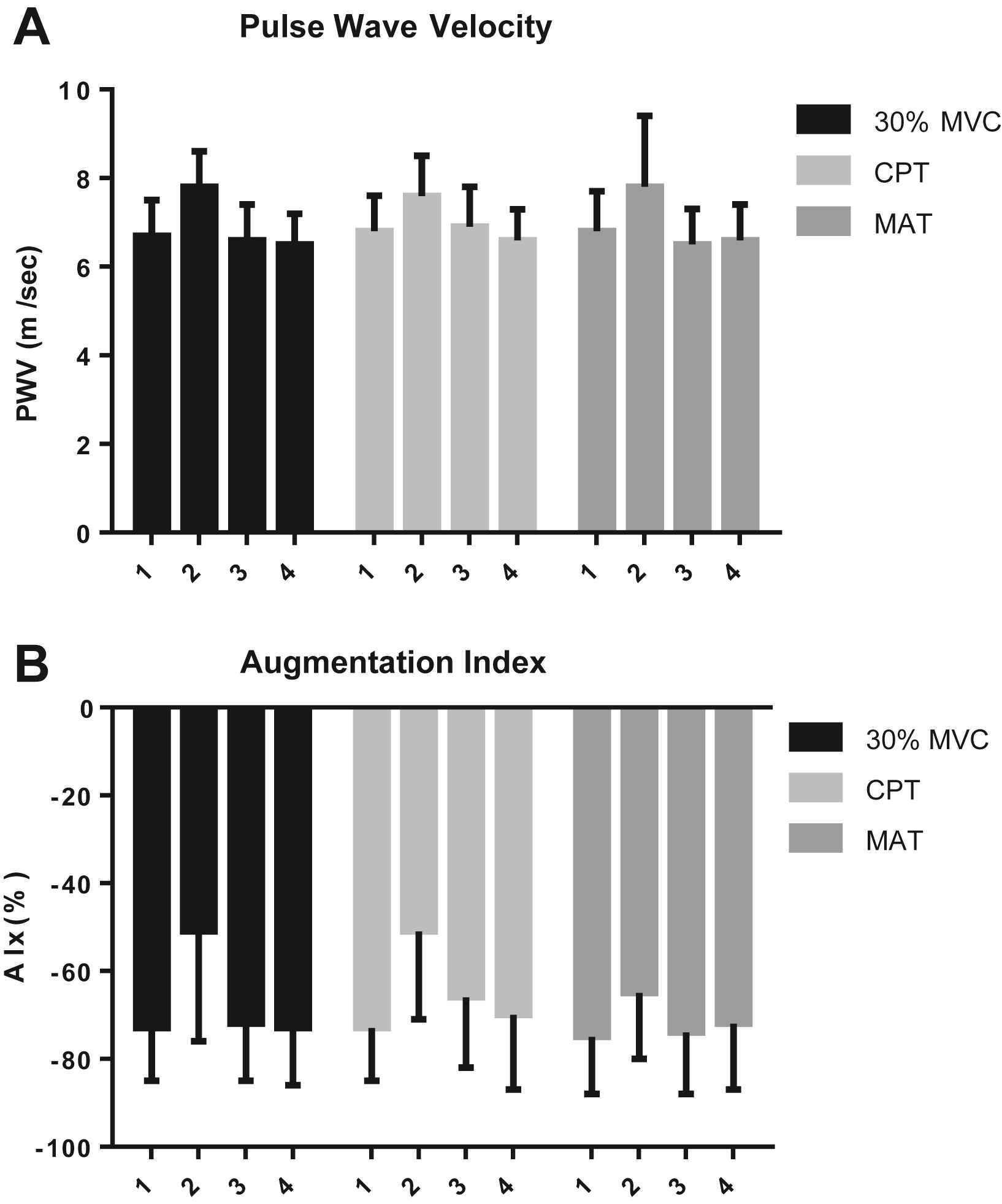
Changes in Pulse Wave Velocity (A) and Augmentation Index (B) with 30% Maximal Voluntary Contraction (MVC), Mental Arithmetic Test (MAT) and Cold Pressor Test (CPT). [1 = baseline, 2 = during test, 3 = 5 min post, and 4 = 10 min post].
| Baseline | During intervention | After 5 min | After 10 min | |
|---|---|---|---|---|
| 30% maximal voluntary contraction | ||||
| Heart rate (min−1) | 70 ± 12 | 77 ± 12 | 67 ± 11 | 68 ± 12 |
| Systolic BP (mmHg) | 112 ± 10 | 125 ± 14 | 113 ± 10 | 116 ± 12 |
| Diastolic BP (mmHg) | 65 ± 6 | 75 ± 6 | 66 ± 6 | 66 ± 6 |
| Pulse pressure (mmHg) | 47 ± 8 | 51 ± 9 | 46 ± 7 | 50 ± 11 |
| Mean arterial pressure (mmHg) | 81 ± 7 | 87 ± 20 | 82 ± 7 | 82 ± 7 |
| Augmentation index (%) | −73 ± 12 | −51 ± 25 | −72 ± 13 | −73 ± 13 |
| Pulse wave velocity (m/sec) | 6.7 ± 0.8 | 7.8 ± 0.8 | 6.6 ± 0.8 | 6.5 ± 0.7 |
| Cold pressor test | ||||
| Heart rate (min−1) | 67 ± 12 | 78 ± 13 | 66 ± 11 | 65 ± 10 |
| Systolic BP (mmHg) | 113 ± 10 | 132 ± 19 | 115 ± 11 | 116 ± 10 |
| Diastolic BP (mmHg) | 65 ± 5 | 80 ± 8 | 68 ± 8 | 67 ± 7 |
| Pulse pressure (mmHg) | 48 ± 8 | 52 ± 12 | 47 ± 7 | 48 ± 8 |
| Mean arterial pressure (mmHg) | 81 ± 6 | 96 ± 9 | 83 ± 9 | 83 ± 7 |
| Augmentation index (%) | −73 ± 12 | −51 ± 20 | −66 ± 16 | −70 ± 17 |
| Pulse wave Velocity (m/sec) | 6.8 ± 0.8 | 7.6 ± 0.9 | 6.9 ± 0.9 | 6.6 ± 0.7 |
| Mental arithmetic test | ||||
| Heart rate (min−1) | 70 ± 12 | 89 ± 17 | 69 ± 11 | 68 ± 10 |
| Systolic BP (mmHg) | 116 ± 12 | 134 ± 17 | 117 ± 11 | 116 ± 10 |
| Diastolic BP (mmHg) | 67 ± 6 | 77 ± 8 | 67 ± 6 | 67 ± 6 |
| Pulse pressure (mmHg) | 49 ± 9 | 58 ± 13 | 50 ± 9 | 49 ± 9 |
| Mean arterial pressure (mmHg) | 83 ± 8 | 96 ± 10 | 83 ± 7 | 83 ± 6 |
| Augmentation index (%) | −75 ± 13 | −65 ± 15 | −74 ± 14 | −72 ± 15 |
| Pulse wave velocity (m/sec) | 6.8 ± 0.9 | 7.8 ± 1.6 | 6.5 ± 0.8 | 6.6 ± 0.8 |
Haemodynamic measurements in normal healthy subjects: 30% maximal voluntary contraction, cold pressor test and mental arithmetic test (n = 23, Mean ± SD).
Cold pressor test
CPT reactivity was examined after baseline measurements, significant increase from baseline in HR, systolic BP, diastolic BP, and mean arterial pressure (P < 0.01). PWV was significantly increased from 6.8 ± 0.8 to 7.6 ± 0.9 m/sec (P < 0.01) and Alx, from −73 ± 12 to −51 ± 20 (P < 0.001). At 5 and 10 min after CPT, values returned almost similar to baseline as shown (Table 1 and Fig. 1A and B). When the model was corrected for HR, systolic BP and diastolic BP the changes both in PWV and AIx remained significant (P < 0.001), see Table 2.
| Model | Model | During intervention | After 5-min | After 10-min | P ANOVA |
|---|---|---|---|---|---|
| Model 1 corrected with heart rate | |||||
| PWV (m/sec) | 30% Maximal voluntary contraction | 7.75 (7.44–8.07) | 6.65 (6.33–6.98) | 6.55 (6.22–6.88) | <0.0001 |
| Cold pressor test | 7.68 (7.31–8.04) | 6.9 (6.48–7.31) | 6.67 (6.27–7.06) | =0.0009 | |
| Mental arithmetic test | 7.89 (7.45–8.34) | 6.53 (6.01–7.05) | 6.66 (6.15–7.17) | =0.0001 | |
| AIx (%) | 30% Maximal voluntary contraction | −51.04 (58.47 to −43.62) | −72.19 (−79.95 to −64.42) | −73.62 (−81.38 to −65.87) | <0.0001 |
| Cold pressor test | −50.68 (−57.5 to −43.87) | −66.16 (−73.96 to −58.35) | −69.64 (−77.08 to −62.2) | =0.0007 | |
| Mental arithmetic test | −65.51 (−71.03 to −59.98) | −74.92 (−81.37 to −68.46) | −72.04 (−78.74 to −66.07) | =0.0722 | |
| Model 2 corrected with mean arterial pressure | |||||
| PWV (m/sec) | 30% Maximal voluntary contraction | 7.8 (7.47–8.12) | 6.64 (6.31–6.98) | 6.57 (6.23–6.9) | <0.0001 |
| Cold pressor test | 7.0.67 (7.32–8.02) | 6.87 (6.47–7.27) | 6.64 (6.26–7.02) | =0.0004 | |
| Mental arithmetic test | 7.81 (7.35–8.27) | 6.51 (6.01–7.02) | 6.64 (6.14–7.13) | =0.0004 | |
| AIx (%) | 30% Maximal voluntary contraction | −48.06 (−56.22 to −40.99) | −71.9 (−79.75 to −64.04) | −72.94 (−80.79 to −65.08) | <0.0001 |
| Cold pressor test | −49.46 (−56.59 to −42.33) | −65.34 (−73.45 to −57.24) | −69.41 (−77.13 to −61.68) | 0.0007 | |
| Mental arithmetic test | −64.62 (−70.52 to −58.71 | −74.2 (−80.67 to −67.72) | −71.7 (−78.02 to −65.37) | =0.0795 | |
| Model 3 corrected with systolic blood pressure | |||||
| PWV (m/sec) | 30% Maximal voluntary contraction | 7.77 (7.45–8.09) | 6.64 (6.31–6.98) | 6.57 (6.24–6.9) | <0.0001 |
| Cold pressor test | 7.65 (7.29–8.01) | 6.86 (6.46–7.26) | 6.63 (6.26–7.01) | =0.0006 | |
| Mental arithmetic test | 7.8 (7.34–8.26) | 6.51 (6–7.02) | 6.64 (6.15–7.13) | =0.0004 | |
| AIx (%) | 30% Maximal voluntary contraction | −50.11 (57.73 to −42.49) | −72.13 (−80.17 to −64.1) | −73.3 (−81.24 to −65.36) | <0.0001 |
| Cold pressor test | −49.09 (−56.43 to −41.75) | −65.62 (−73.71 to −57.54) | −69.62 (−77.32 to −61.93) | =0.0006 | |
| Mental arithmetic test | −64.78 (−70.63 to −58.94) | −74.51 (−80.94 to −68.08) | −71.93 (−78.21 to −65.64) | =0.071 | |
| Model 4 corrected with diastolic blood pressure | |||||
| PWV (m/sec) | 30% Maximal voluntary contraction | 7.77 (7.45–8.09) | 6.64 (6.31–6.98) | 6.56 (6.23–6.9) | <0.0001 |
| Cold pressor test | 7.0.67 (7.32–8.02) | 6.88 (6.48–7.28) | 6.64 (6.26–7.03) | =0.0005 | |
| Mental arithmetic test | 7.81 (7.35–8.28) | 6.51 (6–7.02) | 6.63 (6.14–7.13) | =0.003 | |
| AIx (%) | 30% Maximal voluntary contraction | −50.05 (−57.68 to −42.41) | −71.69 (−79.8 to −63.59) | −72.5 (−80.61 to −64.38) | <0.0001 |
| Cold pressor test | −49.26 (−56.38 to −42.15) | −65.09 (−73.22 to −56.96) | −69.27 (−77.03 to −61.51) | =0.0007 | |
| Mental arithmetic test | −64.46 (−70.42 to −58.5 | −73.88 (−80.41 to −67.35) | −71.49 (−77.86 to −65.11) | =0.0887 | |
PWV and AIx in MCV (30%), CPT and MAT (mean 95% CI).
Mental arithmetic test
During MAT there was a significant increase from baseline in HR, systolic BP, diastolic BP, and mean arterial pressure (P < 0.01). PWV was significantly increased from 6.8 ± 0.9 to 7.8 ± 1.6 m/sec, (P < 0.05) and AIx, from −75 ± 13 to −65 ± 15% (P < 0.05). At 5 and 10 min after the MAT, values returned almost similar to baseline as shown (Table 1 and Fig. 1A and B). When the model was corrected for HR, systolic BP and diastolic BP the changes in PWV (P < 0.001), remained significant and AIx (P = 0.09), see Table 2.
Discussion
The main finding of the present study is that an acute response to mental stress, the cold pressor test and hand-grip isometric exercise is noted, not only on heart rate and blood pressure but also on PWV and AIx in healthy individuals.
It is well known that in the cardiovascular system, the aorta and large arteries are both conduits and buffering organs. The aorta buffers the pressure changes resulting from intermittent ejection of blood into the aorta by the left ventricle. Its elastic wall absorbs a fraction of this energy during systole and releases it during diastole, thereby enhancing coronary blood flow and limiting the increase in left ventricular afterload. Pressure waves are reflected back from the periphery of the circulation and summate with the forward-going wave to produce a characteristic aortic pressure waveform. Normally, reflected waves return during diastole, further enhancing coronary blood flow, but not affecting aortic systolic pressure. However, with aortic and large-vessel stiffening, the pulse wave travels more rapidly and the amplitude of reflected wave increases such that reflected waves now arrive earlier, during systole. This increases left ventricular afterload.
MAT is a validated and widely used test able to induce a considerable degree of perceived stress.24 Previous studies have indicated the effect of MAT in arterial stiffness.1,24,29 One of the mechanisms proposed is the catecholamine release, i.e. epinephrine, norepinephrine and dopamine. Also acute mental stress can induce endothelial dysfunction which in turn is proven to cause increase arterial stiffness.28,29 Furthermore, it has been demonstrated that acute mental stress leads to immune activation and inflammation, which is also linked to increased arterial stiffness indices.18
CPT has been linked with increase arterial stiffness in previous studies.30,31 The response of conduit arteries to systemic cold may be the result of the balance between adrenergic vasoconstriction and vasodilatation, with the latter being mediated by endothelial function. Being modulated by activation of the sympathetic nervous system, vasoconstriction is thus also related to the level of catecholamines in the blood.30,31 In the present study we managed to demonstrate that CPT can cause significant increase in PWV and AIX which can be explained by the above proposed mechanism.
The effect of MVC on AIx was previously assessed demonstrating an increase in arterial stiffness.32 In our study arterial stiffness was increase acutely after MVC performed and returned to normal levels 10 min after the test clearly demonstrating the acute effect of static dynamic exercise on vascular hemodynamics.
To our knowledge this is the first study demonstrating the effect of MVC, CPT and MAT on arterial stiffness indices, both PWV and AIx in a cohort of young normotensive individuals. Further, it has been noted that those changes in an acute setting were independent of blood pressure and heart rate effect pointing to a possible direct pathophysiologic mechanism linking stress to arterial stiffness. Further studies need to be conducted for the enlightening of the mechanisms involved.
Conclusions
We found evidence of an acute effect of mental stress, cold pressor and maximal voluntary contraction on arterial stiffness indices and they are independent of blood pressure changes. This emphasizes the importance of room temperature and relaxation of both muscles and mind when measuring arterial stiffness.
Acknowledgment
This work was done under supervision of the late Professor John Feely, Head Department of Clinical Pharmacology & Therapeutics, Trinity College Dublin & Hypertension Clinic St James’s Hospital Dublin, IRELAND.
References
Cite this article
TY - JOUR AU - Noor-Ahmed Jatoi AU - Stella-Maria Kyvelou AU - John Feely PY - 2014 DA - 2014/03/20 TI - The acute effects of mental arithmetic, cold pressor and maximal voluntary contraction on arterial stiffness in young healthy subjects JO - Artery Research SP - 44 EP - 50 VL - 8 IS - 2 SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2014.02.002 DO - 10.1016/j.artres.2014.02.002 ID - Jatoi2014 ER -
