Comparison of simultaneous invasive and non-invasive measurements of blood pressure based upon MIMIC II database
- DOI
- 10.1016/j.artres.2014.07.001How to use a DOI?
- Keywords
- Invasive blood pressure; Non-invasive blood pressure; MIMIC II database
- Abstract
Objective: To compare the simultaneous invasive and non-invasive measurements of blood pressure (IBP and NIBP) based upon the Multiparameter Intelligent Monitoring in Intensive Care II (MIMIC II) database.
Methods and results: A total of 986 records and 26,942 blood pressure (BP) measurements were extracted from MIMIC II database. The mean values of invasive systolic and invasive diastolic blood pressure (ISBP and IDBP) were 111.2 ± 33.9 mm Hg and 59.9 ± 22.8 mm Hg respectively, and the values of non-invasive ones were 114.0 ± 23.4 mm Hg and 51.0 ± 14.9 mm Hg. The average differences of systolic and diastolic blood pressure were −2.8 mm Hg and 8.9 mm Hg between IBP and NIBP. The correlation coefficients were 0.60 between ISBP and NISBP and 0.45 between IDBP and NIDBP. The robust regression equations between IBP (y) and NIBP (x) showed y = 1.02x − 2.95 for SBP (R2 = 0.60) and y = 0.77x + 18.43 for DBP (R2 = 0.82). At the higher part of BP, IBP is larger than NIBP, and at the lower part of BP, IBP is less than NIBP.
Conclusion: Average invasive systolic blood pressure is lower than the non-invasive one and average invasive diastolic blood pressure is higher than the non-invasive one. The IBP shows good correlation with the NIBP. The invasive blood pressures can be estimated from non-invasive ones by the regression equations.
- Copyright
- © 2014 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
Arterial blood pressure (BP), which can be measured by invasive or non-invasive procedures, is defined as the pressure exerted by circulating blood upon the arterial walls. Most of time, the measurements are somewhat different between these two methods. Non-invasive measurement is extensively used in the routine examinations and monitoring with the advantage of simplicity and safety. Invasive measurements are mainly used as golden criteria in animal experiments and critical care. Understandably, the catheter used for intra-arterial measurement can sense the tiny pulses of blood flow and perceive sensitively the tiny beat-by-beat changes of hemodynamics. A large number of patients have profited from the high accuracy and sensitivity of the invasive blood pressure measurement.1,2
Many studies have been done to compare the accordance between invasive and non-invasive blood pressure in animal experiments,3–9 human researches10,11 and intensive care units.12,13 However, most of the previous studies reached the conclusions based on small populations and small amount of pairing BP data in animal experiments or human researches.
At present, the dynamical and simultaneous differences between invasive BP (IBP) and non-invasive BP (NIBP), the attributions of IBP–NIBP differences to the arterial stiffness and the derivation of IBP from NIBP greatly intrigue us. In this study, we attempted to compare the pairing data of IBP and NIBP based on a large population from Multiparameter Intelligent Monitoring in Intensive Care II (MIMIC II) database.14,15
Materials and methods
The public-access MIMIC II database was set up by Laboratory for Computational Physiology at the Massachusetts Institute of Technology (http://physionet.org).16 The inclusive data were collected over a seven year period beginning in 2001 from Boston’s Beth Israel Deaconess Medical Center, covering any patients admitted to the medical, surgical, coronary and cardiac surgery care units for the adult patients aged over 15 years old and any babies into neonatal ICU. Databases were collected online over TCP/IP. In the database, noninvasive BPs of the patient were measured by oscillometric method with brachial sphygmomanometer cuff and displayed and recorded by the monitoring device. At the same time, invasive BPs were measured routinely at the same arm with an arterial catheter placed into the radial artery and recorded synchronously. Invasive and non-invasive BP data were stored in numeric records. In our study, the MIMIC II Waveform Database Matched Subset was used, including 4897 waveform records and 5266 numerics records. By reviewed the total numerics records, 986 records contain simultaneous IBP and NIBP measurements. To remove the transient noise in the IBP signals, a 5 points median filter for data saved in 1 min interval or a 30 points median filter for data saved in 1 s interval was used. Since the NIBP measurement was performed discretely in time, only the IBP points with corresponding NIBP points were selected. Thus a total of 26,942 IBP/NIBP pairs were included in this study.
The data of systolic BP (SBP) and diastolic BP (DBP) were expressed in mean ± standard deviation (SD). The paired students’ t test was adopted to compare the paring IBP and NIBP with IBM SPSS 19.0 software. Two-tailed Pearson bivariate correlation analysis, linear regression and robust regression with Matlab 2010b were applied to calculate the correlation coefficients and linear regression equations. In addition, Bland and Altman method was used to contrast IBP–NIBP differences with mean values of IBP and NIBP.17
Results
The mean values of invasive systolic and invasive diastolic blood pressure (ISBP and IDBP) were 111.2 ± 33.9 mm Hg and 59.9 ± 22.8 mm Hg respectively, and the values of non-invasive ones were 114.0 ± 23.4 mm Hg and 51.0 ± 14.9 mm Hg. The average differences of systolic and diastolic blood pressure were −2.8 ± 27.2 mm Hg and 8.9 ± 20.9 mm Hg between IBP and NIBP with the statistical significance (P < 0.001).
The correlation coefficients (r) were 0.60 between ISBP and NISBP and 0.45 between IDBP and NIDBP. The linear regression equations between IBP (y) and NIBP (x) showed y = 0.87x + 11.70 for SBP (R2 = 0.36) and y = 0.69x + 24.74 for DBP (R2 = 0.20). However, the Pearson correlation coefficients and the linear regression are highly sensitive to outliers. The robust regression showed more correlative as y = 1.02x − 2.95 for SBP (R2 = 0.60) and y = 0.77x + 18.43 for DBP (R2 = 0.82) (Fig. 1).
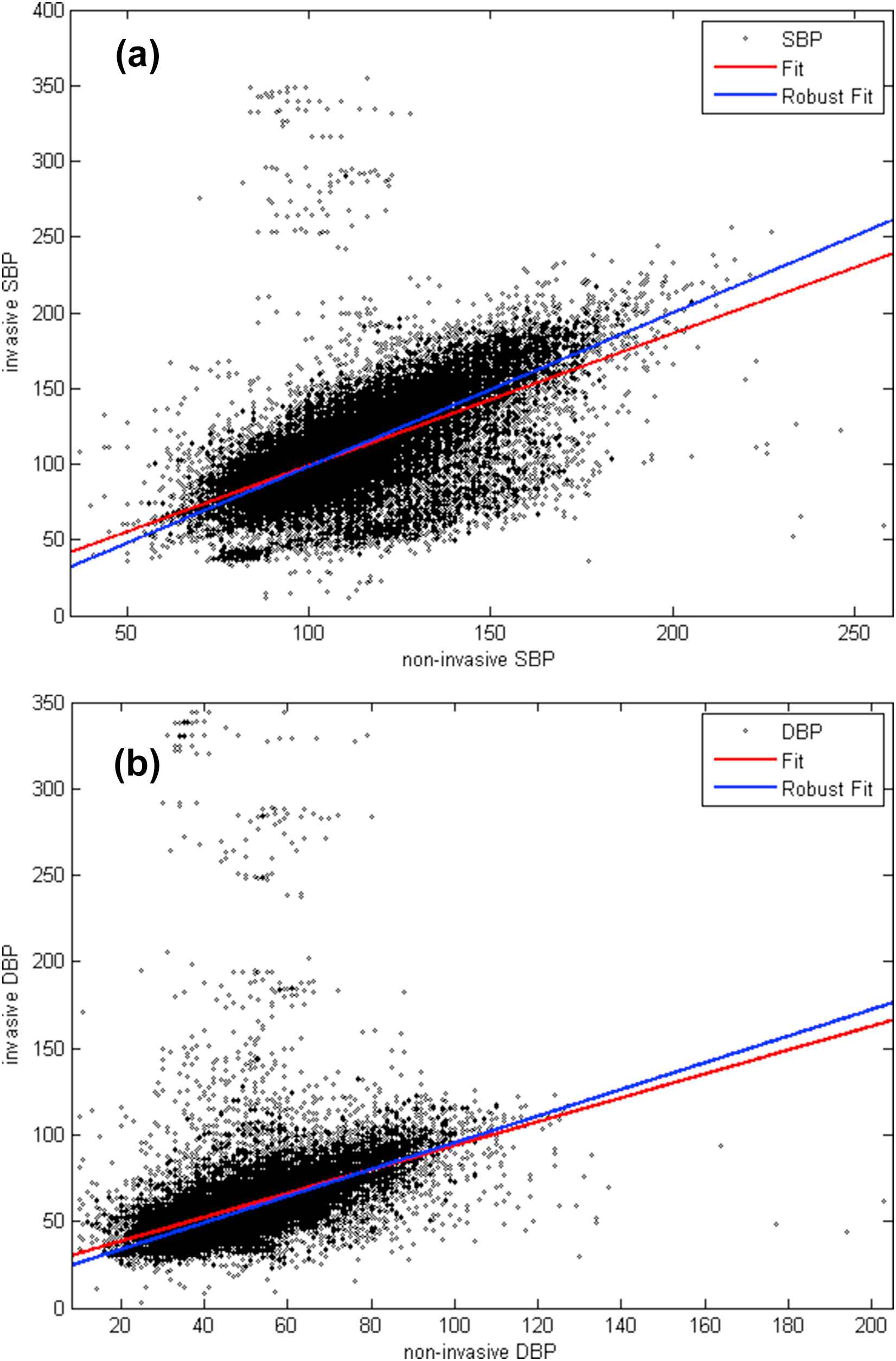
Comparison of non-invasive BP and invasive BP. (a) Comparison of non-invasive SBP and invasive SBP, (b) Comparison of non-invasive DBP and invasive DBP.
The Bland and Altman plots were shown in Fig. 2, in which the differences between invasive and non-invasive BP were plotted against their average values of invasive and non-invasive BP with correlation coefficients of 0.35 and 0.03, intercepts of −39.80 and 5.42 and robust regression R2 of 0.51 and 0.77 for SBP and DBP respectively. This clearly showed that at the higher part of BP, IBP is larger than NIBP, and at the lower part of BP, IBP is less than NIBP.
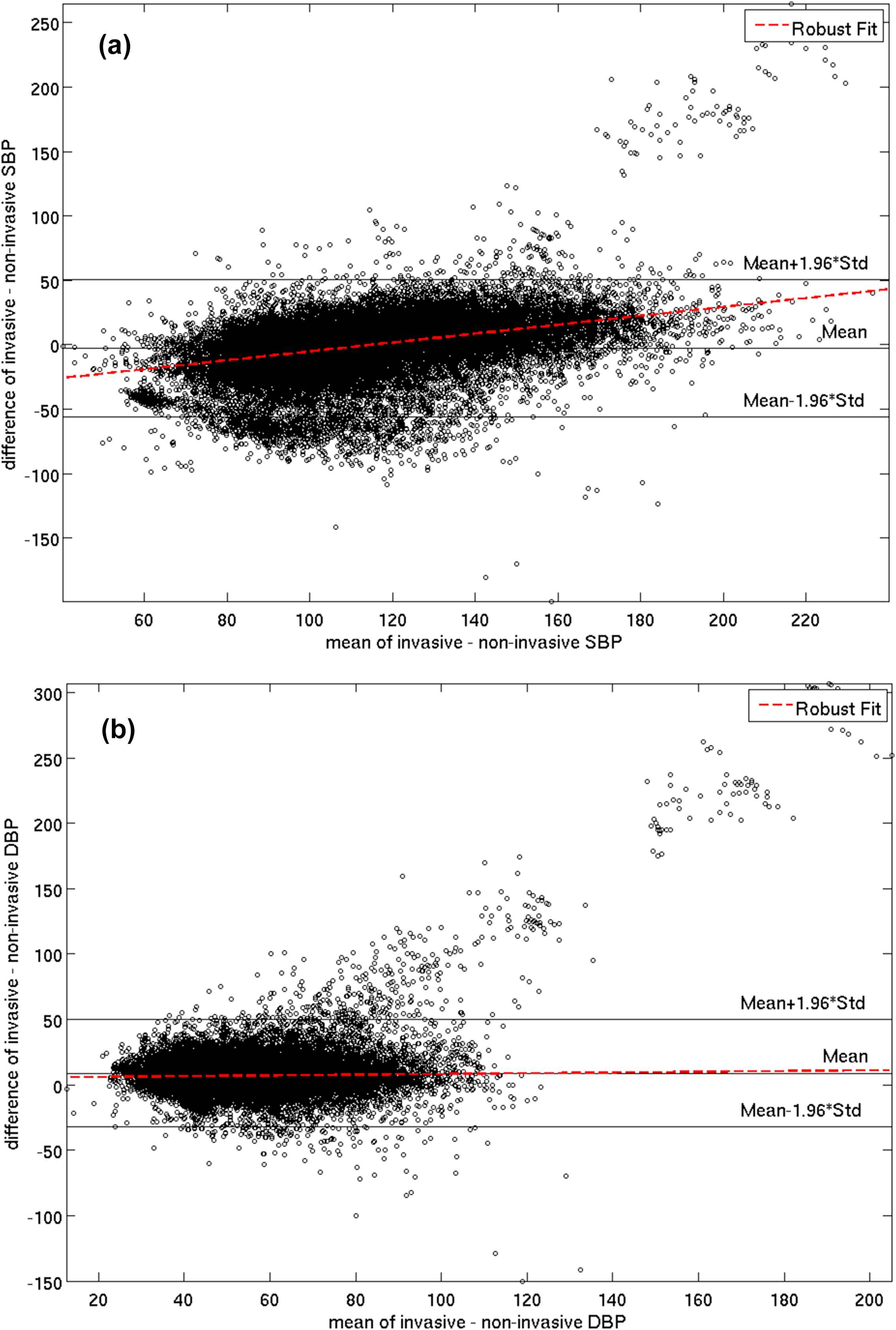
Bland–Altman plot of invasive–non-invasive BP difference versus mean BP. (a) Bland–Altman plot of invasive–non-invasive SBP difference versus mean SBP, (b) Bland–Altman plot of invasive–non-invasive DBP difference versus mean DBP.
Discussion
Many researches have shown the conflicting data regarding the discrepancy of invasive and non-invasive BP. Hodgkin et al. (1982) compared direct BP measurements to non-invasive cuff BP monitored via Doppler ultrasound at the leg distal to the elbow, getting 0.94 and 0.88 of correlation coefficients for SBP and DBP and the regression coefficients less than 1 and the intercepts greater than 0.3 Cuff DBP was slightly lower than direct DBP, while only SBP over 200 mm Hg was underestimated. Cimini and Zambraski (1985) studied normotensive and hypertensive pigs to find consistently low readings (17%) for cuff DBP relative to intra-arterial DBP. SBP were closer between the two techniques with good correlation (r = 0.95).4 Cruz et al. (1998) also found that the cuff method gave readings consistently 18–21 mm Hg below the direct measurement.5 Knaevelstrud and Framstad (1992) studied direct pressure measurements to an oscillometric cuff in pigs.6 The observed regression coefficients were less than 1 and the intercepts were greater than 0. Moreover, BP readings for the cuff were consistently below those for the direct measurement. Correlation coefficients for SBP, MBP and DBP were 0.91, 0.93 and 0.95 respectively. Therefore, it can be concluded that IDBP is higher than NIDBP, whereas ISBP may be higher, similar or lower than NISBP in pigs.
Bode et al. (1996) researched on oscillometric measurements and direct catheter measurements in seven dogs.7 The differences between the direct and indirect values were greatest at high pressures, with the bias of SBP bigger than DBP. Chow et al. (1999) detected systemic bias at extreme hypertension and hypotension via the method of Bland and Altman, showing that the cuff gave higher readings at low blood pressures and lower readings at high blood pressures.8 Gladczak et al. (2013) compared direct measurements via catheterization to indirect sphygmomanometer measurements in pigs and found cuff SBP was higher than SBP for arterial measurements, while cuff DBP was lower than arterial. Furthermore, a Bland–Altman analysis confirmed this bias at the extremes of the normotensive range.9 Obviously, there are bigger deviations between IBPs and NIBPs towards extreme hypertension and hypotension in animals.
Wiecek et al. (1990) compared brachial artery catheter BP and sphygmomanometry BP at rest, during leg lifting and during 2 min of recovery after lifting with the arms and legs.10 Indirect SBP at rest was 13% less than those recorded directly (130 ± 7 mm Hg vs 149 ± 8 mm Hg); DBP was similar using either method. Broadhurst et al. (1990) performed 24-h intra-arterial ambulatory BP monitoring in 50 normal volunteers (cuff BP < 140/90 mm Hg) and defined the upper limit of normal daytime BP in both men and women as 150/90 mm Hg and the upper limit of mean nighttime BP as 130/80 mm Hg for men and 115/65 mm Hg for women.11 Brown et al. (1994) compared intra-arterial and mercury sphygmomanometry BP in 28 pregnant women and assessed interobserver variability in a separate study of 86 pregnant women.12 Sphygmomanometry underestimated direct SBP by average 11 mm Hg. Phase IV Korotkoff sound overestimated direct DBP by average 9 mm Hg and phase V by average 4 mm Hg. They concluded that auscultatory sphygmomanometry in pregnant women underestimated SBP and overestimates DBP. Lalan et al. (2013) studied 1492 simultaneous oscillometric and intra-arterial (umbilical arterial or radial arterial) BP measurements from 101 neonates for comparison.13 Total 125,580 5-min averaged intra-arterial BP readings were used to evaluate BP distribution. Oscillometric radial MBP valued 4.8 ± 9.8, SBP 8.3 ± 11.6, DBP 4.3 ± 9.3 (mm Hg) and difference between oscillometric and umbilical arterial SBP numbered 5.2 ± 11.9 mm Hg and DBP - 0.8 ± 10.4 mm Hg.
Usually, invasive SBP is higher than non-invasive SBP, and invasive DBP is similar to or lower than non-invasive DBP in the above studies. However, our results show that ISBP is a little lower than NISBP, whereas, IDBP is bigger than NIDBP.
The reasons for that may be because of the effect of elasticity of arterial walls and the measurement methods. SBP can be accurately measured whatever in invasive ways or non-invasive ways. However, non-invasive SBP is read after occluding the arterial lumens completely with external pressure which induce two main forces outwards, lateral pressures exerted on arterial walls by blood flow plus elasticity of arterial walls. Therefore, NISBP is higher than ISBP. Their deviation is mainly determined by biological properties of arterial walls. On the other hand, ISBP-NISBP difference can be considered as a good parameter to arterial stiffness. Of course, this need further verification. Because accurate DBP is measured after arterial wall is relaxed completely and arterial lumen is opened completely, the confounding factors to produce IDBP-NIDBP deviations may be mainly from the measurement methods. First of all, invasive DBP is the most accurate to detect the intra-arterial minimum BP value. However, the non-uniform evaluations of DBP are the resource of bias in non-invasive measurements by human ears or equipments.
Borow et al. (1982) compared oscillometric brachial BP with simultaneous central aortic pressure measurements in 30 patients undergoing cardiac catheterization.18 Central aortic pressures ranged widely for SBP (98–177 mm Hg), DBP (41–97 mm Hg), and MBP (60–120 mm Hg). The oscillometric method provided accurate, reproducible, and convenient estimates of central aortic SBP and DBP and might be particularly useful when indirect blood pressure measurements were required for the noninvasive assessment of left ventricular function in patients without aortic stenosis. Chen et al. (2013) reviewed systemically the estimation of central blood pressure with non-invasive methods based on applanation tonometry, and concluded that present tonometry-based central BP estimating methods were acceptable in theory with small errors but there was substantial room for improvement in measurement accuracy of central BP when cuff BP is used to calibrate the peripheral waveforms.19 Derivation of IBP from NIBP is not only useful in estimation of central blood pressure; it is more useful in monitoring critically ill patients. In our study, regression equations were set up to estimate IBP from NIBP.
The invasive measurements showed large scatter up to 350 mm Hg in our study. It is obvious that the pairs of values which invasive measurements are around 300 mm Hg and non-invasive measurements are around 100 mm Hg are outliers. As per our understanding the outliers are caused by the noise during invasive blood pressure measurements. Although median filter was used to minimize the affect of noise, there were still outliers detected. When we calculated the Pearson correlation coefficients or the linear regression, these outliers biased the results and caused a lower correlative between invasive and non-invasive measurements (r = 0.60 and 0.45 or R2 = 0.36 and 0.20 for SBP and DBP). The robust regression used iteratively reweighted least squares with a bisquare weighting function, which gives coefficient estimates that are approximately 95% as statistically efficient as the ordinary least-squares estimates, provided the response has a normal distribution so as to get rid of the outliers.
In conclusion, our study shows that average ISBP is lower than NISBP and average IDBP is higher than NIDBP. The IBP shows good correlation with the NIBP. The invasive blood pressures can be estimated from non-invasive ones by the regression equations. The difference between invasive and non-invasive SBP may be a good index to reflect arterial stiffness.
Conflicts of interest
None.
References
Cite this article
TY - JOUR AU - Bing Liu AU - Peng Qiu AU - Hong Chen AU - Qiao Li PY - 2014 DA - 2014/08/15 TI - Comparison of simultaneous invasive and non-invasive measurements of blood pressure based upon MIMIC II database JO - Artery Research SP - 209 EP - 213 VL - 8 IS - 4 SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2014.07.001 DO - 10.1016/j.artres.2014.07.001 ID - Liu2014 ER -
