Epidemiological and Clinical Aspects of Scorpion Envenomation in Machacalis, Minas Gerais, Brazil, from 2016 to 2017
- DOI
- 10.2991/dsahmj.k.200903.002How to use a DOI?
- Keywords
- Tityus serrulatus; scorpion sting; injuries; envenomation; prevalence
- Abstract
Scorpion envenomation is a serious public health problem in tropical regions due to its high frequency and severity. This research aimed to estimate the prevalence of human cases of scorpion stings reported at Cura D’ars Hospital, Machacalis, Brazil, between 2016 and 2017, in addition to identifying the epidemiological and clinical aspects. This was a descriptive and retrospective study, using the database of the Information System for Notifiable Diseases in Brazil as a reference. Of the five municipalities evaluated, Machacalis had the highest number of cases, although Bertópolis recorded the highest prevalence. A total of 84 cases of scorpion stings were identified, corresponding to 91% of all cases of involvement with poisonous animals. Regarding the sociodemographic profile, the proportion was higher in males (52.0%), people with brown skin (67.0%), people aged 7–14 years (26.0%), and people from rural areas (68.0%). Regarding the epidemiological characteristics, 50.0% of the individuals were assisted between 1 and 3 h after the sting. The main anatomical region affected was the hand (26.0%), and 30.0% used specific serotherapy. For cases classified clinically according to severity, 70.2% were mild, 21.5% moderate, and 8.3% severe. The study allowed us to establish the profile of the victims of scorpion envenomation treated in this area of hospital coverage, as well as to evaluate the approach of the health teams in response to the demand that this neglected condition imposes.
- Copyright
- © 2020 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
In Brazil, epidemiological surveillance of scorpion envenomation is performed passively, in the form of registration in the Ministry of Health Information System for Notifiable Diseases [1]. This system makes it mandatory to notify all injuries caused by poisonous animals, providing access to information to subsidize public health agencies in the distribution of the specific antidote and the respective attendance for the injured [2]. Nevertheless, data from the Ministry itself show that, between 2016 and 2017, there was a marked increase in accidents with scorpions (from 91,476 to 124,077), making a total of 215,553 cases and 263 deaths [3].
Currently, scorpion sting is the main cause of poison-related injury in humans in Brazil. The scorpions of medical importance in the country belong to the Tityus genus, which is the richest in species, representing about 60% of the neotropical scorpion fauna. Tityus serrulatus is found in the south, southeast, and northeast regions of the country, and is responsible for one of the main external causes of hospitalization due to the frequency and severity with which it occurs, especially when the victims are children and elderly people [4].
The venom of T. serrulatus is mainly composed of neurotoxins and is a source of different classes of peptides that affect the normal function of ion channels. The inoculation of the crude poison or some purified fractions causes local pain and complex effects on the sodium channels, producing depolarization of the postganglionic nerve endings, with the release of catecholamines and acetylcholine [4]. The severity of the poisoning is directly related to the amount of inoculated venom and the chemical mediators released. These mediators determine the onset of general organic, digestive, cardiovascular, respiratory, and neurological manifestations resulting from the predominance of sympathetic or parasympathetic effects [5].
In 2009, the high number of scorpion envenomations in tropical countries led the World Health Organization to include them in the list of Neglected Tropical Diseases (NTDs). As the majority of the population affected by this condition have little political influence, NTDs have a low impact on public health policy priorities. This implies low investments in research and prevention, and fragility of the epidemiological information flow that reinforce the perpetuation of conditions of poverty and low health conditions [6].
Studies that address the pattern of occurrence of these types of injuries and their epidemiological characteristics are necessary, since they support the understanding of the dynamics of these injuries, as well as to promote important health surveillance actions [7,8]. The state of Minas Gerais is the Brazilian state that has the highest rate of prevalence of this condition, and most of the studies carried out so far that address this issue come from the metropolitan region of Belo Horizonte [9,10] and other large cities in the state [11–14]. The present study is believed to be the first to describe the epidemiological and clinical profile of this neglected condition throughout the northeast region of Minas Gerais.
The relevance of this study is based on the need to identify the epidemiological and clinical profile of victims of scorpion stings admitted to a hospital reference center in the municipality of Machacalis, given the high number of occurrences and the importance of creating more qualified support strategies for professionals who serve this population, enabling the optimization of time for the adoption of appropriate emergency measures, therefore reducing the morbidity and mortality of victims in the municipalities that comprise the studied region.
2. MATERIALS AND METHODS
This was a descriptive and retrospective study, with a quantitative approach, using as a reference the database of the Information System for Notifiable Diseases of the Ministry of Health of Brazil. We included people of both sexes and ages who were victims of scorpion stings between January 2016 and December 2017, treated at the Cura D’ars Hospital, Machacalis, Mucuri Valley, Minas Gerais, Brazil.
The Cura D’ars hospital is strategically located in the city of Machacalis and has 52 beds. It is an important hospital reference center that provides urgent and emergency medical care to the municipalities of Bertópolis, Fronteira dos Vales, Machacalis, Santa Helena de Minas and Umburatiba, covering a population of approximately 25,747 inhabitants [15] (Figure 1).
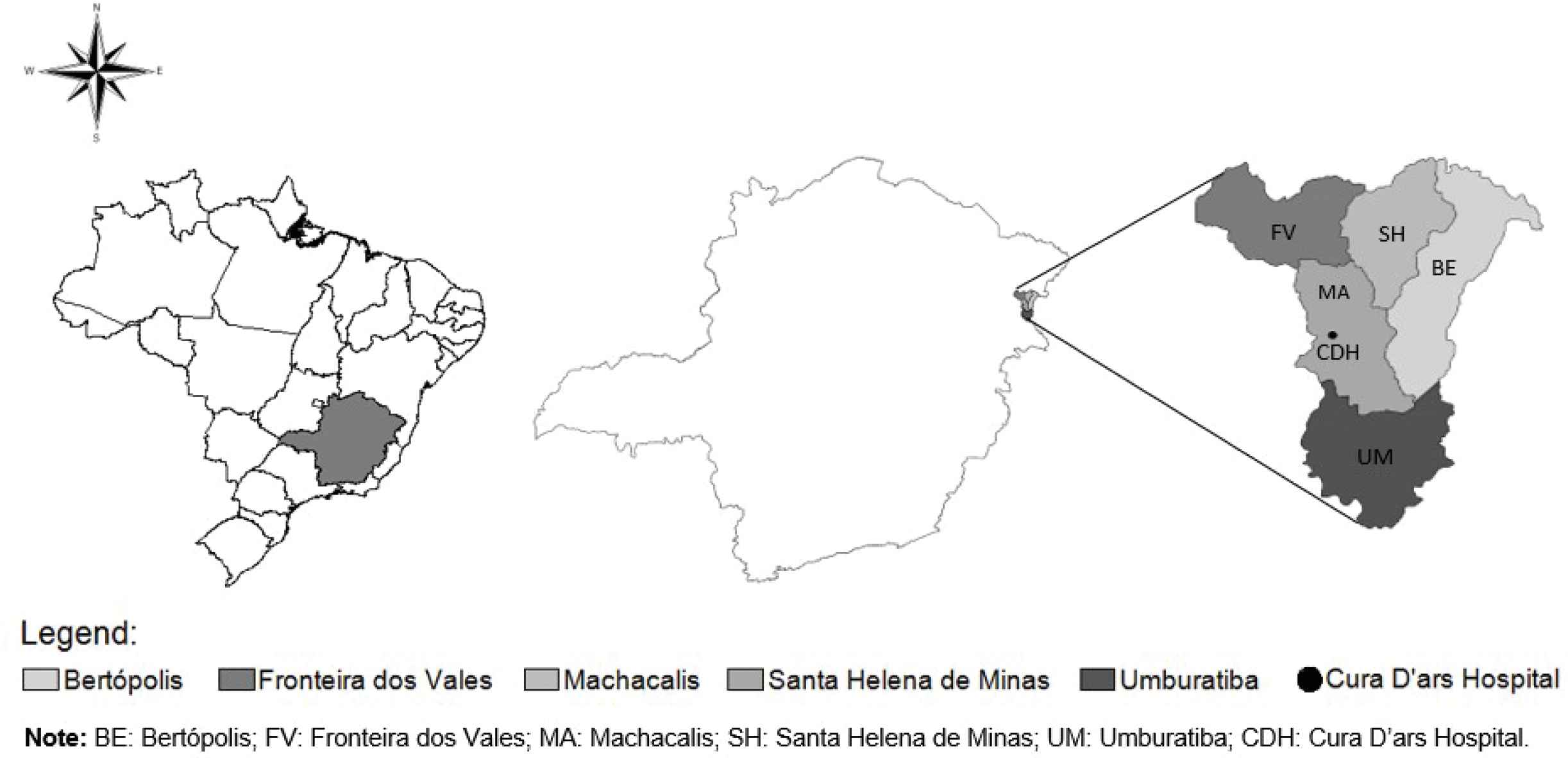
Map of the state of Minas Gerais and the Brazilian territory identifying the municipalities that comprise the coverage area of Cura D’ars Hospital, city of Machacalis.
The municipality of Machacalis is located in the northeastern region of the state of Minas Gerais, 847 km from its capital, at 17°04′38″ latitude south and 40°42′59″ west longitude, at an average altitude 271 m above sea level. The municipality has an area of 332 km², with a population of 7,228 inhabitants, and a demographic density of 21.85 per km2. The characteristic climate of the region is tropical, with an annual average temperature of 25°C and an annual rainfall average of 1,000 mm (Table 1).
| Municipalities | Latitude | Longitude | Land area (km2) | Population | Population density | Annual average rainfall (mm) | Annual average temperature (°C) |
|---|---|---|---|---|---|---|---|
| Bertópolis | 17°03′47″S | 40°34′28″W | 427 | 4,671 | 10.93 | 1,000 | 25 |
| Fronteira dos Vales | 16°53′29″S | 40°55′29″W | 320 | 4,743 | 14.83 | 1,000 | 23 |
| Machacalis | 17°04′38″S | 40°42′59″W | 332 | 7,228 | 21.85 | 1,000 | 25 |
| Santa Helena de Minas | 16°58′59″S | 40°41′08″W | 276 | 6,387 | 22.98 | 1,000 | 25 |
| Umburatiba | 17°15′21″S | 40°34′22″W | 405 | 2,718 | 7.37 | 1,000 | 25 |
Source: Brazilian Institute of Geography and Statistics (2017); Geominas / EMATER.
Geodemographic and physiographic characteristics of the municipalities that make up the coverage area of the Cura D’ars Hospital, Machacalis, Minas Gerais, Brazila
The investigation form used in the municipal hospital reference center and the surrounding municipalities consisted of 59 variable fields referring to general, clinical, and epidemiological data on human injuries caused by poisonous animals. Only the variables of interest for the research were included. However, despite the prerogative that all fields must be filled in by health teams, the system mechanisms that reinforce this requirement only reach the key and mandatory fields.
The prevalence coefficient was calculated by the number of cases multiplied by the constant 100,000 and divided by the assisted population of the hospital coverage area, which produced a result compatible with the number of cases as general and relative prevalence. Population estimation data were obtained from the Brazilian Institute of Geography and Statistics [15].
All patients were assessed for the severity of the poisoning at mild, moderate, and severe levels, which meant that the severity of each case depended on the reaction to the venom of the scorpion and the clinical manifestations presented [16].
The data obtained were arranged in the form of absolute numbers, percentages, and prevalence grouped in Excel spreadsheets and later analyzed by descriptive statistics through simple frequency tests and presented in tables and graphs that reported: age, sex, origin according to the area (rural or urban), municipality and month of occurrence of the injury, type of animal responsible for the injury, part of the body affected, time elapsed between the occurrence of the injury and medical care, use of some type of domestic treatment of the injury before medical care, signs and symptoms presented, clinical classification according to severity, and case evolution.
The research was approved by the Research Review Boarding of Cura D’ars Hospital under protocol number 0128/2017 and authorized by the Epidemiology Sector of the State Health Department of Minas Gerais.
3. RESULTS
3.1. Epidemiological Survey of Cases of Human Victims of Poisonous Animals Assisted at the Hospital Reference Center of Machacalis
A total of 84 patients were identified that corresponded to victims of scorpion sting reported between 2016 and 2017 in the hospital reference center of Machacalis, making a cumulative prevalence of 329.74 cases per 100,000 inhabitants. It was observed that the municipalities of Machacalis, Bertópolis, and Santa Helena de Minas showed the highest occurrence of injuries caused by T. serrulatus (Table 2).
| Municipalities | Scorpion | Prevalence | Snake | Prevalence | Spider | Prevalence | Total | Prevalenceb |
|---|---|---|---|---|---|---|---|---|
| Bertópolis | 22 | 470.99 | 1 | 21.40 | 0 | 0 | 23 | 90.28 |
| Fronteira dos Vales | 1 | 21.08 | 0 | 0 | 0 | 0 | 1 | 3.92 |
| Machacalisc | 32 | 442.72 | 3 | 41.50 | 0 | 0 | 35 | 137.39 |
| Santa Helena | 18 | 281.82 | 2 | 31.31 | 1 | 15.65 | 21 | 82.43 |
| Umburatiba | 11 | 404.70 | 1 | 36.79 | 0 | 0 | 12 | 47.10 |
| Total | 84 | 329.74 | 7 | 27.47 | 1 | 3.92 | 92 | 361.15 |
Source: Epidemiological Surveillance Sector, Cura D’ars Hospital, Machacalis, Minas Gerais, Brazil.
Prevalence per 100,000 inhabitants.
Municipality with hospital reference center.
Occurrence of injuries caused by poisonous animals registered at the Machacalis hospital between the years 2016 and 2017, distributed by municipality of origin and type of injurya
3.2. Number of Cases Per Month of Scorpion Stings in Humans that Occurred between 2016 and 2017
2016 had a higher occurrence of injuries caused by scorpion stings than 2017 (Figure 2). In the analysis of the data obtained, a greater number of cases was observed in 2016, with an ascending peak in August. 2017 had less occurrence despite greater homogeneity of case distribution between the months, demonstrated by a greater peak in January.
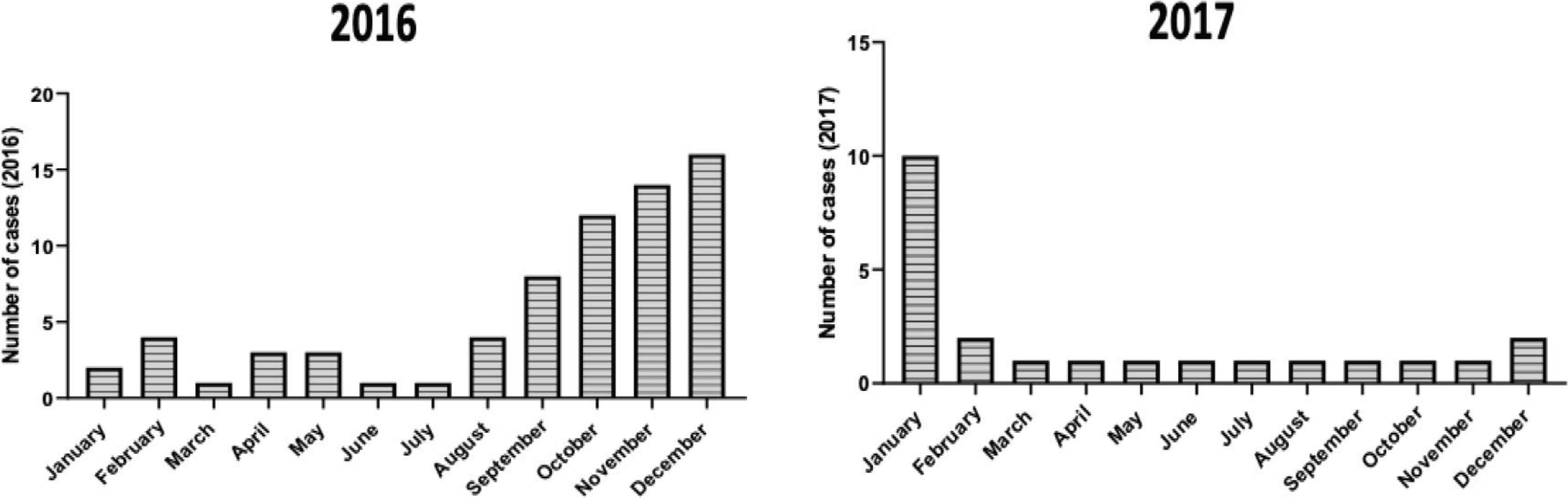
Distribution by number of cases per month of scorpion stings that occurred between 2016 and 2017, covered by the Cura D’ars Hospital, Machacalis, Minas Gerais, Brazil.
3.3. Sociodemographic Profile of Victims of Scorpion Sting who were Identified
Regarding the sociodemographic profile of the cases identified, the proportion was slightly higher in males (52.0%). The most affected groups were people with brown skin (67.0%), people aged 7–14 years (26.0%), and residents of rural areas (68.0%) (Table 3).
| Variables | n | % |
|---|---|---|
| Sex | ||
| Male | 44 | 52.0 |
| Female | 40 | 48.0 |
| Ethnicity | ||
| Brown | 56 | 67.0 |
| Indigenous | 26 | 31.0 |
| White | 1 | 1.0 |
| Black | 1 | 1.0 |
| Age group (years) | ||
| 0–6 | 8 | 9.5 |
| 7–14 | 22 | 26.0 |
| 15–29 | 18 | 21.5 |
| 30–44 | 19 | 22.7 |
| 45–59 | 7 | 8.3 |
| ≥60 | 10 | 12.0 |
| Area of residence | ||
| Rural | 57 | 68.0 |
| Urban | 27 | 32.0 |
Source: Epidemiological Surveillance Sector, Cura D’ars Hospital, Machacalis, Minas Gerais, Brazil.
Sociodemographic profile of victims of scorpion sting assisted at the Cura D’ars Hospital between 2016 and 2017a
3.4. Epidemiological Profile of Victims of Scorpion Sting who were Identified
A total of 30.0% of victims of scorpion sting received medical care within 1–3 h after injury. The hand was the main anatomical region affected by the sting (26.0%) (Table 4).
| Variables | n | % |
|---|---|---|
| Type of occurrence | ||
| Scorpion sting | 84 | 100.0 |
| Elapsed time between the sting and attendance (h) | ||
| 0–1 | 38 | 45.0 |
| 1–3 | 42 | 50.0 |
| 3–6 | 3 | 4.0 |
| 6–12 | 1 | 1.0 |
| Sting spot | ||
| Hand | 22 | 26.0 |
| Foot | 21 | 25.0 |
| Finger | 14 | 16.0 |
| Leg | 9 | 10.0 |
| Trunk | 5 | 6.0 |
| Arm | 3 | 4.0 |
| Forearm | 3 | 4.0 |
| Head | 3 | 4.0 |
| Toe | 3 | 4.0 |
| Thigh | 1 | 1.0 |
| Use of specific serotherapy | ||
| No | 59 | 70.0 |
| Yes | 25 | 30.0 |
Source: Epidemiological Surveillance Sector, Cura D’ars Hospital, Machacalis, Minas Gerais, Brazil.
Epidemiological characteristics of scorpion sting injuries between 2016 and 2017 in the municipalities covered by the Cura D’ars Hospitala
3.5. Clinical Profile of Scorpion Sting Victims According to the Severity of the Poisoning
There was a predominance of minimal poisoning with 70.2% of the cases requiring only symptomatic treatment, followed by cases of moderate poisoning with 21.5% of the sample, and severe poisoning with 8.3%, both requiring specific treatment (Table 5).
| Grade | n | % | ||
|---|---|---|---|---|
| 1 | Minimal envenomation | Local pain and paresthesia | 59 | 70.2 |
| 2 | Moderate envenomation | Severe local pain associated with one or more manifestations, such as discrete nausea, vomiting, sweating, drooling, agitation, tachypnea and tachycardia. | 18 | 21.5 |
| 3 | Severe envenomation | In addition to those mentioned in the moderate form, presence of one or more of the following manifestations: profuse and incoercible vomiting, sweating, severe drooling, prostration, convulsion, coma, bradycardia, heart failure, acute pulmonary edema and shock. | 7 | 8.3 |
Severity of scorpion sting poisoning according to the Grade 1–3 scoring system
4. DISCUSSION
Our results showed that of the 84 cases of scorpion stings assisted by the Cura D’ars hospital, in Machacalis all fell into the category of injuries with poisonous animals, since T. serrulatus is the only species present in the studied region and is also associated with more serious cases because it has the most toxic poison among endemic species of scorpions in Brazil. Machacalis was the municipality with the highest number of cases, although Bertópolis obtained the highest prevalence, followed by Santa Helena de Minas, Umburatiba, and Fronteira dos Vales. It is worth mentioning that the greater number of cases in Machacalis may have been influenced by the location of the reference hospital and by the difficulty of transport from other municipalities, referring only to the cases with the greatest potential for severity.
Among all injuries caused by poisonous animals, scorpion sting occupied a prominent position, as it accounted for approximately 91% of the admitted cases, with a relative prevalence of 329.74 cases per 100,000 inhabitants and contributing to a general prevalence of 361.15 cases per 100,000 inhabitants, when added to the cases of snake and spider bites. It is noteworthy that only the municipality of Machacalis has a hospital reference center in its territory, which may have contributed to a greater concentration of notifications and, even so, there may have been errors or omissions regarding the actual number of occurrences. Under-reporting of these cases is frequent since the health teams of the municipalities do not fill out the notification forms for suspected cases according to the recommendation of the Ministry of Health [17]. Given this situation, we suggest that data incompleteness and inconsistency may have occurred in these specific situations. It is possible that such reference centers when assisting the victims referred from these municipalities failed to complete the fields of the individual investigation form of the information system for notifiable diseases, especially information related to the municipality of occurrence of the injury, leading to a false impression that these cases do not occur in the municipalities of origin and thus overestimating the records of the notifying hospital reference center [18].
It appears that these municipalities did not report these occurrences as they should, or at the time that these cases occurred, possibly so as not to lose or prolong the waiting time for transportation to the hospital reference center. Thus, it is important that health surveillance in municipalities without a hospital unit effectively monitors the evolution of cases and their epidemiological behavior to prevent new occurrences [19].
The only case of injury involving scorpion sting in the municipality of Fronteira dos Vales is not because this injury is unusual in that location, but it is because the majority of the victims in that municipality are referred to the hospital reference center located in the city of Águas Formosas, for geographic and logistical issues. The Information System for Notifiable Diseases reported that, in 2016–2017, 41 cases of injuries by poisonous animals were registered in the municipality, 37 of which were scorpion stings [17].
The municipalities of Bertópolis and Santa Helena de Minas have rural districts and two indigenous lands where the Maxakali indigenous people live. The characteristics of the population of these two municipalities may have contributed to the increase in cases due to a large number of rural residents and also the lack of housing and sanitation conditions for the indigenous population [20].
A higher relative prevalence of injuries caused by scorpions was observed, which can be justified by the geographical and climatic characteristics of the studied region and by the circulation of the species T. serrulatus. This is popularly known as the yellow scorpion and considered the most dangerous, in which its parthenogenesis process allows that the female scorpion generates copies of itself twice a year without the need for mating [21]. Besides, the study region has low socioeconomic conditions and climatic characteristics that vary from hot to rainy in summer and dry in winter, favoring the circulation of this species. Its vegetation is formed by the transition between the Cerrado and the Atlantic Forest biomes that have lost space for agricultural activities with high rates of deforestation [22], modifying the ecological dynamics of the scorpion fauna [9], contributing to increasing the prevalence of these injuries in the region studied.
The prevalence found for scorpion sting confirms the trend of cases increasing of this condition in Brazil in recent years [11]. Although injuries by snakes and spiders are the most frequent in the northern and southern regions of the country, respectively, our results showed greater epidemiological similarity with the northeast region, with a higher occurrence of injuries caused by scorpions [23–25].
Figure 2 shows that a greater number of cases was observed in the spring and summer of 2016. In 2017, there was a greater predominance in the summer, which tends to be warmer and rainier, and favors the biological behavior of hunting and reproduction of these animals, coinciding with the planting season and farming practices that justify this monthly variation. However, we found no justification for this important difference in the notifications that occurred between 2016 and 2017. It was observed that there were no institutional campaigns that encouraged preventive measures that justified a notable reduction in cases in 2017. Our results are similar to other studies carried out in the state of Minas Gerais [11,26].
Regarding the sociodemographic profile, the majority of scorpion sting victims identified in the present study were students, followed by farmers, domestic workers, and unemployed people, differing from the occupational reality of the subjects of other consulted studies [7,9]. In this study, stings were slightly more common in men, converging with most studies that indicated a higher prevalence for men [9–21]. Regarding ethnicity, brown-skinned individuals had a higher proportion affected, this may be justified by the higher population proportion for this color in the Brazilian population in the region studied according to Brazilian Institute of Geography and Statistics estimates, which reported that most of the regional population declares itself as brown and that few studies have addressed the ethnic aspects of this condition [27]. It is noteworthy in this study that the proportion of cases in the Maxakali indigenous population was almost half of that in the brown population and larger than in white and black people.
The data obtained lead us to believe that this number is underestimated, as not all victims attended the Machacalis hospital, with the most serious cases being referred to more equipped hospital reference units located in Águas Formosas, Teófilo Otoni, and Governador Valadares for appropriate and timely treatment of such emergencies. In addition, many occurrences go unnoticed by the health authorities, since many Maxakali Indians do not resort to health care, especially when they are victims of scorpion bites, and prefer to use popular medicine combined with religious rituals [28].
The study revealed a higher percentage of involvement in the age group from 7 to 14 years, diverging from several studies that reported most cases being aged >20 years [29,30].
Cases were predominant in individuals from rural areas, converging with some studies found in the literature [31,32], but diverging from the current trend of increasing cases in urban areas due to population increase and uncontrolled deforestation to expand the agricultural frontier [33].
Most of the identified cases of a scorpion sting (50.0%) were treated within a maximum time interval of 1–3 h, between the time elapsed from the sting and the beginning of medical care. It was observed that, with the time of attendance, the residents of the host city of the evaluated hospital had easier access, which resulted in a considerable reduction in the time between the occurrence of the injury and the attendance [2]. Although it is possible to observe an acceptable time in the analyzed cases, the lack of infrastructure on the unpaved roads and the distance from some rural localities to the hospital unit can compromise care. Despite no deaths were observed, attendance delay is a determining factor of mortality, which associated with the underreporting of lighter cases and the difficulty of access may have made it possible to attend only the most serious cases. Delays in the time of care can considerably increase the lethality of these cases when the care is performed between 6 and 12 h after the injury [34].
As for the anatomical region of the sting, among the 10 sites investigated, the upper and lower limbs stood out, as the corporeal extremities are considered vulnerable places when performing vigorous activities such as agricultural activities, handling of machines, tools, cleaning and removal of debris, among others. The aspects related to the body area most frequently reached in the present research are also similar to the studies published in Brazil and other regions of the world [35–37].
We observed that most cases did not use specific serotherapy, due to their classification as mild cases, and only used symptomatic drugs. In the context of moderate to severe cases in the present sample, the treatment instituted was specific serotherapy for the scorpion of the Tityus genus. In cases where it is not possible to differentiate between injuries with spiders of the Phoneutria genus and with scorpions of the Tityus genus (due to the similarity of the clinical manifestations and the nonidentification of the animal causing the injury), or in the absence of specific serotherapy for scorpion stings, the trivalent antidote is recommended, which neutralizes the venom of the Loxosceles and Phoneutria spiders, and the Tityus scorpion. This initiative may have been the reason there were no deaths from this type of envenomation in this evaluation period [2].
The severity of poisoning is directly related to individual issues, such as body mass and age, size of the animal causing the injury, affected region, amount of poison inoculated, individual sensitivity to the poison, and health status of the victim [37,38]. Regarding the severity of scorpion bites, 70.2% of the affected individuals were classified as having mild poisoning, with a benign course. The cases classified as mild had only local manifestations, such as pain at the sting site and paraesthesia. These clinical characteristics are similar to those found in studies conducted in different Brazilian states [31,39] and in other countries [40,41]. In most cases, where there is only one local condition, treatment is symptomatic and consists of pain relief, usually with the anesthetic block in the affected region, and administration of analgesics and antihistamines [42].
Moderate and severe cases accounted for 21.5% and 8.3% of the sample, respectively. The clinical manifestations of the moderate cases that predominated were severe pain at the sting site, mild sweating, nausea, occasional vomiting, and tachycardia, as reported by several previous studies [43,44]. Concerning the cases classified as severe, in addition to presenting with intense pain and sweating, they also showed profuse vomiting, agitation, and prostration, without heart failure, pulmonary edema, shock, seizures, and coma, as reported in other research [45]. In these patients, specific serotherapy is required and, generally, two to six ampoules should be administered intravenously as soon as possible, in an appropriate dose, according to the severity of the condition [46]. Patients with systemic manifestations, especially children, must be kept under continuous observation of vital functions, aiming at the early diagnosis and treatment of complications [45].
Regarding case evolution, the entire sample had a favorable prognosis, progressing to cure, with no record of death or any local or systemic complications associated with the injury. It is possible to notice that there is a relationship between the time elapsed between the sting and the beginning of medical care and the prognosis in each particular case [46].
Some limitations need to be considered in this study, such as the lack of quality and inconsistencies in hospital records, in addition to the under-reporting of these injuries by local health teams and even the personal judgment of the victims themselves when deciding not to seek medical attention in cases of minor injuries when they believed that medication was not necessary.
The survey of the victims of injuries caused by scorpion sting allows a better knowledge of its prevalence. According to Lima-Costa and Barreto [47], descriptive studies allow determination of the distribution of diseases or health conditions, considering the time, place, or characteristics of the affected individuals.
We suggest that it is necessary to recognize the importance of strategies such as the training of health professionals to enable the proper filling of forms; raising the awareness of these professionals about the importance of the quality of the records produced; systematic monitoring of the quality of the database, performing routine analyzes to identify eventual incompleteness, inconsistency or duplicity; in addition to performing information retrieval.
The findings of the current study increase our understanding of the epidemiology of injuries caused by scorpion stings and could be useful in identifying the conditions that increase the risk of envenomation in the region. Furthermore, this study provides data for the local development of health actions to promote the control and prevention of these injuries.
5. CONCLUSION
Injuries caused by scorpion sting are a major challenge for public health in Brazil, mainly because its characteristics as a tropical country favor the proliferation of these animals. Also, the lack of efficiency and quality of data has harmed public policies aimed at the most vulnerable populations, especially for residents of the rural area and the Maxakali Indigenous people. In this sense, only through necessary interventions such as timely notification, clinical approach to cases for adequate treatment, and improving data quality and feedback between the collaborative care network, government, and population, will it be possible to overcome this condition.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
Drafting, literature review, data collection, statistical analysis and article writing: DSTJ, ABSM, BSF, JML, LSP and MECS. Article writing, analysis and interpretation of data, critical revision and supervision: EMA, RCO and LCV. All authors read and approved the final version of the manuscript.
ACKNOWLEDGMENTS
The authors would like to thank the clinical direction and the Epidemiology Sector of Cura D’ars Hospital who supported this research from the beginning to the end.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Dilceu Silveira Tolentino Júnior AU - Eliseu Miranda de Assis AU - Roberto Carlos de Oliveira AU - Arlanjo Bispo de Sousa Marques AU - Bruno Souza Farias AU - Jessé Medeiros Leandro AU - Lucas Silveira Paulo AU - Mácio Emílio Caldeira da Silva AU - Lízia Colares Vilela PY - 2020 DA - 2020/09/08 TI - Epidemiological and Clinical Aspects of Scorpion Envenomation in Machacalis, Minas Gerais, Brazil, from 2016 to 2017 JO - Dr. Sulaiman Al Habib Medical Journal SP - 128 EP - 135 VL - 2 IS - 3 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.200903.002 DO - 10.2991/dsahmj.k.200903.002 ID - TolentinoJúnior2020 ER -
