The Incidence and Prognosis of ICU Delirium: A Retrospective Study from a Single Center
- DOI
- 10.2991/icres.k.210206.001How to use a DOI?
- Keywords
- Delirium; ICU; sleep quality; 28-day mortality; length of ICU stay
- Abstract
Purpose: Delirium is a frequent occurrence amongst Intensive Care Unit (ICU) patients, but studies on its causes are sparse and its risk factors vary from disease to disease. Here, in this study, an attempt was made to investigate the factors associated with the prognosis of delirium in the ICU.
Methods: An observed study was performed of consecutive patients from September 2016 to November 2016 who were admitted to the ICU. The patients were screened for delirium by using the diagnostic tools of the Richmond Agitation Sedation Scale score and the Confusion Assessment Method ICU. Patients were divided into subgroups according to heart/vascular, cerebral, pulmonary, maxillofacial/limbs, obstetric, urinary and spinal disease.
Results: A total of 406 patients of which 186 developed delirium (45.8%). The main causes of delirium were different. The only independent factor for delirium in heart and vascular subgroups was the quality of sleep (Odds Ratio (OR) = 0.236, p < 0.001 [0.111–0.500]). For those with intestinal disease, the risk factors included age (OR = 2.514, p = 0.002 [1.397–4.524]), use of vasoactive therapies (OR = 13.799, p = 0.002 [2.669–71.361]) and the quality of sleep (OR = 0.114, p < 0.001 [0.036–0.366]). Older age (OR = 1.100, p = 0.022 [1.014–1.194]), higher acute physiology, age and chronic health evaluation II scales (OR = 1.255, p < 0.001 [1.112–1.417]) and the quality of sleep (OR = 0.090, p = 0.034 [0.010–0.829]) were noted as risk factors for septic shock patients. Delirium led to extended ICU-stays (p < 0.001), and only the subgroups of septic shock patients showed a difference in 28-day mortality rates (p = 0.006).
Conclusion: The incidence of delirium and its associated risk factors varied according to disease type. In the study cohort, the highest 28-day mortality was recorded for the patients admitted for septic shock who had developed delirium.
- Chinese Abstract
目的:谵妄是重症监护病房(ICU)患者的常见症状,但对其病因的研究很少,且其危险因素因疾病而异。在本次研究中,我们探讨了与ICU患者谵妄预后相关的因素。
方法:连续纳入2016年9月至2016年11月入住ICU的患者进行观察性研究。采用Richmond躁动-镇静评分量表和ICU意识状态评估法评估患者谵妄情况;并根据心脏/血管、脑、肺、颌面部/四肢、产科、泌尿和脊柱疾病将其分为亚组。
结果:共纳入了406例患者,其中186例为谵妄患者(45.8%)。造成谵妄的主要原因各异;在心脏/血管疾病亚组中,睡眠质量是导致谵妄的唯一的独立危险因素(OR=0.236;95%置信区间,[0.111–0.500];p < 0.001)。在胃肠道疾病患者中,导致谵妄的危险因素包括年龄(OR=2.514;95%置信区间,[1.397–4.524];p = 0.002)、使用血管活性药物(OR = 13.799;95%置信区间,[2.669–71.361]; p = 0.002)和睡眠质量(OR = 0.114;95%置信区间,[0.036–0.366];p < 0.001)。此外,年龄较大(OR = 1.100;95%置信区间, [1.014–1.194]; p = 0.022),较高的急性生理学、年龄和慢性健康评估II 评分(OR =1.255;95%置信区间,[1.112–1.417]; p < 0.001)和睡眠质量(OR = 0.090;95%置信区间,[0.010–0.829]; p = 0.034)被认为是脓毒性休克患者的危险因素。谵妄导致ICU住院时间延长(p < 0.001),且与其他亚组相比,脓毒性休克亚组的28天病死率存在差异(p = 0.006)。
结论:谵妄的发生率及其相关的危险因素因疾病而异。在本研究队列中,发生谵妄的脓毒性休克患者28天病死率最高。
- Copyright
- © 2021 First Affiliated Hospital of Zhengzhou University. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Intensive Care Units (ICUs) are specialist wards providing intensive care to critically ill patients or to those in an unstable condition. ICUs are typically multidisciplinary, admitting patients with a range of pathologies that require intensive or high dependency care due to disease severity or unstable disease presentation [1]. Given the severity of the condition of the ICU patients, delirium is a common occurrence, with incidence rates ranging from 11% to 80% reported in previous studies [1–3]. Delirium is characterized by transient states of cognition/consciousness [4] that can lead to extended ICU stays, loss of cognitive function, mortality or a heightened risk of death after 6 months. The disorder, therefore, represents a burden to patients, relatives, and health care systems [5–7].
The treatment of delirium in the ICU is dependent on its early diagnosis, the alleviation of modifiable risk factors, and the treatment of predisposing factors [8]. Previous [9] studies identified age, Complexity Prediction Instrument (COMPRI) scores, and psychosocial vulnerabilities as risk factors. Tse et al. [10] performed a retrospective analysis that identified a history of delirium, in different patient populations with independent risk factors such as Cardiopulmonary Bypass Graft in patients aged ≥64 years, stroke patients, those experiencing a transient ischemic attack, depression, a loss of cognitive function, and beta-blocker usage prior to surgery. Wang et al. [11] further showed that age (>70 years), anesthesia, hypercapnia during operation, surgery lasting over 3 h, hypotension, and sleep disorders were associated with delirium in geriatrics undergoing orthopedic surgery. The occurrence of delirium varied according to disease type.
A diagnosis for delirium can be made based on medical history, the assessment of mental status and the identification of possible contributing factors. Typical examinations include mental status examinations that include assays of awareness, attention and thinking, either informally or through conversation; assessments of mental state, confusion, perception and memory; physical and neurological exams and the analysis of underlying disease. The assessment of delirium in the ICU setting includes the Confusion Assessment Method for the ICU (CAM-ICU) [12] and the Intensive Care Delirium Screening Checklist [13,14]. The CAM-ICU is verified as an accurate predictor of delirium occurrence in critically ill patients [15]. In the present study, we investigated the risks of delirium in ICU patients to identify specific characteristics as prognostic indicators. We focused on subjects with a range of disease types to improve disease prognosis and identification. Since the causes and occurrence of delirium in the ICU vary according to disease-type, our study aimed to identify novel independent risk factors in the patients admitted to ICU. The results of this study would offer new insights for patient management and treatment in the ICU setting.
2. MATERIALS AND METHODS
2.1. Patient Setting
The study was performed in a large mixed medical ICU from September 2016 to November 2016 in Changsha, China. The ICU was isolated from the rest of the hospital and was managed by accredited intensivists responsible for patient care. Ward rounds were performed twice per day and treatment plans were regularly reviewed. The lights of the ICU were dimmed to promote sleep.
2.2. Study Population
The inclusion criteria in this study were therefore as follows: age >18 years; ICU treated for >24 h. Informed consent was provided by the patient or next of kin.
Exclusion criteria: known sleep disorders, drug-treated mental illness, psychological issues, cognitive disorders, dementia or central neurological impairment diagnosed by radiological scans; and Richmond Agitation-Sedation Scale (RASS) scores ≥4 during the ICU stay.
2.3. Data Collection
Patient data were collected on weekdays and included characteristics such as gender, age, alcohol and nicotine intake, diabetes, hypertension and vascular disease. The cut-off time was 28 days.
2.4. Delirium Measurements
The symptoms of delirium were assessed twice daily by two ICU clinicians using the CAM-ICU scales. Delirium was defined as: (1) acute changes or fluctuations in mental state; (2) a loss of attention; (3) changes in consciousness; and (4) unordered thoughts. Delirium was present for values of: 1 + 2 + 3 or 1 + 2 + 4 [16]. Patients with delirium were considered positive when presenting at least one positive CAM-ICU during the ICU stay.
2.5. Assessment of Diseases Types
Patients were divided into subgroup according to heart/vascular disease, cerebral disorders, pulmonary disease, disease of the maxillofacial/limbs, gynecologic disorders, obstetric disease, urinary and spinal disease. Sepsis 3.0 was used to diagnose septic shock [17].
2.6. Statistics
Data were represented as mean ± SD, and were analyzed using SPSS 18.0 software (Armonk, New York). Differences amongst the groups were compared using a t-test for normally distributed data, and a Wilcoxon rank-sum test for non-normal data, represented by M (P25, P75). χ² tests were used to compare categorical variables (theoretical frequency <5 for continuous correction methods). For theoretical frequencies <1, exact probability methods were adopted. Kaplan-Meier (KM) curves were analyzed using log-rank tests. Survival analyses were performed via stepwise Cox regression models. p < 0.05 and p < 0.01 were deemed statistically significant.
3. RESULTS
This was an observational study of consecutive patients from September 2016 to November 2016 admitted to the ICU for surgery or treatment. In total, 42/459 patients were excluded, with 11 not completing the delirium assessments. Therefore, 406 patients were enrolled following CAM-ICU evaluations. Of these patients, 107 had vascular and cardiac disease, 107 had intestinal disease, 41 had diseases of the pulmonary system, 37 suffered from septic shock, 34 had cerebral disease, 29 had maxillofacial/limbs, 21 had gynecologic disease, 17 had urinary disease, and 13 had diseases of the spine (Figure 1).
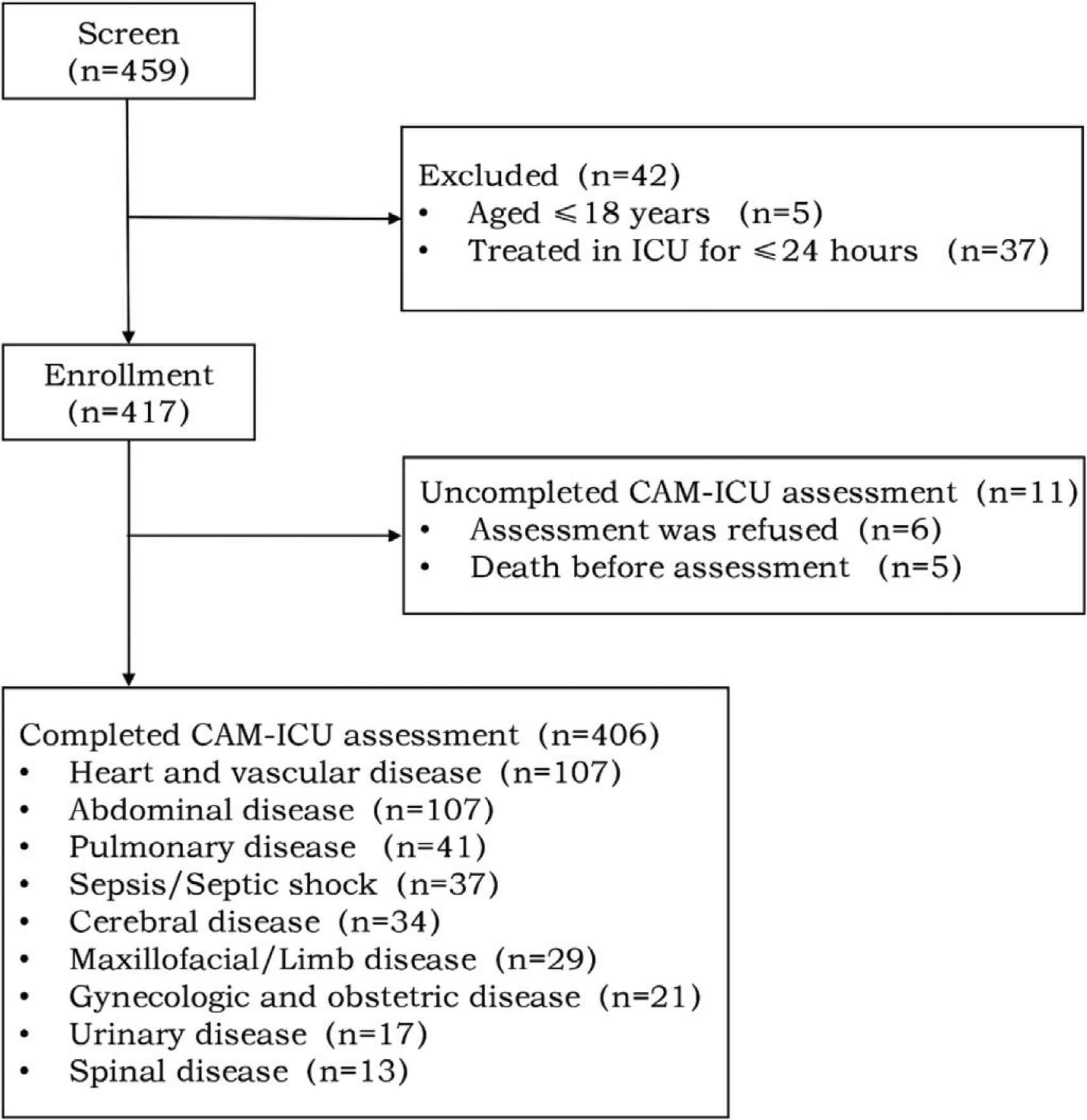
Flow diagram of the study protocol. A total of 406 patients were finally enrolled. Inclusion criteria: age >18 years; ICU treatment for >24 h. Informed consent provided by the patient or next of kin. Exclusion criteria: known sleep disorders, drug treated mental illness, psychological issues, cognitive disorders, dementia or central neurological impairment diagnosed by radiological scans; and RASS scores ≥3 during the ICU stay.
3.1. Biochemical Indicators and Baseline Features
Of the 406 included patients, 186 (45.8%) suffered from delirium in the ICU. The patients with delirium were aged 60 ± 14 years (n = 186) in comparison to 50 ± 16 years for ICU patients without delirium (n = 220, p < 0.001). Compared to those without delirium, sequential organ failure assessment (8 ± 5 vs 5 ± 4) and Acute Physiology, Age and Chronic Health Evaluation (APACHE II) (14 ± 6 vs 9 ± 5; p < 0.001) scores were higher in delirium patients. The patients with delirium had a poor sleep quality (p < 0.001), hypertension (39% vs 25%, p = 0.003), were sedated (82% vs 65%; p < 0.001), had high multiple organ dysfunction syndrome scores (40% vs 21%; p < 0.001) high levels of vasoactive drug administration (39% vs 29%; p = 0.04). Longer ventilation times (11 h [3, 27] vs 5 h [1, 10]; p < 0.001), longer duration of ICU stay (5.5 ± 5.4 vs 3.0 ± 2.5; p < 0.001) and higher 28-day mortality rates (13% vs 4%; p < 0.001) were reported for those that developed delirium (Table 1).
| Variables | Delirium (n = 186) N (%) | Non delirium (n = 220) N (%) | p-value |
|---|---|---|---|
| Age, mean (SD)a, years | 60 ± 14 | 50 ± 16 | <0.001 |
| Men | 101 (54) | 135 (61) | 0.151 |
| Medical history | |||
| Hypertension | 73 (39) | 56 (25) | 0.003 |
| Cardiac disease | 55 (30) | 48 (22) | 0.074 |
| Diabetes | 21 (11) | 18 (8) | 0.29 |
| Smoking history | 48 (26) | 73 (33) | 0.105 |
| Drinking history | 24 (13) | 28 (13) | 0.958 |
| Baseline features | |||
| APACHEb II score, mean (SD) | 14 ± 6 | 9 ± 5 | <0.001 |
| SOFAc score, mean (SD) | 8 ± 5 | 5 ± 4 | <0.001 |
| MODS | 75 (40) | 46 (21) | <0.001 |
| Mechanical ventilation | 156 (84) | 171 (78) | 0.119 |
| Duration of ventilation, median (IQR), h | 11 [3, 27] | 5 [1, 10] | <0.001 |
| Sedation | 152 (82) | 143 (65) | <0.001 |
| Vasoactive drugs | 72 (39) | 64 (29) | 0.04 |
| Sleep quality assessment (PSQI) | <0.001 | ||
| Fairly good | 5 (3) | 57 (26) | – |
| Fairly bad | 18 (10) | 80 (36) | – |
| Very bad | 163 (87) | 83 (38) | – |
| Prognostic indicators | |||
| Duration of ICU stay | 5.5 ± 5.4 | 3.0 ± 2.5 | <0.001 |
| Duration of hospital stay | 20.5 ± 11.9 | 19.5 ± 17.2 | 0.504 |
| 28-day mortality | 25 (13) | 9 (4) | 0.001 |
| Biochemical indicators | |||
| PH | 7.37 ± 0.10 | 7.40 ± 0.10 | 0.422 |
| PaO2 | 128.6 ± 63.2 | 135.1 ± 58.1 | 0.284 |
| PaCO2 | 128.6 ± 63.3 | 39.3 ± 14.3 | 0.787 |
| Lac | 3.3 ± 8.5 | 2.1 ± 2.7 | 0.052 |
| WBC | 14.8 ± 6.9 | 14.2 ± 7.3 | 0.352 |
| Hb | 96.0 ± 24.3 | 98.5 ± 23.1 | 0.285 |
| PLT | 146.5 ± 73.2 | 162.7 ± 87.9 | 0.047 |
| HCT | 29.5 ± 7.1 | 30.6 ± 11.3 | 0.234 |
| PCT | 2.0 [0.2, 12.1] | 0.9 [0.2, 4.7] | 0.023 |
| ALB | 28.5 ± 5.9 | 29.6 ± 6.4 | 0.082 |
| TBIL, median (IQR) | 15.3 [9.3, 31.2] | 15.9 [10.3, 24.3] | 0.674 |
| DBIL, median (IQR) | 7.2 [4.1, 14.9] | 7.4 [4.45, 11.15] | 0.503 |
| ALT, median (IQR) | 22.9 [13.5, 49] | 21.0 [13.0, 39.4] | 0.155 |
| AST, median (IQR) | 40.0 [24.0, 98.0] | 38.6 [20.7, 78.3] | 0.091 |
| BUN, median (IQR) | 8.5 [5.4, 12.7] | 6.7 [4.3, 10.2] | <0.001 |
| Cr, median (IQR) | 110.0 [83.0, 165.0] | 92.0 [72.0, 123.5] | 0.027 |
| UA, mean (SD) | 318.6 ± 146.4 | 297.6 ± 142.5 | 0.146 |
SD, standard deviation;
APACHE, acute physiology, age and chronic health evaluation;
SOFA, sequential organ failure assessment;
MODS, multiple organ dysfunction syndrome.
Baseline characteristics stratified by delirium
In terms of biochemical indicators, the non-delirium group had higher levels of BUN (8.5 [5.4, 12.7] vs 6.7 [4.3, 10.2], p < 0.001) PCT (2.0 [0.2, 12.1] vs 0.9 [0.2, 4.7], p = 0.023), and Cr (110.0 [83.0, 165.0] vs 92.0 [72.0, 123.5], p = 0.027), whilst PLT levels declined (146.5 ± 73.2 vs 162.7 ± 87.9, p = 0.047). No differences were observed between the other indicators (Table 1).
3.2. Delirium According to Disease Types
A total of 406 patients were studied of which 186 developed delirium (45.8%). We found that the highest incidence of delirium was amongst the subgroup of cerebral disease (68%), followed by pulmonary disorders (63%), maxillofacial/limbs (52%), septic shock (49%), cardiac and vascular disease (44%) and intestinal disease (42%) (Figure 2).
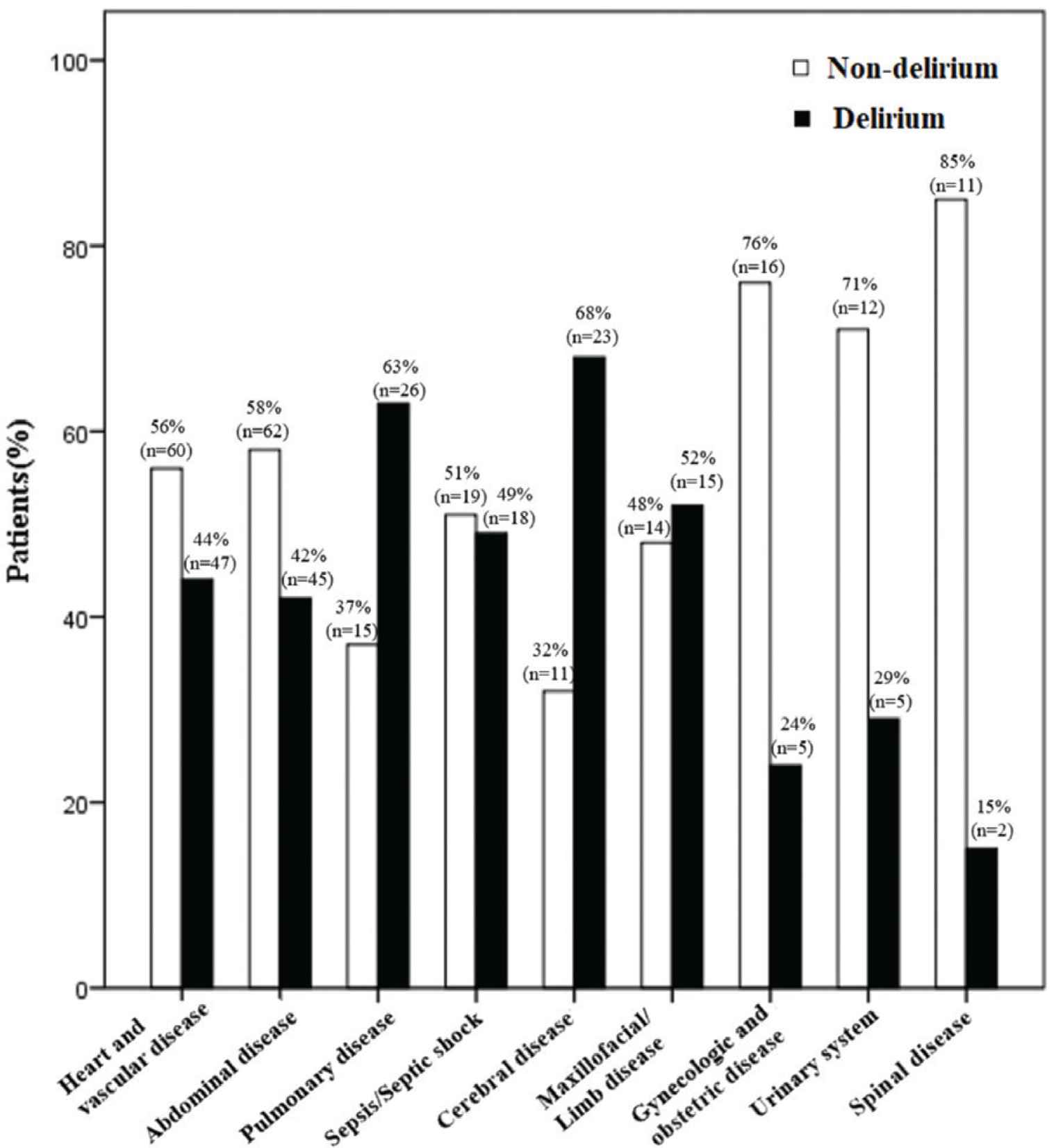
Delirium according to disease types. The symptoms of delirium were assessed twice daily by two ICU clinicians. Delirium was defined as: (1) acute changes or fluctuations in mental state; (2) loss of attention; (3) changes in consciousness; and (4) unordered thoughts. Delirium was considered present at values of: 1 + 2 + 3 or 1 + 2 + 4. Patients with delirium were positive when presenting at least one positive CAM-ICU during the ICU stay. In total, 186/406 patients had delirium.
Considering the occurrence of delirium as a dependent covariate, we used multiple logistic regression for data comparisons. Logistic regression variables were then introduced into the univariate analysis, including those with p-values <0.05. From these analyses, we observed that older patients were likely to develop delirium (Odds Ratio (OR) = 1.756, p = 0.001 [1.406–2.194]) as were those with higher APACHE II scores (OR = 1.093, p = 0.001 [1.039–1.150]). Patients with a longer duration of ventilation also showed increased susceptibility to the development of delirium (OR = 1.022, p = 0.012 [1.005–1.040]). Sedated patients (OR = 3.406, p < 0.001 [1.867–6.212]) were prone to delirium, whist a good sleep quality was protective against the onset of delirium (OR = 0.186, p < 0.001 [0.121–0.288]) (Table 2).
| Variables | All patients (n = 406) [p; (ORa, 95% CI)] | Heart and vascular disease (n = 104) [p; (OR, 95% CI)] | Abdominal disease (n = 92) [p; (OR, 95% CI)] | Sepsis/Septic shock (n = 37) [p; (OR, 95% CI)] | Cerebral disease (n = 31) [p; (OR, 95% CI)] | Pulmonary disease (n = 36) [p; (OR, 95% CI)] |
|---|---|---|---|---|---|---|
| Age, years | 0.001; (1.756, 1.406–2.194) | – | 0.002; (2.514, 1.397–4.524) | 0.022; (1.100, 1.014–1.194) | – | – |
| APACHE II score | 0.001; (1.093, 1.039–1.150) | – | – | <0.001; (1.255, 1.112–1.417) | – | – |
| Sedation | <0.001; (3.406, 1.867–6.212) | – | – | – | – | – |
| Vasoactive drugs | – | – | 0.002; (13.799, 2.669–71.361) | – | – | – |
| Sleep quality assessment (PSQI) | <0.001; (0.186, 0.121–0.288) | <0.001; (0.236, 0.111–0.500) | <0.001; (0.114, 0.036–0.366) | 0.034; (0.09,0.010–0.829) | – | – |
| Duration of ventilation | 0.012; (1.022,1.005–1.040) | – | – | – | – | – |
OR, odds ratio.
“–” represents p is not statistically significant.
Multivariate regression analysis of the risk factors for delirium as a dependent variable in all patients and diseases types
Regarding disease status, delirium development in cardiac patients was dependent on sleep levels (OR = 0.236, p < 0.001 [0.111–0.500]). For ICU patients with intestinal disease, the use of vasoconstrictive agents (OR = 13.799, p = 0.002 [2.669–71.361]), older age (OR = 2.514, p = 0.002 [1.397–4.524]) and low levels of sleep (OR = 0.114, p < 0.001 [0.036–0.366]) were risk factors. For septic shock patients, higher APACHE II scores (OR = 1.255, p < 0.001 [1.112–1.417]), low sleep levels (OR = 0.090, p = 0.034 [0.010–0.829]), and an older age (OR = 1.100, p = 0.022 [1.014–1.194]) were found to be the risk factors for disease. There were no notable risk factors of delirium in those with lung or cerebral disease, though the patient numbers were low in these groups (Table 2).
3.3. Prognosis of Delirium in Different Diseases Types
The length of ICU stays and 4-week survival times were compared through multivariate stepwise Cox regression models in delirium and non-delirium groups. We found that in all patient groups, delirium led to a significantly longer ICU stay (p < 0.001) and higher 28-day mortality (p = 0.001).
The length of ICU stays in those with cardiac disease (p < 0.001), pulmonary disorders (p = 0.011), septic shock (p < 0.001), cerebral disease (p = 0.011) and intestinal disease (p = 0.47) were comparable to the general population (Figure 3). Only the subgroup of septic shock patients showed higher 28-day mortality in comparison to other patients with delirium (p = 0.006, Figure 4).
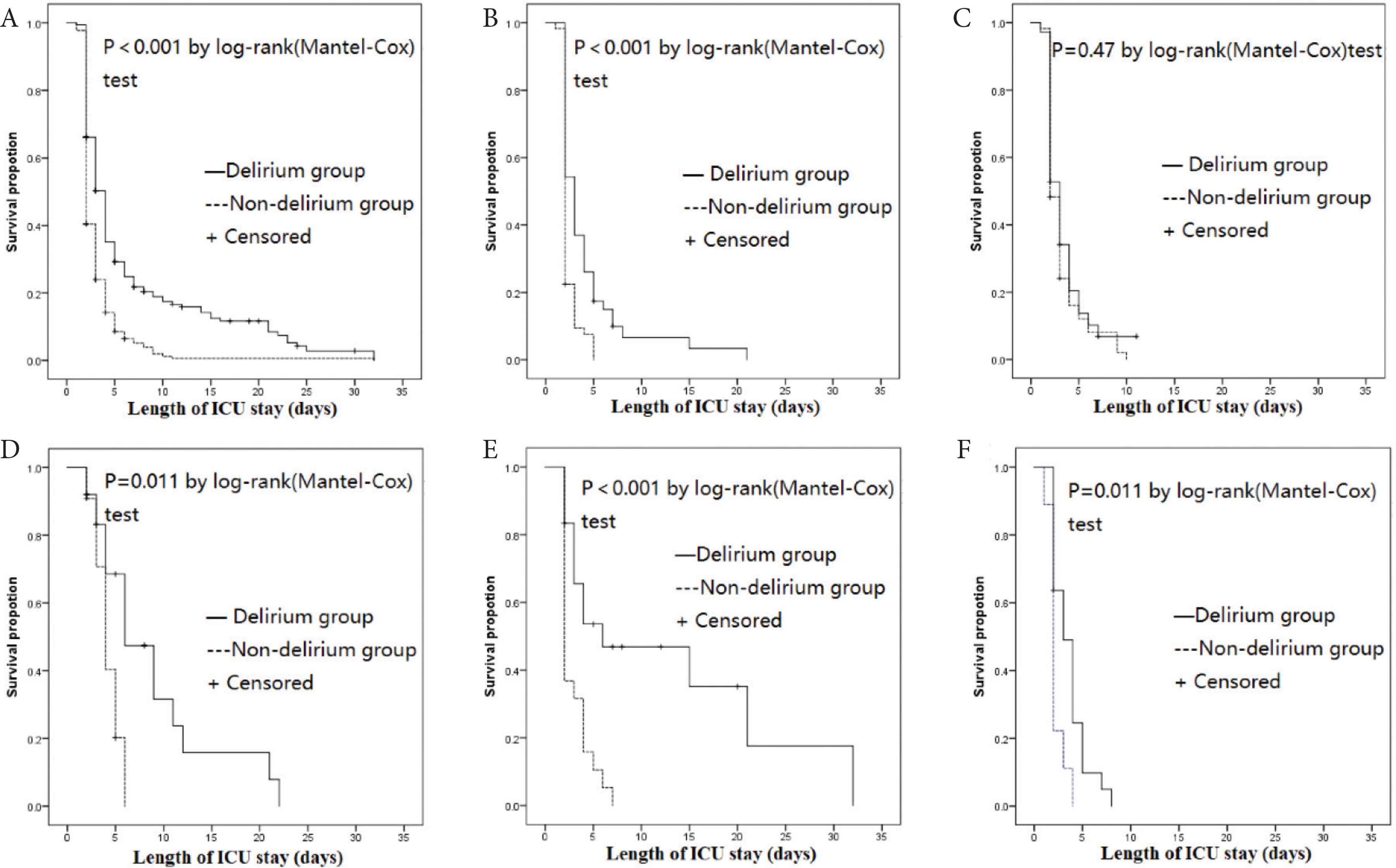
Length of ICU stay according to disease types in patients with or without delirium. Subgroups were classified according to disease types as described in materials and methods. Delirium was assessed as shown in Figure 1. A = Total patient cohort; B = Cardiac/vascular disease patients; C = Intestinal disorders patients; D = Pulmonary disorders patients; E = Septic shock patients; F = Cerebral disease patients.
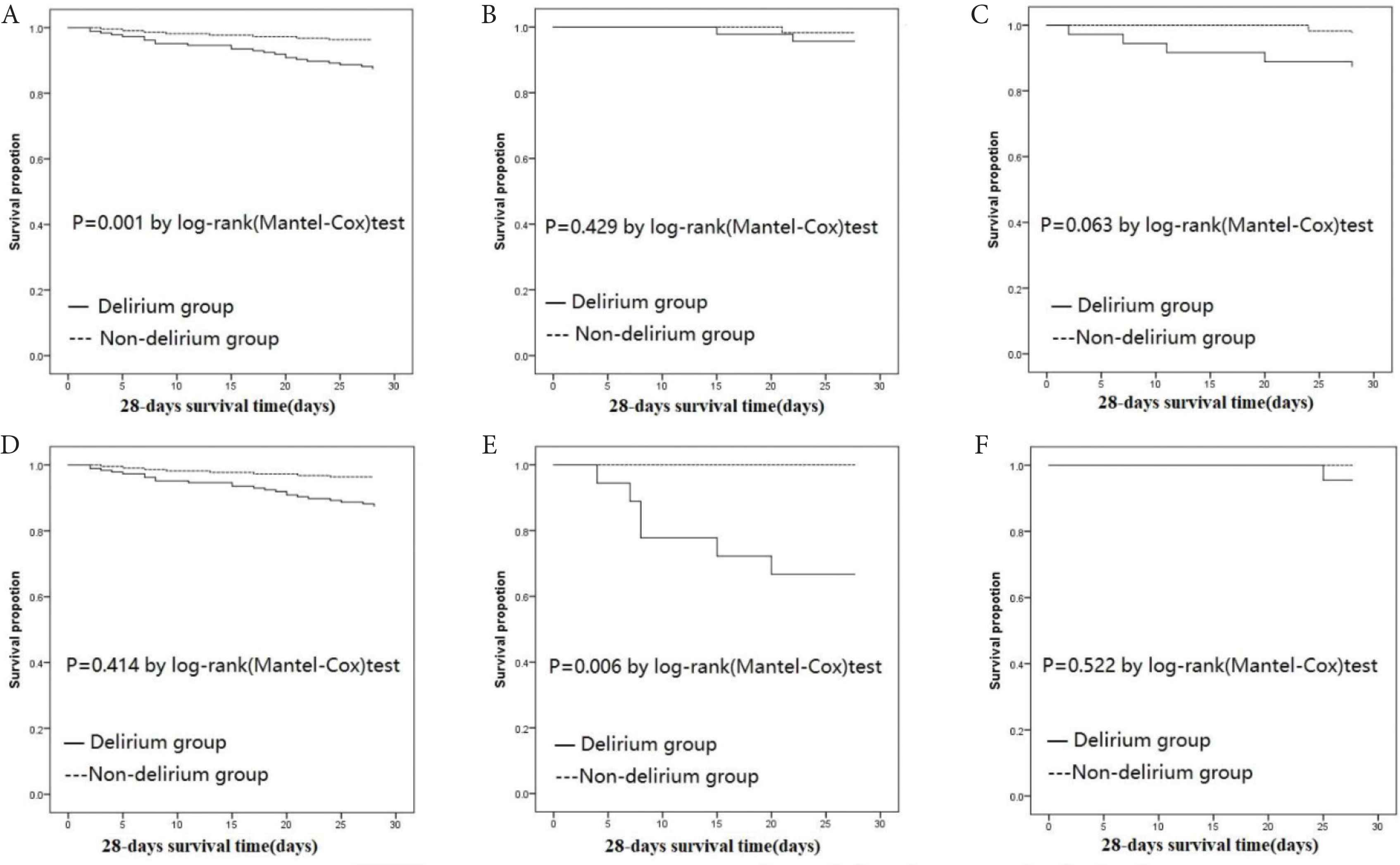
Rates of 28-day mortality between delirium and non-delirium groups. A = Total patient cohort; B = Cardiac/vascular disease patients; C = Intestinal disorders patients; D = Pulmonary disorders patients; E = Septic shock patients; F = Cerebral disease patients.
4. DISCUSSION
Given the severe condition of ICU patients, delirium is common, with incidence rates ranging from 11% to 80%, which can lead to prolonged ICU stays, mortality, cognitive decline, and an increased risk of death after 6 months [1–3]. In our study, of the 406 patients assessed, 186 (45.8%) had delirium in the ICU. We demonstrated that delirium is strongly associated with a poor prognosis that varies according to the underlying disease types. A range of independent risk factors were identified to be associated with delirium upon the analysis of the disease characteristics of each patient subgroup. We found that ICU delirium was related to a poor prognosis with longer ICU stays and higher 28-day mortality. Amongst them, those with septic-shock associated delirium had the highest 28-day mortality.
For this study the symptoms of delirium were assessed twice daily by two ICU clinicians using the CAM-ICU scales. We found that delirium occurred in 45.8% of patients (range: 15–68%) which was comparable to previous assessments in those with sepsis [6,18]. In a Japanese study, 27.8% of patients developed delirium in the ICU. In cardiac patients, delirium rates of 28% have been reported. Delirium was also shown to occur to high rates in transapical Transcatheter Aortic Valve Implantation (TAVI) (47%) patients, but was less common in transfemoral TAVI (17%) [10]. It probably depends on the type of disease, and our study included a variety of diseases that were common in the ICU, and the study showed that the overall incidence of delirium in the ICU was 45.8%, suggesting that the incidence of delirium in the ICU was high.
We found that the use of sedatives, APACHE II scores, sleep disorders and ventilation duration could predict delirium. However, the risk factors varied according to disease types. The pathophysiological mechanisms of delirium development are largely undefined [19] and are mainly dependent on the physiological characteristics of individual patients [8,11,20]. Yamaguchi et al. [9] found that older age and biopsychosocial vulnerability revealed through the COMPRI scale, led to a risk of ICU delirium and could therefore, predict mortality and longer ICU stays. Harten et al. [21] demonstrated that during cardiac surgery, the maintenance of a mean arterial pressure of 80–90 mm/Hg reduced the rates of postoperative cognitive decline and delirium, suggesting that cerebral hypoperfusion/hypoxia contributes to changes in cognition. In our study, older age and lack of sleep were also identified as the risk factors for delirium. Previous studies [22–25] demonstrated that in unwell elderly individuals, the risk of delirium increased from 3% in those aged ≤65 years to 14% in those aged 65–74 years, with up to 36% of patients ≥75 years (p < 0.0001). Older age was also a risk factor amongst hospitalized individuals, with Pandharipande et al. [24] showing a higher incremental risk in those aged ≥65 years of transitioning to delirium by 2% for each year of life post-65 years (OR: 1.01, 95% CI = 1.00, 1.02, p = 0.03). These findings can be explained by a loss of neuronal function, changes in neurotransmitter systems, a loss of white matter integrity, a decreased regional cerebral blood flow, and a loss of neurochemical activity [26]. Besides, in patients with low sleep levels, delirium was frequent, suggesting the disruption of circadian rhythm as a possible cause for the onset [27–30]. Madrid-Navarro et al. [28] showed that exposure to continual noise, light and medication leads to poor sleep quality that ultimately causes delirium as a result of sleep disruption. The availability of drugs that can treat sleep disturbances in those who are critically ill is also sparse. Knauert et al. [29] suggested a range of multidisciplinary strategies to change the environment of the ICU and improve sleep and circadian rhythm, which may lead to a lower occurrence of delirium. It is therefore the responsibility of the healthcare professionals to provide evidence-based medicine in practice [31]. Prospective studies with larger sample sizes are needed to fully determine the specific risk factors for delirium [32,33].
Delirium is a complex disorder that is related to the severity of illness; environment; patient care; and iatrogenic factors. Considering the adverse impact of ICU delirium on critically ill patients, early identification is important to actively improve reversible risk factors. The effective participation of nurses and the treatment of underlying conditions that predispose patients to delirium can improve outcomes in patients receiving critical care [8]. There are no recommended preventive drugs or therapies for delirium. Non-drug interventions, including positive communication, early diagnosis in patients with psychological problems, family companionship, early mobilization therapeutic activities, optimization of hearing and vision, and improved sleep can improve patient support [34]. Patient outcomes may be improved by implementing preventive strategies for patients admitted to the ICU; early identification of the risk factors associated with delirium and taking positive corrective actions [35]. Despite the knowledge acquired to-date, everyday use of these therapies remains limited [36]. Delirium leads to poor long-term outcomes and high mortality rates as we observed that patients with delirium had longer times in the ICU and high rates of 28-day mortality. The prognosis of sepsis/shock patients with delirium was lower than those without, consistent with previous studies [9,22]. We previously showed comparable data [6] for patients with septic shock-associated delirium, in which more prolonged ICU stays and high mortality rates were observed. This may be related to the seriousness of the primary disease. In case of sepsis, long-term treatment is required to ameliorate the disease mediated neuronal cell damage, mitochondrial and endothelial dysfunction, a loss of neurotransmission, and altered neuronal Ca2+ homeostasis [37]. High mortality rates and long ICU stays have been reported as a result of extended resource consumption due to the high critical care burden [32]. Prolonged hospitalization can extend recovery times, increase the risk of patient falls, and heighten the risk of nosocomial infections amongst other undesirable effects [31]. Delirium experienced in the ICU can be long-lasting, with many survivors developing mental problems and subsequent cognitive impairment [17]. ICU patients with delirium struggle to separate fact from fiction and experience memory loss [19,38]. Attempts to understand the experience of ICU patients with delirium are therefore required to fully reveal its downstream consequences in surviving patients.
From our results, it was noteworthy that delirium did not influence the 28-day mortality for specific disease states. For example, the occurrence of delirium did not influence those with an abdominal disease. This may be explained by the fact that those with intestinal problems were treated with surgery and thus their disease was transient and rapidly treated, with no prolonged ICU stays required. This contrasted the findings of Raats et al. [39] who reported a regular occurrence of delirium in those undergoing abdominal surgery. It was further reported that delirium led to prolonged hospital stays, high mortality rates and the subsequent discharge to a nursing home. In contrast to other studies [40,41], we observed changes in the duration of mechanical ventilation time due to delirium in those with pulmonary disease. This may be explained by the occurrence of respiratory failure, lack of treatment efficacy, and the low number of patients analyzed in this disease subgroup.
Our study protocol had some limitations. First, this was single-center observational study and the number of ICU patients with delirium that were analyzed was small. Second, we evaluated delirium twice per day and if this occurred outside of the assessment time, misdiagnosis could result. Third, the subgroup of patients with cerebral diseases included patients with hypertensive intracerebral hemorrhage, ruptured aneurysm hemorrhage, subarachnoid hemorrhage, brain injury and other newly emerging cerebral diseases without previous mental system illness and cognitive disorders. Thus, we cannot rule out that these emerging cerebral diseases may affect the cognitive function. Finally, we did not perform an analysis of the long-term prognosis. Futher studies may be carried out with specific focus on each disease type in the ICU in larger patient cohorts to determine the causality and etiology of the risk factors for delirium.
5. CONCLUSION
The incidence of delirium and its associated risk factors varied according to disease type. The risk factors for delirium were found to be disease specific. However, older age and poor sleep quality were identified as common risk factors in most disease subgroups. While ICU delirium led to poor outcomes, with longer ICU stays and higher 28-day mortality, the highest 28-day mortality was associated with septic-shock associated delirium.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
Lina Zhang, Yuhang Ai, Meilin Ai, Li Huang, Qianyi Peng and Qing Feng contributed to the study conception and design. Lina Zhang, Yuhang Ai and Qianyi Peng performed the data analysis and interpretation. Qing Feng and Li Huang revised the manuscript for important intellectual content. Lina Zhang, Yuhang Ai, Li Huang, Qianyi Peng and Qing Feng gave final approval of the version to be published. All authors read and approved the final manuscript.
FUNDING
This work was supported by the
ABBREVIATIONS
- CAM-ICU,
confusion assessment method for the intensive care unit;
- CI,
confidence interval;
- IQR,
interquartile range;
- RASS,
Richmond Agitation Sedation Scale;
- PSQI,
Pittsburgh Sleep Quality Index;
- WBC,
white blood cell;
- Hb,
hemoglobin;
- PLT,
platelet;
- HCT,
hematocrit;
- PCT,
procalcitonin;
- ALB,
albumin;
- TBIL,
total bilirubin;
- DBIL,
direct bilirubin;
- ALT,
glutamic-pyruvic transaminase;
- AST,
glutamic-oxalacetic transaminase;
- BUN,
blood urea nitrogen;
- Cr,
creatinine;
- UA,
uric acid.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
We ensure that the research described has been carried out in accordance with the Ethical Principles for Medical Research Involving Human Subjects (Declaration of Helsinki) of the World Medical Association. Central South University, Xiangya Hospital Ethics Committee approval the study, all patients involved in the study are based on the principle of voluntary, and have signed an informed consent form. We will maximize the protection of the interests of patients, and will not cause harm to all patients.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Qing Feng AU - Yuhang Ai AU - Meilin Ai AU - Li Huang AU - Qianyi Peng AU - Lina Zhang PY - 2021 DA - 2021/02/13 TI - The Incidence and Prognosis of ICU Delirium: A Retrospective Study from a Single Center JO - Intensive Care Research SP - 16 EP - 23 VL - 1 IS - 1-2 SN - 2666-9862 UR - https://doi.org/10.2991/icres.k.210206.001 DO - 10.2991/icres.k.210206.001 ID - Feng2021 ER -
