Enhancing the role of pharmacists in the cascade of tuberculosis care
- DOI
- 10.1016/j.jegh.2016.05.001How to use a DOI?
- Copyright
- © 2016 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Pharmacies in low and middle income countries (LMICs) serve a broad role in health service delivery. Their high numbers, long hours of operation, absence of appointments and user fees, and strong community presence make them highly accessible and desirable points of care within communities that have limited access to more specialized or qualified medical services [1,2]. South Africa, for example, has approximately 20,000 pharmacy personnel distributed countrywide; India has over 600,000 [3]. In many settings, pharmacists remain the first and only health care provider that patients utilize [2]. Pharmacists can thus play an important role in facilitating optimal pathways to the care of tuberculosis (TB), a disease which affects over 9 million individuals every year.
In most high burden countries, despite the existence of national TB programs that provide free TB testing and treatment services, persons with symptoms suggestive of TB and notified TB patients more commonly access care from private providers, including pharmacists [4,5]. Surveys from India, Vietnam, Tanzania, and Uganda, show that 40–60% of TB patients approach pharmacies before visiting a diagnostic facility or medical practitioner [6–11]. Studies also show that pharmacists from high burden communities indicate strong support to participate in TB programs [12,13].
To date, however, pharmacists’ contributions have been restricted to their traditional role as ‘drug-dispensers’, that is to provide physician-prescribed treatment to notified TB patients, or at best to serve as treatment supervisors under the DOT (directly observed therapy) framework [13,14]. In reality, pharmacists can contribute to TB care and control in several ways (Fig. 1). However, their capacity to facilitate TB case detection, or to comprehensively support patients receiving treatment, remains underutilized [13,15–17].
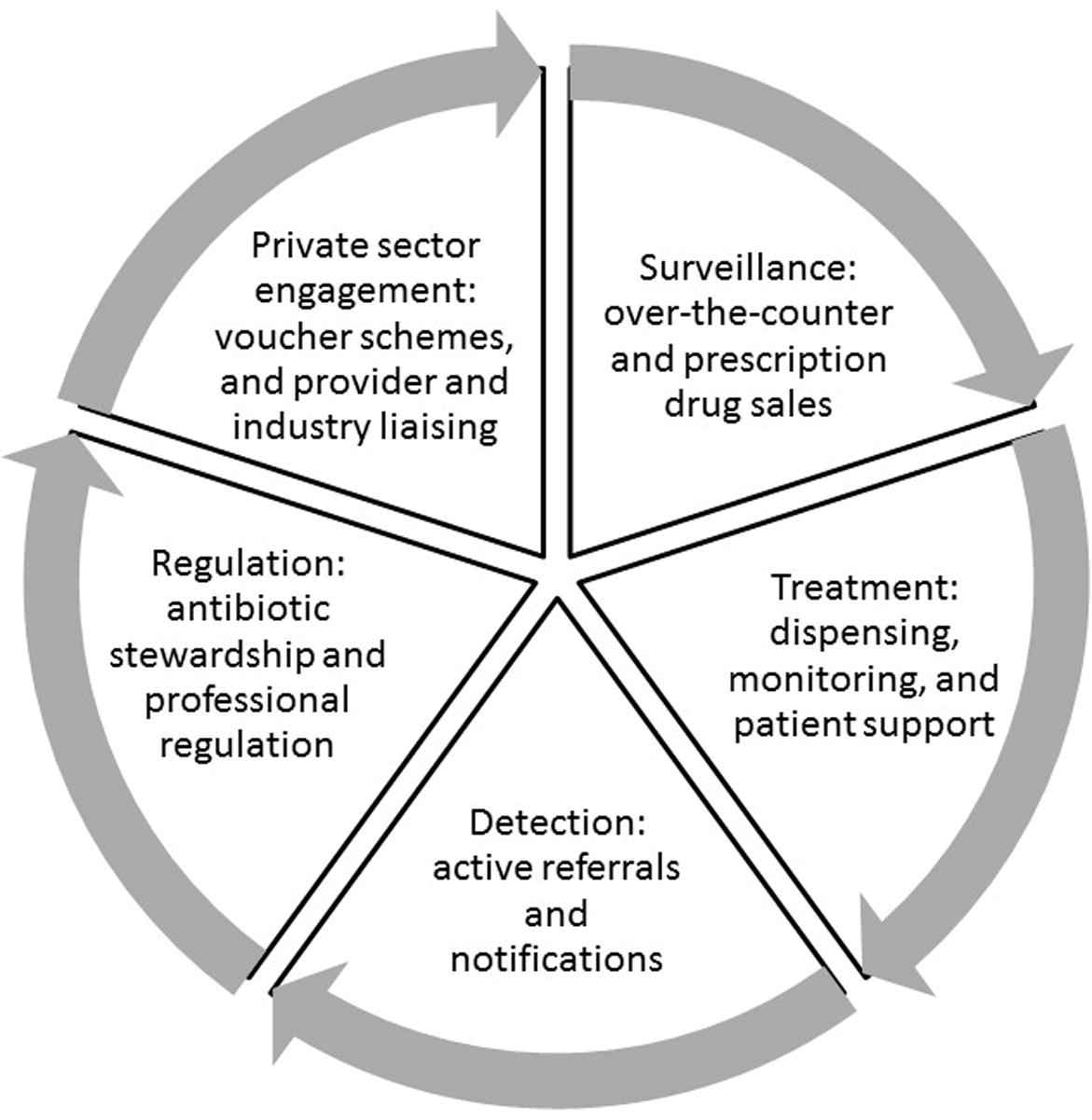
Pharmacists’ roles in tuberculosis care in low and middle income countries.
A number of intersecting factors challenge the engagement of pharmacists in TB detection and management within LMICs. First, pharmacists, among other provider groups, are implicated in TB diagnostic delay and drug-resistance by facilitating patient self-medication and antibiotic misuse [18,19]. Studies from India, Nepal, Cambodia, and Vietnam, show that pharmacists commonly dispense cough syrups, antibiotics (including anti-TB drugs), antihistamines, and bronchodilators to patients with chronic cough, without physician prescription, but rarely refer them for TB testing [20–24]. Pharmacists’ over-the-counter practices are no doubt driven by high consumer demand for rapid, symptomatic relief, coupled with patients’ disinclination to endure the time or cost of medical consultations, or suffer TB-related stigma [12,25]; pharmacists have reported high client attrition when referring symptomatic patients for TB care [17]. Nonetheless, the State of the World’s Antibiotic Report stresses alarming rates of nonprescription antibiotic use in LMICs as a result of poor antibiotic stewardship [18]. Private pharmacies in countries such as India are particularly worrisome, as they more often dispense newer broad-spectrum antibiotics such as fluoroquinolones compared with older antibiotics [18]. The overuse of fluoroquinolones has been directly linked to TB diagnostic delays and the development of drug-resistant TB [26].
Second, most pharmacies are private commercial entities that rely on a business model [1]. Referring TB symptomatic individuals for diagnostic services and forfeiting a drug sale, or encouraging notified patients to access free treatment via the national TB program may conflict with their basic mandate to earn revenues. Loss of income is recorded to be an important deterrent to pharmacists’ engagement in TB programs that fail to provide adequate retail compensation [16,17]. Indeed, economic incentives are shown to drive antibiotic overuse across the full hierarchy of health care providers, not just pharmacists, and even in professionally regulated settings [18].
This leads to the final challenge: pharmacies in most LMICs tend to be poorly regulated and are often run by laypersons with no formal education in pharmacy practice [1,27]. Low income countries have an average of 1.2 qualified pharmacists per 10,000 of the population, compared with 4.4 in middle income and 10.8 in high income countries [28]. That many LMICs have far greater numbers of pharmacies than qualified pharmacists further reflects the problem of inappropriate supervision of drug-related services in TB affected communities [28]. Small-scale surveys from India and Laos, for instance, reveal that fewer than 15% of staff working within chemist or drug shops have any training or qualification in pharmacy [29,30]. While strict policies are in place to ensure provider competence, curtail over-the-counter prescription drug sales, and sustain the division of tasks between pharmacists and physicians in industrialized countries, these practices differ dramatically in settings that lack professional regulatory enforcement.
This has important implications for efforts to utilize pharmacists in TB care provision within LMICs. Clearly, there is a need to train and educate pharmacy providers, including those who lack formal qualification, in TB prevention and treatment, with specific guidance on symptom screening, referral, and treatment support. Pharmacists also need to be educated on antibiotic stewardship and the need to avoid dispensing anti-TB drugs and other antibiotics without prescriptions. Education alone, however, is unlikely to change pharmacist behaviors [31–33]. There is a parallel need to regulate, or at minimum, monitor current practices in order to build basic pharmacy competency, and foster a sense of professionalism and accountability.
A paradigm shift is thus needed to engage and strengthen the role of pharmacists in improving TB care and control in LMICs. We have identified several roles that pharmacy providers can play to constructively contribute to the cascade of TB care (Fig. 1). In order to realize this potential, national TB programs and other stakeholders in LMICs need to engage and work with professional pharmacy associations and trade organizations, and adopt multipronged interventions that combine education and peer-influence strategies with regulatory enforcement [32,33]. There is also a strong argument to be made for investing in public–private partnerships that respond to pharmacists’ profitmaking needs while promoting the optimal delivery of health care services. Creative contractual engagements with private pharmacy owners in South Asia have led to significant improvements in TB notification and treatment completion rates, with tangible impacts at the global level [1,4,34–36]. The increase in global TB notifications in 2014—the first measureable increase since 2007—was largely attributed to successful collaborations between private providers and the public sector in India, via private provider interface agency models in urban pilots that included pharmacy providers [37,38]. There is great potential to scale-up the engagement of pharmacies in similar social businesses and franchising models, health insurance schemes, regulatory regimes, and social protection initiatives to maximize their role in TB care.
Conflicts of interest
None declared.
Acknowledgements
The authors are grateful for grant support from the IC-IMPACTS Centres for Excellence.
References
Cite this article
TY - JOUR AU - Amrita Daftary AU - Nita Jha AU - Madhukar Pai PY - 2016 DA - 2016/05/31 TI - Enhancing the role of pharmacists in the cascade of tuberculosis care JO - Journal of Epidemiology and Global Health SP - 1 EP - 4 VL - 7 IS - 1 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2016.05.001 DO - 10.1016/j.jegh.2016.05.001 ID - Daftary2016 ER -
