Trends in lung cancer incidence in Lebanon by gender and histological type over the period 2005–2008
- DOI
- 10.1016/j.jegh.2017.04.003How to use a DOI?
- Keywords
- Lung cancer; Trends; Adenocarcinoma; Squamous
- Abstract
Introduction: Lung cancer incidence rates, overall and by histologic subtypes, vary substantially by gender and smoking. This study’s aim was to review data regarding trends in the number of cases of different lung-cancer histologies and relate these to smoking habits by gender in Lebanon.
Materials and methods: Lung cancer data using ICD-O, 3rd edition, from the Lebanese National Cancer Registry from 2005 to 2008 were stratified by gender for histology type for patients aged over 18 years.
Results: Lung cancer cases among males were 2.5 times higher than those in females. The most common lung cancer histology type for males and females was adenocarcinoma for all observed years. The proportion of squamous cell carcinoma in incident cases was significantly higher in males than in females for the total period from 2005 to 2008, P = 0.032, but not in individual years. The ratio of adenocarcinoma to squamous cell carcinoma in incident cases between 2005 and 2008 was 2:45 for males and 3:15 for females.
Conclusion: Lung cancer histology in Lebanon is following a pattern similar to that found in most countries of North America and in Europe, where adenocarcinoma is the most prevalent subtype among both males and females.
- Copyright
- © 2017 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Introduction
Lung cancer is the most common cause of cancer-related death among both sexes combined [1]. The incidence rates of this disease have increased dramatically in developing countries, particularly in the Arab world, where tobacco consumption among both sexes continues to rise. Currently, around half of lung cancer cases occur in developing countries, whereas in the 1980s, developing countries contributed to around 31% of cases [2]. In the United States and Europe, rates of smoking among males have decreased, thus resulting in decreased lung cancer incidence, while increased smoking among females since the 1970’s has increased the incidence of female lung cancer in these countries [2,3].
Lebanon is a small middle-income country on the Eastern Mediterranean shore with a population of around 4 million Lebanese citizens, 1 million Syrian refugees, and half a million Palestinian refugees. It is at the third stage of its demographic transition characterized by a decline in both fertility and mortality rates [4]. According to the United Nation’s World Population Prospects, the average life expectancy in Lebanon will rise from 71 to 78.7 years between 2009 and 2050, leading to an increase in the median population age from 28.8 to 41.7 years as well as the percentage of older population aged 60 years and above from 10.3% to 25.8%. Data from World Health Organization (WHO) Globocan 2012 have shown that in the Arab world, Lebanon has the highest lung cancer incidence in females and the third highest in males (Table 1). According to the National Cancer Registry (NCR) of Lebanon, lung cancer incidence from 2003 to 2008 remained relatively stable among males ranking second behind prostate cancer, but increased among females, for which it ranks third behind breast and colon cancer [5].
| Smoking Males% | Smoking Females% | ASR (W) 100,000 (males) | ASR (W) 100,000 (females) | Data quality indicator | |||
|---|---|---|---|---|---|---|---|
| Quality | Regional or national | Coverage | |||||
| Eastern Mediterranean | |||||||
| Egypt | 40 | <1 | 11.2 | 3.8 | High-quality* | Regional | Lower than 10% |
| Bahrain | 34 | 8 | 21.3 | 8.5 | High-quality* | National data or high quality regional | Greater than 50% |
| Iraq | 26 | 3 | 24.2 | 6.6 | Frequency data | ||
| Jordan | 47 | 6 | 27.0 | 4.1 | National data (rates). | ||
| Kuwait | 35 | 4 | 9.9 | 4.8 | High-quality* | National data or high quality regional | Greater than 50% |
| Lebanon | 46 | 31 | 30.2 | 11.0 | National data (rates). | ||
| Libya | 47 | <1 | 28.0 | 3.7 | High-quality* | Regional | Lower than 10% |
| Syria | 42 | N/A | 25.5 | 5.3 | No data, estimated from neighboring countries | ||
| Morocco | 33 | 2 | 25.5 | 2.8 | Regional data (rates) | ||
| Oman | 12 | <1 | 6.7 | 2.8 | High-quality* | National data or high quality regional | Greater than 50% |
| Saudi Arabia | 24 | 1 | 7.3 | 2.7 | National data (rates). | ||
| Tunisia | 58 | 5 | 31.1 | 1.7 | High-quality* | Regional | Lower than 10% |
| UAE | 19 | 2 | 11.2 | 5.2 | National data (rates). | ||
| Yemen | 35 | 11 | 6.4 | 1.7 | Regional data (rates). | ||
| Southern Europe | |||||||
| Italy | 33 | 19 | 38.5 | 13.1 | High-quality* | Regional | Lower than 10% |
| France | 36 | 27 | 52.0 | 20.2 | High-quality* | Regional | Between 10% and 50% |
| Greece | 63 | 41 | 50.9 | 9.0 | No data | ||
| Spain | 36 | 27 | 52.5 | 11.3 | High-quality* | Regional | Between 10% and 50% |
| Northern Europe | |||||||
| Norway | 28 | 26 | 34.8 | 26.1 | High-quality* | National data or high quality regional | Greater than 50% |
| Sweden | 24 | 24 | 19.4 | 19.1 | High-quality* | National data or high quality regional | Greater than 50% |
| United Kingdom | 25 | 23 | 34.9 | 25.9 | High-quality* | National data or high quality regional | Greater than 50% |
| Germany | 33 | 25 | 38.8 | 17.9 | High-quality* | Regional | Between 10% and 50% |
| Eastern Europe | |||||||
| Turkey | 47 | 15 | 63.9 | 8.8 | High-quality* | Regional | Lower than 10% |
| Croatia | 36 | 30 | 58.2 | 15.4 | High-quality* | National data or high quality regional | Greater than 50% |
| Poland | 38 | 27 | 60.5 | 21.8 | High-quality* | Regional | Lower than 10% |
| Romania | 38 | 18 | 58.8 | 11.2 | Regional data (rates) | ||
| North America | |||||||
| US | 33 | 25 | 44.2 | 33.7 | High-quality* | National data or high quality regional | Greater than 50% |
Data included in Cancer incidence in Five Continents (CI5) volume IX and/or X.
Prevalence of adult smoking by gender from selected eastern Mediterranean and European countries and the United States, WHO, 2009 and Age-standardized rates to the world population ASR (W), rates stratified per gender per 100,000, Globocan (2012).
Trends in lung cancer incidence are largely the product of changing smoking prevalence and patterns of tobacco consumption. The most common forms of tobacco smoking in Lebanon are cigarettes or waterpipe smoking, which is gaining popularity, particularly among females [6]. A recent study has shown that waterpipe smoking generates ambient carcinogens and toxicants equivalent to 2–10 cigarettes in 1 h of use [7]. Adult smoking in Lebanon is estimated at 38.5% (males at 46% and females at 31%) [8]. Smoking prevalence among the youth is estimated to be among the highest worldwide (65.8% for boys and 54.1% for girls), with waterpipe smoking the major form of smoking (33.9%) followed by cigarette smoking (8.6%) [8].
In addition to smoking, urban air pollution measured by concentrations of particulate matter <10 µm in size (PM10) exceeds the levels set by WHO (20 µg/m3) in most urban Lebanese cities [9].
Smoking rates among Lebanese females are the highest in the Mediterranean and Arab region and are rising at a higher pace than those observed in neighboring countries [10–12]. Currently, the incidence of lung cancer among females remains lower than that of males [5]; however, it is expected to increase in the future since incidence of lung cancer closely reflect patterns in smoking prevalence from 20 to 30 years earlier due to the long latency period between the time of smoking initiation until diagnosis [13,14].
Lung cancer incidence rates, overall and by histologic subtypes, vary substantially by gender and smoking [15–17]. Different proportions of histology types were reported among males and females, mainly confirming the close relationship between smoking and squamous cell carcinoma. Here, we present from the NCR in Lebanon the percentage of lung cancer cases for each of the common histology types by gender from 2005 to 2008. We also relate patterns of smoking to lung cancer cases and compare lung cancer histology by gender to the west and the Arab world.
2. Materials and methods
Lung cancer data (C-33 and C-34) using ICD-O, 3rd edition, from the Lebanese NCR yearly incidence from years 2005 to 2008 were stratified by gender for histology type for adult patients aged over 18 years. The NCR was established in 1995; however, the first data collection was initiated in 2003. The NCR relies on both a capture and a recapture system. The former relies on physicians’ routine reporting of cancer cases collected from clinics in addition to the ministry of health drug dispensing center distribution, while the latter relies on gathering information from histopathologic and hematologic laboratories. In 2004, there were 17 reporting sites for the recapture system. The information includes cancer site, date of diagnosis, morphology, stage, TNM classification, and grade. For the interest of this study and best data quality, lung cancer incidence data from 2005 to 2008 were retrieved, as data from subsequent years are not yet publicly available. Histologic groups were stratified as non-small cell squamous and adenocarcinoma, small cell, large cell, other non-small cell, and sarcoma. The proportion of patients with adenocarcinoma and the squamous cell carcinoma was compared by gender using the two-sided population proportions test; a P value of <0.05 was considered significant (Table 2 ). The ratio of adenocarcinoma: squamous cell carcinoma was calculated by dividing the number of adenocarcinomas by the number of squamous cell carcinomas. The resulting ratio, reflecting the magnitude of the difference between adenocarcinoma and squamous cell carcinoma, was compared among males and females by year.
| Males N (%) | Females N (%) | P-value | ||
|---|---|---|---|---|
| 2005 | SCC | 81 (16.1) | 23 (11.6) | 0.131 |
| Adenocarcinoma | 230 (45.8) | 93 (47.0) | 0.771 | |
| 2006 | SCC | 79 (13.6) | 31 (12.9) | 0.787 |
| Adenocarcinoma | 266 (45.6) | 105 (43.6) | 0.603 | |
| 2007 | SCC | 121 (19.5) | 35 (15.0) | 0.128 |
| Adenocarcinoma | 282 (45.4) | 117 (50.0) | 0.230 | |
| 2008 | SCC | 122 (21.0) | 46 (18.0) | 0.317 |
| Adenocarcinoma | 230 (39.5) | 110 (43.1) | 0.327 | |
| 2005–2008 | SCC | 403 (17.6) | 135 (14.5) | 0.032 |
| Adenocarcinoma | 1008 (44.1) | 425 (45.8) | 0.378 |
Number and percentage of lung cancer histology in males and females, from yearly incident lung cancer cases in 2005–2008, Lebanon, NCR.
3. Results
The most common histology type reported was non-small cell adenocarcinoma for all years 2003–2008 in all cases (Fig. 1 ). Adenocarcinoma accounted for 57% and 61% for years 2003 and 2004, respectively. A decrease was observed in subsequent years, with the proportion ranging from 41% to 44% until 2008; however, it remained the predominant histology subtype, doubling the next most common category, squamous cell carcinoma (Fig. 1). The relative proportion of lung cancer cases by histology among males and females was comparable in Lebanon between 2005 and 2008, as shown in Table 2. Histology type proportion did not vary by gender by year; however, the proportion of squamous cell carcinoma was significantly higher in males than in females for the total period extending from 2005 to 2008, with a P = 0.032, but not in individual years (Table 1). As for adenocarcinoma, males and females kept a comparable proportion at individual years and over the period (2005–2008).
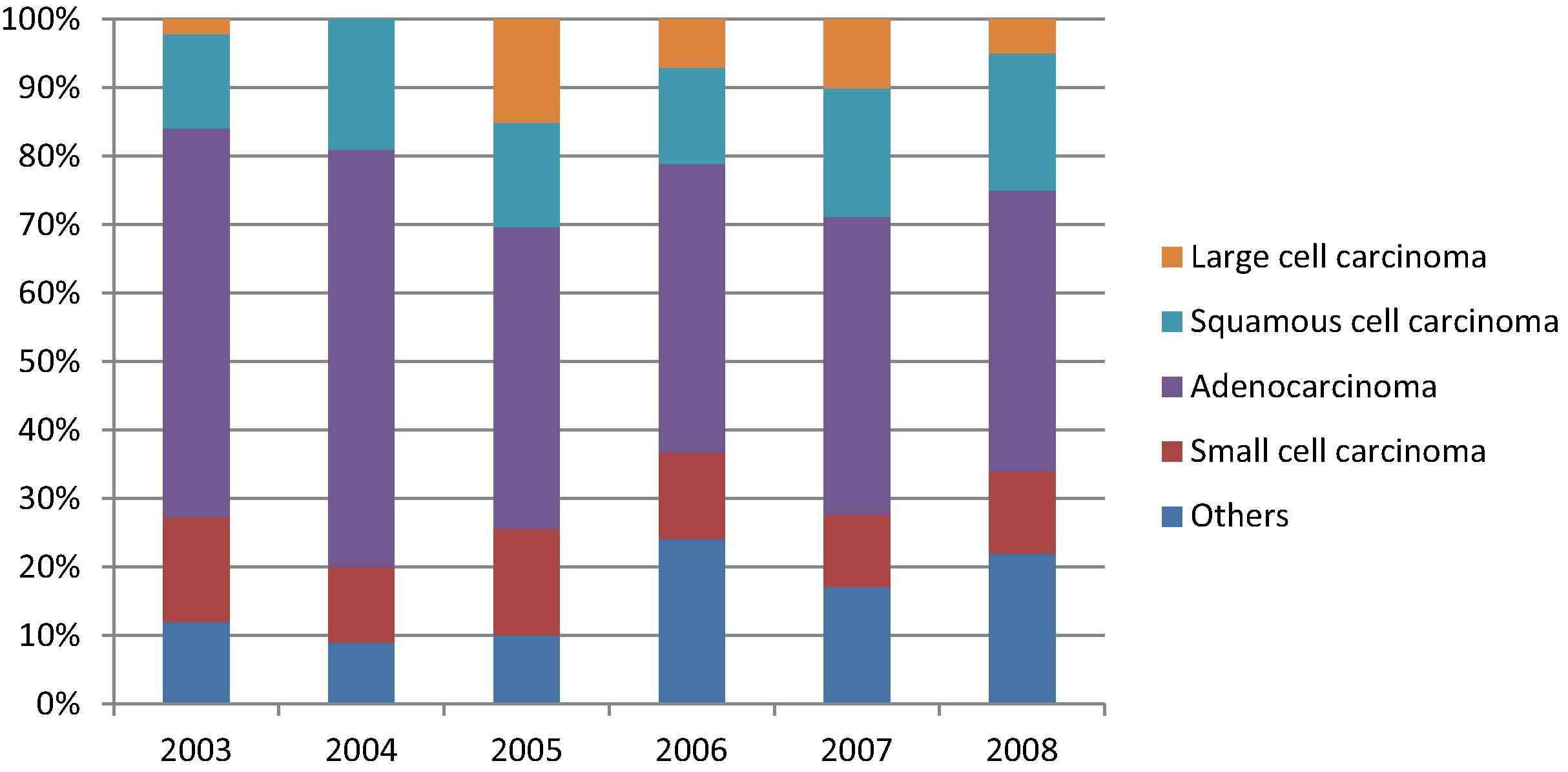
Percentage of lung cancer histology for both males and females from the total or yearly incident lung cancer cases 2003–2008, Lebanon, NCR.
3.1. Lung cancer incidence trends in males
Between 2005 and 2008, 2288 lung cancer cases were reported among males, of which 1008 cases were non-small cell adenocarcinomas and 403 cases were non-small cell squamous carcinomas. Adenocarcinomas had the highest incidence in males, followed by other non-small cell carcinomas, squamous cell carcinomas, small cell carcinomas, unspecified carcinomas, large cell carcinomas, and sarcomas. Adenocarcinoma cases remained relatively stable during 2005, 2006, and 2007, during which they accounted for about 45% of lung cancer cases and then decreased to 39.5% in 2008 (Fig. 2 and Table 2). Squamous lung cancers accounted for 16.1% of lung cancer cases in 2005 then decreased to 13.6% in 2006. In 2007, squamous lung cancer cases increased to 19.5% and then to 21% in 2008 (Fig. 2).
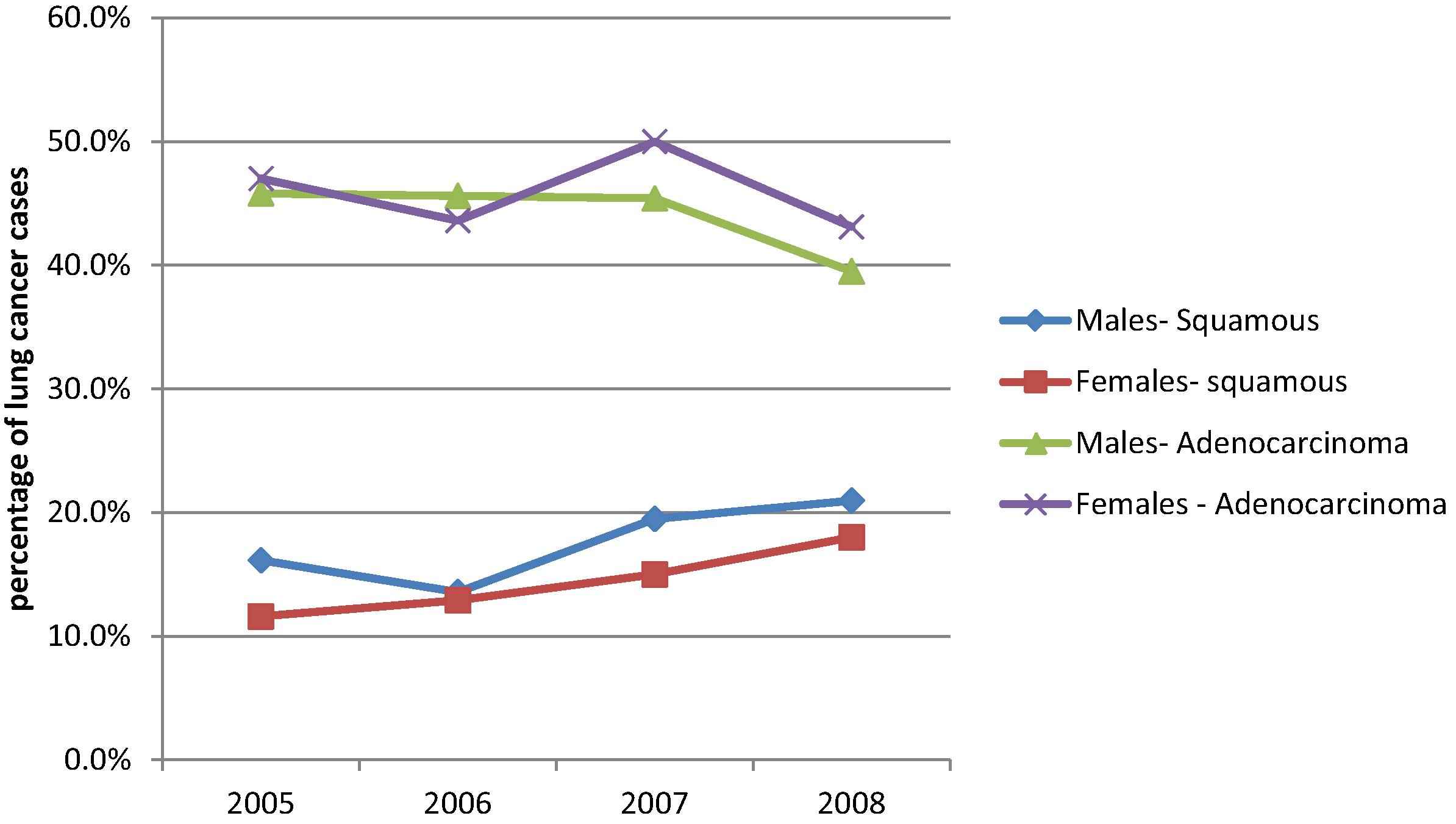
Percentage of lung cancer histology by gender from yearly lung cancer incidence cases in 2005–2008, Lebanon, NCR.
3.2. Lung cancer incidence trends in females
Between 2005 and 2008, 928 lung cancer cases were reported among females of which 425 cases were non-small cell adenocarcinomas and 135 cases were non-small cell squamous carcinomas. Adenocarcinomas are also the most common type, followed by other non-small cell carcinomas, squamous cell carcinomas, small cell carcinomas, unspecified carcinomas, sarcomas, and large cell .carcinomas. Adenocarcinomas accounted for 47% of lung cancers among females in 2005 and = − decreased to 43.1% in 2008 (Fig. 2). Squamous cell carcinomas increased gradually from 11.6% in 2005 to 18% in 2008 (Fig. 2).
3.3. Ratio of adenocarcinomas:squamous cell carcinomas
The ratio of adenocarcinomas: squamous cell carcinoma between 2005 and 2008 was 2:45 for males and 3:15 for females over the study period. As shown in Fig. 3 , and further elucidated in Table 2, females maintained a higher proportion of adenocarcinoma than males over the study period, yet the difference was not significant.
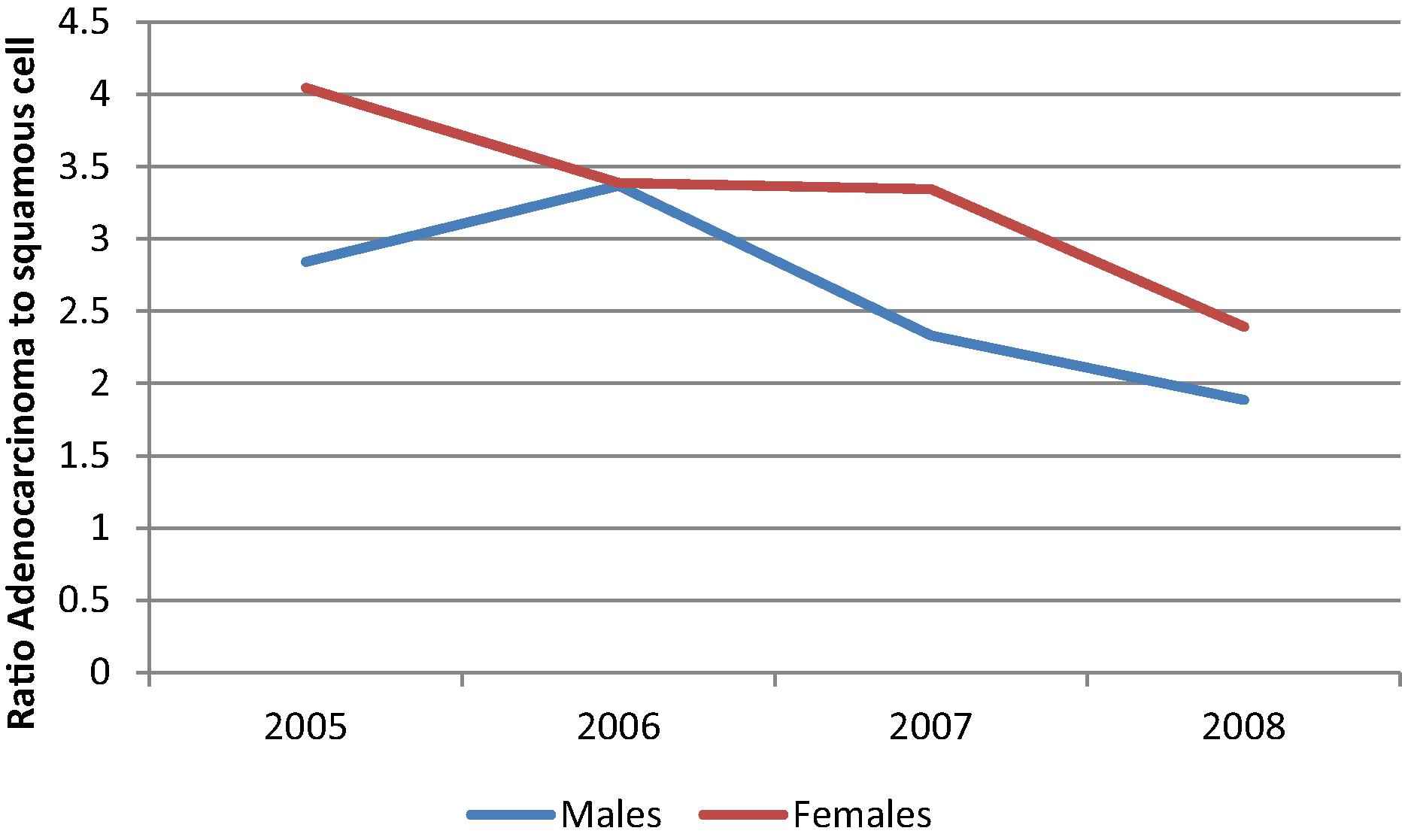
Ratios of Adenocarcinoma:Squamous cell carcinoma by gender 2005–2008, Lebanon, NCR.
Ratios illustrated in Fig. 3 showed that females maintained a higher proportion of adenocarcinoma compared to squamous cell carcinoma than males except for in 2006 (Figs. 2 and 3). Over the study period, the total number of male lung cancer cases was around 2.5 times the number of female lung cancer cases. While the proportion of adenocarcinoma in females did not show a decreasing trend over the study period, the observed decreasing trend is due to a gradual increase in proportion of squamous cell carcinoma in females from 11.6% in 2005 to 18% in 2008. A similar increase in squamous cell carcinoma was observed among males for the same period, with 16.1% in 2005 to 21% in 2008.
4. Discussion
Data from the Ministry of Public health in Lebanon revealed a higher lung cancer incidence among males than females approximating a 2.5 times higher incidence (2288 male cases versus 928 female cases). Specifically, non-small cell squamous cancer incidence among males is 3 times higher than that among females (403 versus 135 cases), which is likely to be secondary to the higher smoking prevalence among males. Our data are limited to a study period from 2005 to 2008; therefore, the trends observed over this brief period cannot be conclusive enough to make any speculations on future trends. The rapid change in squamous cell carcinoma may be a surrogate marker of smoking habits; though smoking increases the risk of both histological types, the relative risk associated with smoking is much higher for squamous cell carcinoma than for adenocarcinoma, so that in smokers squamous cell carcinoma rates are higher than adenocarcinoma rates [18,19]. The gradual increase in males and females noted in squamous cell carcinoma over the study period is to be observed over the coming years to test the significance of this trend.
Our results have, however, confirmed that the proportion of adenocarcinoma is greater than the proportion of squamous cell carcinoma for all years in both genders, especially in females. Adenocarcinoma was observed in both smokers and nonsmokers (including ex-smokers), yet adenocarcinoma risk decreases less rapidly after smoking cessation compared to other histology types [20]. This high proportion of adenocarcinoma is a legacy of smoking habit in the Lebanese population in both genders over the past two to three decades. A study conducted by Saade et al. in 2008 revealed that the smoking incidence among females has risen, and now smoking among males is only 1.5 times higher than smoking among females [8]. Similarly, the WHO report on the global tobacco epidemic in 2013 revealed that the relative smoking incidence among males is around 1.3 times higher than that of females. These data suggest that in a 20-year period, the relative incidence of lung cancer among females is expected to increase. However, even if smoking rates among females surpasses those of males in the future, the incidence of lung cancer among females is less likely to exceed that of males according to a systematic review and meta-analysis of 47 articles containing 404,874 individuals, which revealed that male smokers had a 61% higher risk of lung cancer than female smokers [21]. The incidence of smoking among Lebanese females is the highest in the Eastern Mediterranean region [8], and these high smoking rates have resulted in the highest incidence rates of lung cancer among females in the Mediterranean region.
According to Globocan 2012, the incidences of lung cancer cases in Lebanon among both males and females is lower than in countries of Eastern, Northern, and Southern Europe as well as North America, where the smoking rates are lower than in Lebanon (Table 1). These discrepancies in incidences of lung cancer cases between Lebanon and Western countries might be attributed to the Mediterranean diet compared to Western diets. Several studies have identified diet as a protective factor for lung cancer. For instance, the incidence of tobacco-related cancers of lung, mouth, and pharynx tend to be low amongst migrants from the Mediterranean region than Australian-born men, which has been attributed to the healthier dietary habits, which may protect against these epithelial cancers [22].
As shown in Fig. 4 , among many countries of the Arab region such as Egypt [23], Palestine [23], Jordan, and Arab Gulf Cooperation Council countries [24], squamous cell carcinoma and adenocarcinoma show approximately the same proportions in males, with a tendency for squamous cell carcinoma to be higher, while adenocarcinomas tend to be the predominant histologic type among females [25]. In Algeria and Tunisia, the major histologic type of lung cancer is squamous cell carcinoma in males [23]. Among Algerian females, the major histologic type is also squamous cell carcinoma, while in Tunisian females, both histologic types show approximately the same proportions [23]. Similarly, a study from Pakistan over the period of 2003–2008 concluded that nearly half the lung cases in males and a third of females were squamous cell carcinoma. A statistically significant increase in squamous cell carcinoma was noted over the study period in both genders [26]. Similar proportions of squamous cell lung cancer were found from a national registry in Poland, including more than 20,000 patients from 1995 to 1998, with 55.2% for males and 32.5% for females. Females had more adenocarcinoma, yet the most prevalent form remained squamous cell carcinoma. Smoking patterns revealed less smoking in patients with adenocarcinoma in both genders [27]. These results further suggest that smoking habits and exposure to smoking in nonsmokers predicted lung cancer histology in these groups. Specifically, Turkey seems to have a similar proportion of adenocarcinoma cases (46%) [28] among females as those seen in Lebanon, with adenocarcinoma being the most common histologic subtype among both sexes [29].
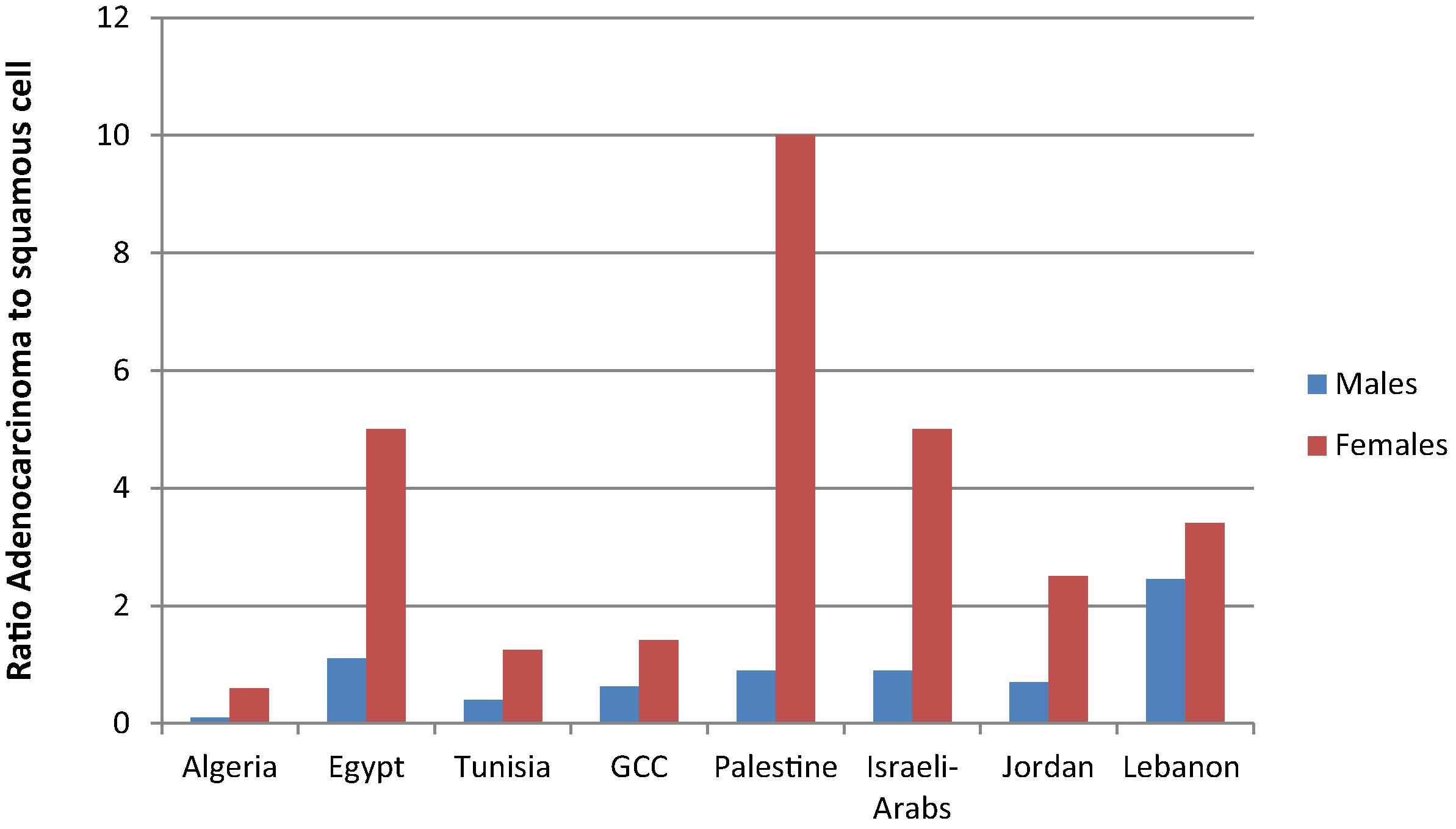
Ratios of Adenocarcinoma:Squamous cell carcinoma by gender, Lebanon (2005–2008), Lebanon (2005–2008), Arab world (1998–2005).
In our study, the ratio of adenocarcinoma to squamous cell carcinoma was higher in females (3:15) than in males (2:45). Fig. 5 reveals that the ratio of adenocarcinoma to squamous cell carcinoma is higher in females than in males in western countries, yet this ratio is higher among Lebanese females. The increase in adenocarcinoma cases among females could be directly attributed to increased smoking rates. However, adenocarcinoma remains the most common histologic type among females; thus, factors other than smoking could be influencing this pattern. In fact, hormonal factors, particularly exogenous and endogenous estrogens, have been shown to play a role in the development of adenocarcinoma [30]. Hormonal replacement therapy among women has led to increased cases of adenocarcinoma in several studies, suggesting a role for gender in susceptibility to developing adenocarcinoma [30,31].The general trend observed in females over the past 20 years in the United States showed that adenocarcinoma rates were increasing, while squamous cell carcinoma rates were decreasing. In never smokers in Europe, the United States, and Asia, females were found to have a higher incidence of lung cancer compared to males [17].
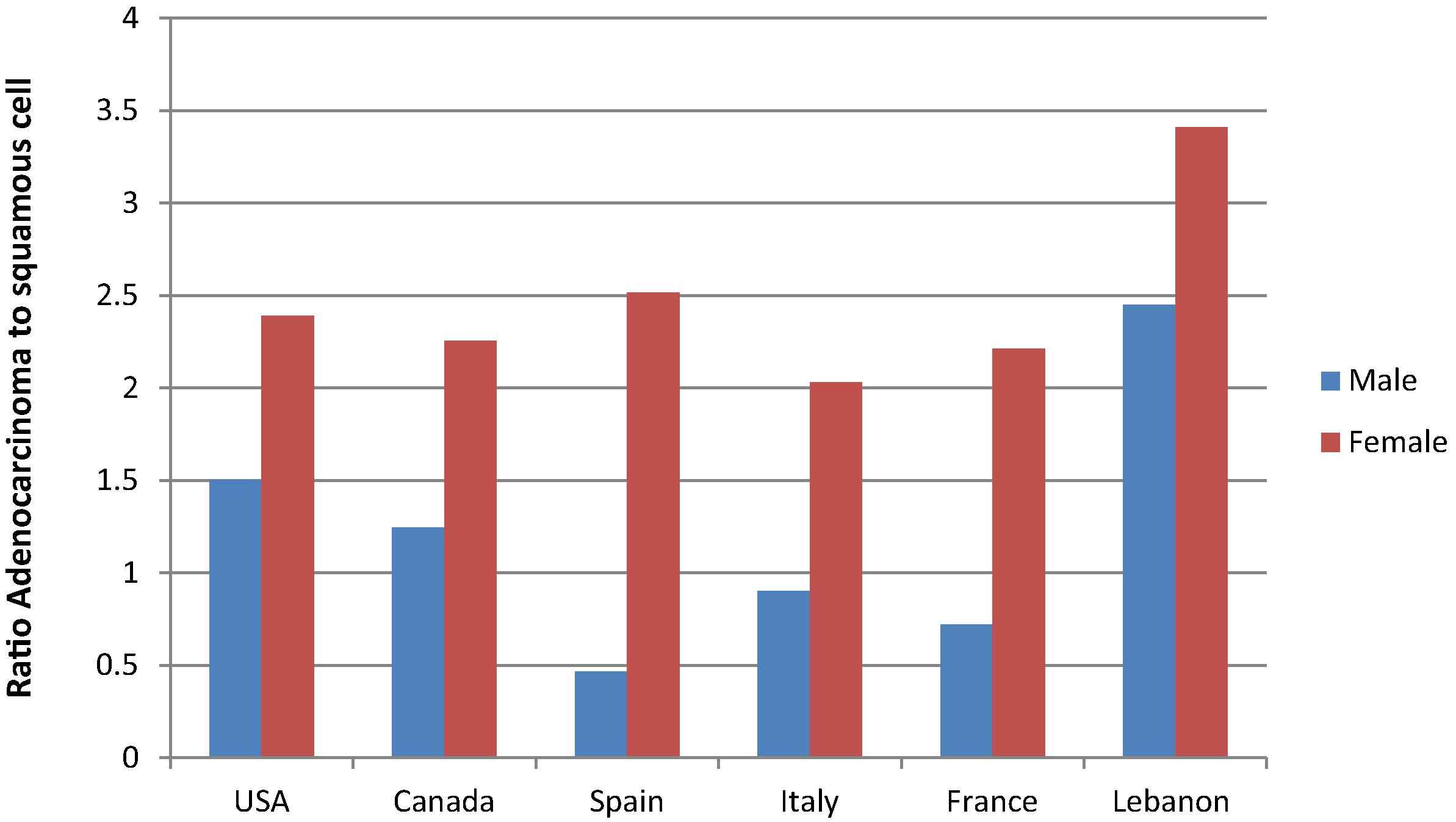
Ratios of Adenocarcinoma:Squamous cell carcinoma by gender, Lebanon (2005–2008), EU/ North America (1978–2002).
In men, lung cancer rates have been declining overall and by subtype around the world since the beginning of the study period (1978–2002), except for adenocarcinoma [20]. In Europe, Oceania, and North America, a different histologic distribution among females and males exists compared to the Arab region. In males, squamous cell carcinoma was the most common subtype, but rates started decreasing and adenocarcinoma rates started to stabilize during the mid-1980s in North America, Australia, and Iceland; however, they were the most common subtype in recent years in all countries except for France, Spain, and The Netherlands [20]. In females, adenocarcinoma was the most common except in The Netherlands, and rates for this histologic type are still increasing in Austria, France, Iceland, Italy, the Netherlands, Spain, and Switzerland [20,32]. According to the Surveillance, Epidemiology, and End Results data in the United States from 1973 to 2010, adenocarcinomas were constant in males and increased for females, whereas squamous cell carcinomas decreased for both genders [16]. Thus, adenocarcinoma is currently the most common histologic type among both sexes in developed countries, while rates are still increasing among females, which resemble the patterns observed in Lebanon but not yet in the rest of the Arab world. Early signs of a decline in adenocarcinoma can, however, be observed in Canada, Denmark, and Australia among females younger than 60 years [20].
5. Conclusions
Analysis of data from the Lebanese National Cancer Registry have shown that lung cancer histology in Lebanon is following a pattern similar to that found in most countries of North America and in Europe. As a result of well-established smoking habits among the Lebanese female population, lung cancer cases among females are still significantly higher than in the rest of the Arab world. Adenocarcinoma is the most prevalent subtype among both males and females, having a different pattern than that seen in most Arab countries where squamous cell carcinoma is the predominant subtype among males. Lebanon has the highest incidence of lung cancer among females and is the third highest among males in the Arab region. Despite some efforts in raising awareness about the dangers of smoking, specifically in schools, and in banning smoking in closed areas, smoking prevalence remains high and is expected to continue increasing among females. Data on young Lebanese smokers revealed that females have increased their smoking rates and might soon surpass those of males. Thus, smoking cessation and preventive actions against smoking initiation are evidently still needed. Urgent solutions have yet to be found for the smoking endemic in Lebanon, with more efforts placed at raising awareness particularly among young people.
Contribution
ST conceived the research idea and wrote the paper. MC performed the statistical analysis and reported the results. DM reviewed and edited the manuscript. AS analyzed and interpreted the data.
Acknowledgements
None.
References
Cite this article
TY - JOUR AU - Sally Temraz AU - Maya Charafeddine AU - Deborah Mukherji AU - Ali Shamseddine PY - 2017 DA - 2017/04/29 TI - Trends in lung cancer incidence in Lebanon by gender and histological type over the period 2005–2008 JO - Journal of Epidemiology and Global Health SP - 161 EP - 167 VL - 7 IS - 3 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2017.04.003 DO - 10.1016/j.jegh.2017.04.003 ID - Temraz2017 ER -
