Symptoms and risk factors for stroke in a community-based observational sample in Viet Nam
- DOI
- 10.1016/j.jegh.2012.06.001How to use a DOI?
- Keywords
- Stroke; Symptoms; Viet Nam; Community-based; Risk factors
- Abstract
Background: Viet Nam is experiencing a health transition from infectious to chronic disease. Data on cardiovascular diseases, including strokes, are limited.
Methods: Data were randomly collected from six communities in Da Nang, Viet Nam, on participant demographics, medical history, blood pressure, anthropometrics and health behavior using World Health Organization (WHO) guidelines. Stroke symptoms were collected by self-report with the standardized Questionnaire for Verifying Stroke Free Status. Multivariate logistic regression was used to identify factors associated with the presence of stroke symptoms.
Results: One thousand six hundred and twenty one adults were examined with a mean age of 52.0 years (±12.5 years), of which 56.1% were women. 27.3% of the participants were found to have hypertension, 26.2% used tobacco, and 16.1% were overweight. More than two-thirds of the participants with hypertension were unaware of their condition. Almost one fourth of the participants were identified by the questionnaire as previously experiencing at least one stroke symptom. Age, rural residence, and education were associated with the presence of stroke symptoms. Models adjusted for demographics found hypertension, high cholesterol, reported severe chest pain, former smoking, and being overweight to be associated with a higher prevalence of stroke symptoms.
Conclusions: The high frequency of stroke symptoms in Da Nang calls for further evaluation and interventions to reduce hypertension and other risk factors for chronic disease in Viet Nam and other health transition countries.
- Copyright
- © 2012 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- Open access under CC BY-NC-ND license. http://creativecommons.org/licenses/by-nc-nd/4.0/
1. Introduction
By the year 2030, stroke will account for the highest percentage of disability-adjusted life years worldwide [1] reaching epidemic proportions [2]. Low- and middle-income countries have the largest burden of stroke, accounting for more than 85% of stroke deaths globally [2,3]. Developing countries such as Viet Nam are currently experiencing a health transition from infectious to chronic diseases in which the impact on the health of the population from chronic diseases will be especially devastating. The need to develop population-based studies to evaluate stroke prevalence, incidence and risk factors is imperative [4,5].
The prevalence of key risk factors, such as smoking [6], hypertension [7–9] and body mass index (BMI) [10,11], for stroke is high and is increasing in Viet Nam. Documenting the incidence of stroke in countries such as Viet Nam is difficult because patients with mild or transient symptoms may not present to hospitals or clinics for diagnosis, and longitudinal studies following patients for incident cerebrovascular disease are expensive and rarely done. A practical solution to identify persons at high risk for stroke involves the collection of stroke symptoms. In developed countries it has been postulated that a high proportion of such symptoms outside of a diagnosed stroke or transient ischemic attack (TIA) may be indicative of “silent” or “whispering” strokes—those that are not severe enough to motivate the individual to consult a physician or, if clinical care was sought, symptoms were not defined well enough to result in a proper diagnosis [12,13]. This may be even more relevant in resource-poor countries where access to health care can be more difficult.
The present study was initiated in collaboration with the Da Nang Department of Health (DOH) to establish a cohort of randomly selected participants to focus on stroke risk and symptoms. The aims of this study were to: (1) describe self-reported and measured risk factors in a community-based study of residents in Da Nang Province; (2) document stroke symptoms occurring in the community; and (3) determine factors that are associated with the prevalence of stroke symptoms in the sample.
2. Methods
2.1. The sample
Da Nang Province is located in the central part of Viet Nam, approximately 700 km south of Ha Noi and 1000 km north of Ho Chi Minh City. It encompasses 1255 km2 and has a population of 887,100 people (2009 census). The Province is geographically divided into mutually exclusive units in several layers based on administrative and geographic characteristics. In Da Nang there are seven districts subdivided into 56 communes (similar to a U.S. county), which are further subdivided into hamlets (villages or towns). The communes are characterized according to their urbanicity by the Vietnamese government, ranging from 100% urban to 100% rural. This designation was used to classify communes into urban or rural to distinguish lifestyles. A commune was designated as half rural/half urban if it had more than 30% agricultural land and respective farm workers. In Da Nang, the social characteristics of a mountainous and rural commune are very similar, although geographic characteristics are different.
Households were selected for inclusion in the study based on a clustered sampling design in which the highest tier was the commune and the second tier was the hamlet from which households were randomly selected. Of 56 communes located in Da Nang, 3 urban (from a total of 37 urban communes), 2 rural (from 13) and 1 mixed urban–rural (from 6) communes were randomly selected, in which five hamlets were also randomly selected within each. From a census list of households in each hamlet, 30 households were randomly selected and adults, aged 35 years or older, living in these households were approached for inclusion in the study.
Research staff conducted door-to-door visits of each selected household, described the study, and invited the adult household members aged 35 years or older to participate. They were asked to go to the nearest Department of Health clinic for administration of in-person interviews and physical assessments. If no one was at home, multiple visits were made to the household and/or a letter was left there explaining the study. All households were ultimately contacted. Of the 5.5% of refusals, the major reason involved the person being too busy to make time for the study with a few declining owing to lack of comfort with the procedures (e.g. blood spot collection). The Human Subjects Division of the University of Washington and an equivalent division in the Da Nang Department of Health approved all procedures. All study participants provided informed consent.
2.2. Data collection
The WHO’s STEPS instrument was utilized from the WHO STEPwise Approach to Chronic Disease Risk Factor Surveillance as the basis for community interviews [14] in order to collect data via an in-person interview. All questions, including those on demographics, tobacco and alcohol use, physical activity, self-reported history of disease, and dietary intake were included. These questions were supplemented with others on physical function, women’s health and anxiety/stress. Questions were included from U.S.-validated instruments on symptoms that may be related to previous myocardial infarction or stroke. Questions on chest pain were from the Rose Angina Questionnaire [15]. Six questions on stroke symptoms were taken from the Questionnaire for Verifying Stroke-Free Status (QVSFS) [16]. In addition to asking if respondents had been told by a physician whether they had ever had a stroke, mini-stroke or transient ischemic attack, this questionnaire asks if they had ever had the following symptoms: (1) sudden painless weakness on one side of the body; (2) sudden numbness or a dead feeling on one side of the body; (3) sudden painless loss of vision in one or both eyes; (4) sudden loss of one-half of vision; (5) sudden loss of the ability to understand what people are saying; and (6) sudden loss of the ability to express ideas verbally or in writing. The questions in the QVSFS have been reported to have a negative predictive value (NPV) of 0.96 for the probability of correctly identifying stroke-free individuals, and a positive predictive value (PPV) of 0.71 for correctly identifying those with a history of stroke/transient ischemic attack in a population with a high prevalence of stroke [16]. Systolic and diastolic blood pressure (mm Hg) and heart rate (beats/minute) statistics were collected using a digital blood pressure device (Microlife USA, Inc., Clearwater, FL). Participants were allowed to sit quietly for 5 min prior to having their blood pressure taken twice in a seated position; the average of the two measures was used for analysis. Weight (±0.2 lb) was also measured (OMRON Model HBF-400 scale, Omron Corporation, Kyoto, Japan). Participants removed their shoes prior to being weighed.
Two health care workers stationed at each of the hamlet health clinics collected the data. A centralized training of all research staff was held to review study procedures, make final modifications, pre-test the forms, and conduct field exercises of examination procedures. Data were collected between July 1 and December 30, 2010. Four supervisors provided guidance on questions that arose during the data collection period across all sites. Study physicians conducted site visits periodically throughout the study period to monitor quality and assure standardization of procedures.
2.3. Statistical analysis
Body mass index was calculated and categorized as underweight (less than18), normal (18–25), overweight (25–30) and obese (greater than 30). Hypertension was designated as systolic blood pressure greater than 140 mm Hg or diastolic blood pressure greater than/equal to 90 mm Hg. After discovering a relatively high frequency of vision symptoms, potential issues that may have been related to a misinterpretation of these questions were discussed with medical colleagues in Da Nang. It became clear that these questions could have elicited a response based on any previous vision problem regardless of its etiology and not necessarily stroke-related. To increase the sensitivity of the questions for use in regression analysis, a binary, non-visual variable identifying self-report of at least one of the other four non-visual symptoms: weakness, numbness, problems with understanding language, and problems with speaking/writing was developed in an attempt to increase the sensitivity of the questions.
Descriptive statistics were calculated by gender. Multivariate logistic regression adjusted for household clusters was completed using the binary non-visual stroke variable as the dependent variable. Variables selected for potential inclusion in the model were age, gender, education (years), region, hypertension (self-reported and measured), self-reported diabetes, self-reported high cholesterol, severe chest pain lasting 30 min or longer, smoking status (never, former, current), number of drinks consumed in a week (categorized as none, 1–7 or greater than 7), number of days eating fruits/vegetables per week (categorized as less than 3, 3–4, 5–6, or 7 days/week), BMI category (underweight, normal or overweight/obese), and low activity level (defined from STEPS survey). Associations were reported in models adjusted for demographics (age, region, gender, education, and household) and in a fully-adjusted model with all variables included. Odds ratios (OR), 95% confidence interval (CI) and p-values were reported. Analyses were performed using SPSS version 16.0 and Stata version 11.0.
3. Results
Of the 1713 adults approached for inclusion in the study, 92 from 17 households declined participation resulting in a response rate of 94.5%. A total of 1621 adults from 883 households provided informed consent and completed the study. The age of participants ranged from 35 to 93 years with a mean of 52.0 years (±12.5) and 56.1% were women.
While men and women did not differ by age (Table 1), gender differences were found for geographic region, income, education, smoking status, measured hypertension and number of reported stroke symptoms (p < .01). More than half (51.1%) of men self-reported to be current smokers compared with only 6.7% of women. Almost 5% (78 participants) reported having severe chest pain lasting over 30 min indicative of a previous myocardial infarction. Four persons reported having been told they had suffered a heart attack. Four participants, two men and two women, reported having been told by a health care worker that they had had a stroke; three currently used tobacco (all men), only one had measured hypertension, and one was overweight. All were identified by the QVSFS reporting symptoms other than vision problems. Of the 443 persons found to have hypertension, more than two thirds (302) were unaware of their condition (Table 2).
| Characteristic | Men (N = 712) | Women (N = 909) | Total (N = 1621)a | pb | |||
|---|---|---|---|---|---|---|---|
| N | % | N* | % | N* | % | ||
| Age (years) | 0.20 | ||||||
| <40 | 125 | 17.6 | 124 | 13.7 | 249 | 15.4 | |
| 40–49 | 230 | 32.4 | 303 | 33.4 | 533 | 32.9 | |
| 50–59 | 192 | 27.0 | 278 | 30.6 | 470 | 29.0 | |
| 60–69 | 80 | 11.3 | 100 | 11.0 | 180 | 11.1 | |
| 70+ | 83 | 11.7 | 103 | 11.3 | 188 | 11.5 | |
| Mean ± SD | 51.8 ± 12.5 | 52.2 ± 12.4 | 52.0 ± 12.5 | 0.33 | |||
| Region | 0.004 | ||||||
| Urban | 389 | 54.6 | 449 | 49.4 | 838 | 51.7 | |
| Rural | 220 | 30.9 | 272 | 29.9 | 492 | 30.4 | |
| Mixed urban–rural | 103 | 14.5 | 188 | 20.7 | 291 | 18.0 | |
| Monthly household income (in millions of dong) | 0.001 | ||||||
| <2 | 113 | 16.1 | 212 | 23.8 | 325 | 20.4 | |
| 2–3.9 | 235 | 33.5 | 270 | 30.3 | 505 | 31.7 | |
| 4–5.9 | 148 | 21.1 | 198 | 22.2 | 346 | 21.7 | |
| >6 | 205 | 29.2 | 211 | 23.7 | 416 | 26.1 | |
| Education | <0.001 | ||||||
| No formal schooling | 8 | 1.1 | 76 | 8.4 | 84 | 5.2 | |
| Grade school | 544 | 76.4 | 716 | 78.8 | 1260 | 77.7 | |
| College | 48 | 6.7 | 63 | 6.9 | 111 | 6.8 | |
| University or post-grad | 112 | 15.7 | 54 | 5.9 | 166 | 10.2 | |
| Self-reported medical history | |||||||
| Hypertension | 101 | 14.2 | 131 | 14.4 | 232 | 14.3 | 0.52 |
| Diabetes | 26 | 3.7 | 37 | 4.1 | 63 | 3.9 | 0.72 |
| Myocardial infarction | 2 | 0.3 | 2 | 0.2 | 4 | 0.2 | 0.59 |
| Severe chest pain (⩾30 min) | 30 | 4.2 | 48 | 5.3 | 78 | 4.8 | 0.32 |
| Stroke | 2 | 0.3 | 2 | 0.2 | 4 | 0.2 | >0.99* |
| High cholesterol | 41 | 5.8 | 58 | 6.4 | 99 | 6.1 | 0.59 |
| Cancer | 2 | 0.3 | 4 | 0.4 | 6 | 0.4 | 0.70* |
| Self-reported number of stroke symptoms | 0.002 | ||||||
| 0 | 565 | 79.6 | 646 | 71.6 | 1211 | 75.1 | |
| 1 | 76 | 10.7 | 121 | 13.4 | 197 | 12.2 | |
| 2 | 49 | 6.9 | 88 | 9.8 | 137 | 8.5 | |
| 3+ | 20 | 2.8 | 47 | 5.2 | 67 | 4.2 | |
| Nutritional status | 0.61 | ||||||
| Underweight | 79 | 11.2 | 121 | 13.4 | 200 | 12.4 | |
| Normal | 513 | 72.6 | 637 | 70.6 | 1150 | 71.5 | |
| Overweight | 107 | 15.1 | 134 | 14.9 | 241 | 15.0 | |
| Obese | 8 | 1.1 | 10 | 1.1 | 18 | 1.1 | |
| Current smoking | 364 | 51.1 | 61 | 6.7 | 425 | 26.2 | <0.001 |
| Measured hypertension | 245 | 34.4 | 198 | 21.8 | 443 | 27.3 | <0.001 |
Numbers may not sum to total due to missing data.
p of 2-sided Fisher’s Exact test.
Characteristics of community survey participants in Da Nang, Viet Nam, by sex.
| Self-reported hypertension | Measured hypertension | ||||||
|---|---|---|---|---|---|---|---|
| No (N = 1177) | Yes (N = 443) | Total (N = 1620) | p | ||||
| n | % | n | % | n | % | ||
| Not reported | 1085 | 92.3 | 302 | 68.2 | 1387 | 85.7 | <0.001 |
| Yes, reported | 91 | 7.7 | 141 | 31.8 | 232 | 14.3 | |
Association between self-reported and measured hypertension.
Self-reported stroke symptoms differed by symptom and across gender (Fig. 1). Symptoms relating to vision problems were reported most frequently with over 22% of women and 15% of men reporting having experienced a sudden loss of vision in one or both eyes. Almost 13% of the women and 8% of the men previously experienced a sudden loss of half of their vision. The prevalence of other reported stroke symptoms was much lower. The number of symptoms reported increased with age (Fig. 2). While almost 84% of adults under 40 years of age had not experienced any of these symptoms, the number was reduced to 63% in those age 70 years and older. Using these symptoms, 75.3% of all subjects were considered to be “stroke-free”.
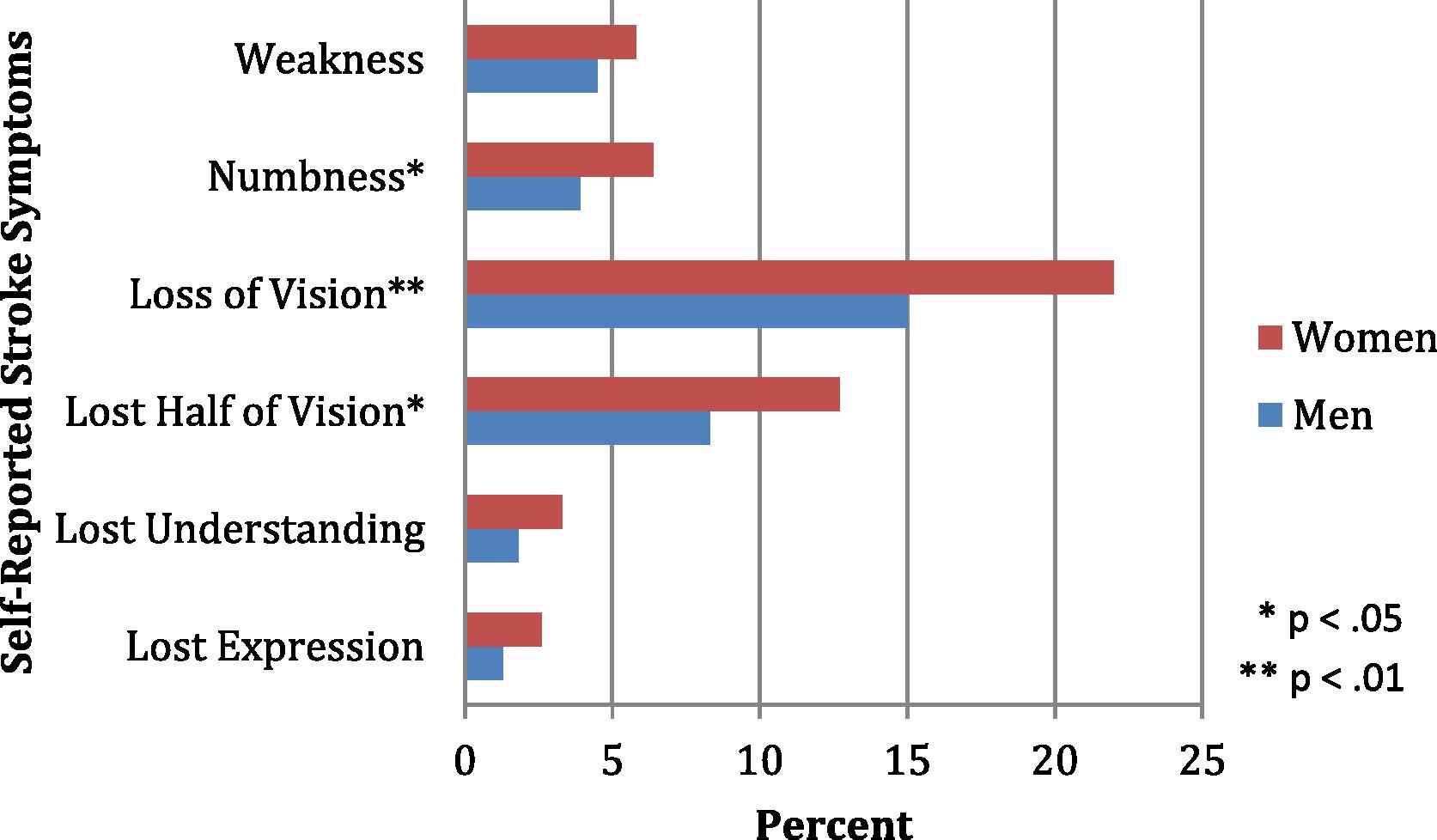
Self-reported stroke symptoms (%) by gender in 1621 adults age 35 and older living in Da Nang province, Viet Nam.
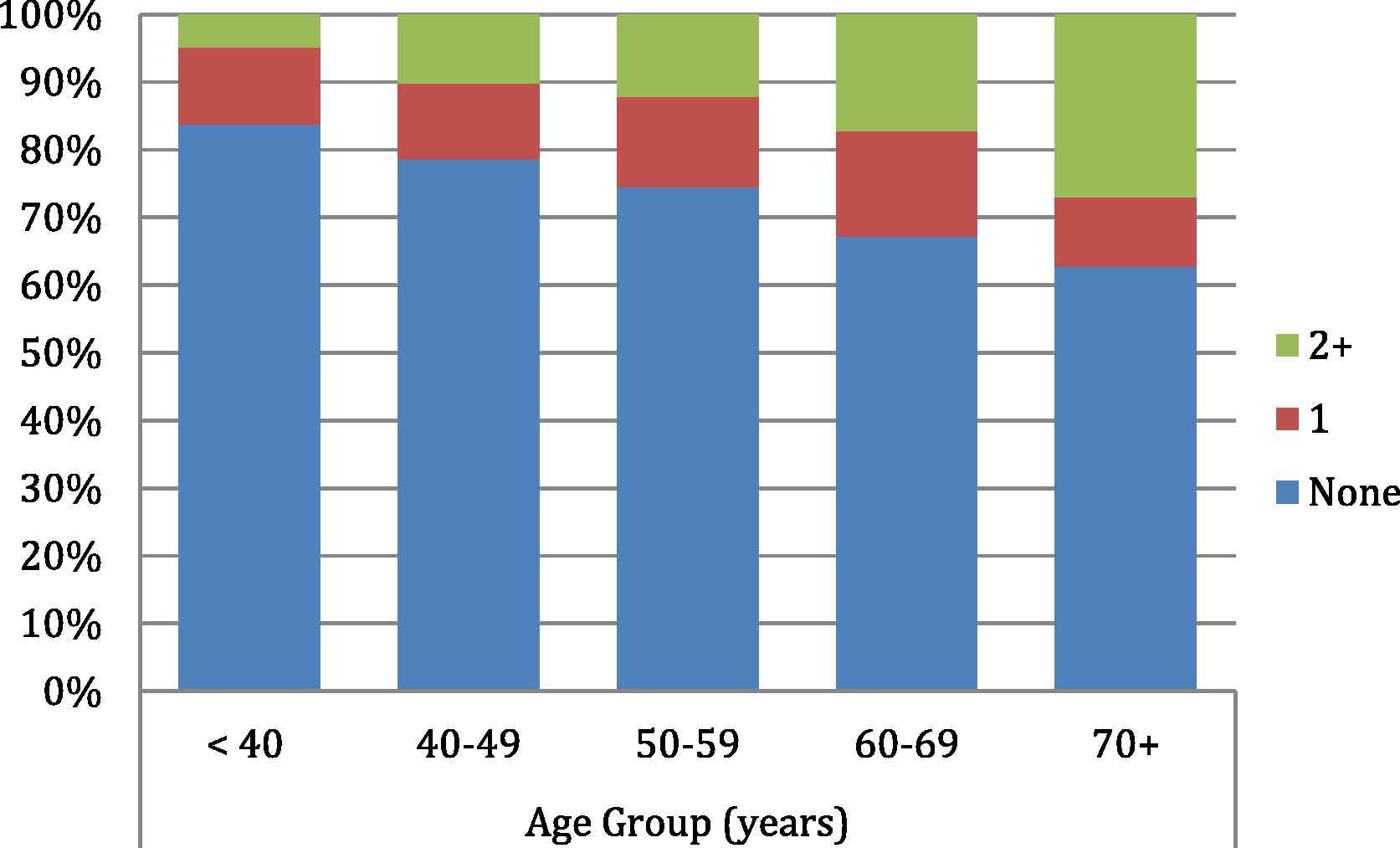
Number of stroke symptoms reported by age category in 1621 community-dwelling adults in Da Nang, Viet Nam.
As a result of the high potential for misinterpretation of the questions related to vision loss, factors for possible stroke excluding these two symptoms were investigated. The frequency of having any one of the other four symptoms was reduced to 9.4% (153 individuals). Results of the logistic regression models assessing risk factors for non-visual stroke symptoms are shown in Table 3. Models were adjusted for clustering within household, age, region and education. Five additional risk factors were associated with the non-visual stroke symptoms after adjustment for demographics: hypertension (self-reported, measured or both) (OR: 1.85, 95% CI: 1.29–2.66); self-reported high cholesterol (OR: 4.61, 95% CI: 2.66–7.97); reporting previous severe chest pain lasting 30 min or longer (OR: 6.46, 95% CI: 3.70–11.30); former smoking compared with non-smokers (OR: 2.00, 95% CI: 1.13–3.53); and being overweight compared with normal weight individuals (OR: 1.82, 95% CI: 1.11–2.95). In the fully adjusted model, age, region, hypertension, high cholesterol, severe chest pain, and former smoking remained associated with non-visual stroke symptoms.
| N | Demographic adj.a Odds Ratio (95% CI) | p | Full adjustmentb Odds Ratio (95% CI) | p | |
|---|---|---|---|---|---|
| Age (years) | 1618 | 1.04 (1.03–1.05) | <0.001 | 1.04 (1.02–1.05) | <0.001 |
| Region | |||||
| Urban | 838 | 1.00 (reference) | 1.00 (reference) | ||
| Rural | 492 | 1.64 (1.09–2.50) | 0.02 | 2.36 (1.41–3.97) | 0.001 |
| Mixed Urban/Rural | 291 | 2.30 (1.43–3.69) | 0.001 | 2.95 (1.72–5.07) | <0.001 |
| Male gender | 712 | 0.89 (0.61–1.32) | 0.567 | 0.76 (0.40–1.46) | 0.42 |
| Education (years) | 1621 | 0.95 (0.90–1.00) | 0.05 | 0.98 (0.93–1.04) | 0.53 |
| Diabetesc | 63 | 2.01 (0.93–4.32) | 0.08 | 0.96 (0.33–2.79) | 0.94 |
| High cholesterolc | 99 | 4.61 (2.66–7.97) | <0.001 | 3.21 (1.51–6.84) | 0.002 |
| Hypertensiond | 534 | 1.85 (1.29–2.66) | 0.001 | 1.63 (1.08–2.45) | 0.02 |
| Severe chest paine | 78 | 6.46 (3.70–11.30) | <0.001 | 5.62 (3.04–10.36) | <0.001 |
| Smoking status | |||||
| Never | 960 | 1.00 (reference) | 1.00 (reference) | ||
| Former | 235 | 2.00 (1.13–3.53) | 0.02 | 1.94 (1.04–3.61) | 0.04 |
| Current | 425 | 0.93 (0.52–1.67) | 0.82 | 1.07 (0.57–2.00) | 0.83 |
| BMI Category | |||||
| Normal | 1150 | 1.00 (reference) | 1.00 (reference) | ||
| Underweight | 200 | 1.16 (0.72–1.88) | 0.54 | 1.19 (0.73–1.95) | 0.38 |
| Overweight/Obese | 259 | 1.82 (1.11–2.95) | 0.02 | 1.38 (0.79–2.39) | 0.26 |
| Alcoholic drinks/week | |||||
| None | 987 | 1.00 (reference) | 1.00 (reference) | ||
| 1–7 drinks | 557 | 1.07 (0.65–1.77) | 0.77 | 0.99 (0.58–1.67) | 0.96 |
| 7 or more | 75 | 0.30 (0.07–1.35) | 0.12 | 0.27 (0.05–1.33) | 0.11 |
| Fruits/vegetables eaten | |||||
| 7 days per week | 402 | 1.00 (reference) | 1.00 (reference) | ||
| 5–6 days | 757 | 0.83 (0.49–1.43) | 0.51 | 0.80 (0.44–1.46) | 0.47 |
| 3–4 days | 346 | 1.21 (0.68–1.28) | 0.52 | 1.27 (0.66–2.44) | 0.27 |
| Less than 3 days | 115 | 1.29 (0.62–0.70) | 0.49 | 1.33 (0.56–3.17) | 0.52 |
| Low physical activity | 1.29 (0.87–1.91) | 0.20 | 1.26 (0.83–1.91) | 0.27 | |
Adjusted for age, gender, education, region and household (cluster). ORs for demographics are shown without additional variables in the model.
Adjusted for all variables shown.
Self-reported.
Self-reported or measured at examination above 140 mm Hg systolic or 90 mm Hg diastolic.
Previous self-reported severe chest pain lasting more than 30 min.
Risk of Stroke Symptoms by Selected Risk Factors using Multivariate Logistic Regression.
4. Discussion
This is the first study to evaluate symptoms and risk factors for stroke in a community setting in Viet Nam. Using symptoms, three fourths (75.3%) of adults aged 35 years and older were found to be “stroke-free” based on the QVSFS. In a regression model designed to identify the most potent predictors of these stroke symptoms, several expected risk factors were found to be associated, including age, geographic region, hypertension, and being overweight. However, two other chronic diseases emerged as risk factors for stroke symptoms: history of a previous myocardial infarction (as measured by symptoms) and self-reported high cholesterol.
Self-report of disease underestimates the prevalence of many conditions, including chronic diseases. In developing countries where access to health care is limited, less severe symptoms or those lasting for shorter durations may often never be brought to the attention of a physician. Only four participants reported that a doctor or health care worker had told them they had had a stroke in this sample. The prevalence of self-reported stroke found here—2.5 per 1000—is slightly lower than those reported in two other Viet Nam regions—between 6–10 per 1000 in two rural areas [17], and 6.1 per 1,000 in both urban and rural sites in the south [18].
Use of symptoms to identify persons at high risk of stroke has been previously utilized in developed countries [12,19]. In the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, persons identified through the QVSFS were found to have decreased physical and mental functioning [12] including cognition [20], and to be at an elevated risk of future stroke [21] suggesting these symptoms may be a form of “whispering” stroke. This premise may be even more relevant in countries with fewer opportunities for diagnosis than in the U.S. In Mexico, stroke symptoms lasting longer than 24 h were reported in only 30 of 2437 (1.2%) persons surveyed, much lower than symptoms reported here [22]. As the symptoms reported in this study and in REGARDS do not specify duration, they are capable of capturing TIAs which also are highly predictive of future stroke. However, this definition may also increase the capture of other non-stroke/TIA conditions as symptoms in less than 24 h which can reflect a variety of etiologies.
The high prevalence of the visual symptoms collected in this study in Viet Nam suggests that they are less reliably predicting cerebrovascular accidents (CVAs) and may represent other illnesses such as migraine, a unique cultural interpretation of the questions, or both. In addition, other non-neurologic causes of visual problems are also likely to be picked up here, such as those owing to infections, cataracts, and other conditions. While this definition of stroke, excluding visual symptoms, does not replace a neurologic exam, it may afford a useful measure for both stroke screening and for research purposes. This study did not estimate stroke prevalence in Da Nang using responses to the QVSFS as the setting and context here were very different than in other studies validating the use of the questionnaire [16,23]. However, it remains a useful tool for estimating “stroke-free” status as has been reported in this study.
In Viet Nam, chronic disease risk factors are alarming. Similar to the findings in this study that over half the men were current smokers, another study reported that nearly a quarter of adults and half of the men aged 15 years and older currently smoke tobacco [6]. The 2001–2002 Viet Nam National Health Survey found 17% of adults aged 25–65 years old were hypertensive, which represents a 51% increase since 1992 [24]. Studies have reported the prevalence of hypertension among adults reaching 30% in urban areas [7,25] and 20% in rural ones [8,9]. Of emerging importance in countries experiencing the health transition is the increase in body mass index (BMI) leading to obesity in populations previously dealing with malnutrition [26].
Culturally, both alcohol and tobacco use is highly prevalent in Viet Nam. Although bong use is found in the north or more mountainous regions of the country, cigarettes are the predominant type of smoking in Da Nang. In the questionnaire, participants were asked about the frequency of different types of tobacco used. Of the 425 current smokers in this study, all smoked either manufactured or hand-rolled cigarettes and none used pipes, cigars, or cheroots. Unfortunately, there was no question regarding the use of bongs although they are rare in Da Nang. Only 5% used smokeless “tobacco”, with almost all respondents chewing the “betel” leaf, a mild stimulant. Alcohol consumption behavior can include social drinking around meals as well as binge drinking during events and rites, such as weddings. The source of the alcohol consumed was not clarified in the questionnaire utilized in this study and therefore could not determine differences in risk between Western drinks, home brews, or other liquors consumed.
Many of the risk factors found to be associated with non-visual stroke symptoms were to be expected, especially associations with increased age, rural region, less education, prevalence of hypertension and obesity. The more than six-fold increased association of stroke symptoms in persons who reported severe chest pain and the four-fold increased association in those reporting hyperlipidemia may reflect the duality of heart disease and stroke reflecting cardiovascular diseases as well as confusion between heart and brain diseases in Viet Nam. In general, the results of this study correspond well with those found in the INTERSTROKE Study, a case-control study evaluating risk factors for stroke in 22 countries [27], although several risk factors in this study did not reach significance, most likely owing to study power.
Strengths of this study include the random selection of adults living within a community setting, the standardized use of study instruments across regions, the near complete participation, and the evaluation of stroke symptoms using a standardized questionnaire. The primary weakness of this study involved its inability to follow-up participants with a clinical evaluation. Follow-up of those individuals reporting symptoms with neurologic evaluations at a future surveillance visit may help shed light on distinctions between prior stroke, TIA and non-CVA symptoms. Other limitations include the inability to distinguish sources of alcohol or food consumption which may result in different associations with stroke symptoms and the lack of clarity in ascertaining vision-related stroke symptoms. Regardless, this study provides important data to be considered when evaluating persons at a high risk of future stroke in Viet Nam.
5. Conclusions
The results of this study confirm the serious burden of stroke symptoms and risk factors in Viet Nam. Prospective studies are needed to verify these results and to provide data to monitor trends in stroke and chronic disease risk factors. Ultimately, development of interventions to reduce hypertension and other risk factors for stroke is of critical importance in Viet Nam and other low-resource countries facing the health transition.
Acknowledgment
This study was funded by 1 R21 TW008431-01A1 of the Fogarty International Center and the National Institute of Neurological Disorders and Stroke, National Institutes of Health.
Disclosures: No co-authors have any disclosures to make regarding conflicts of interest. All co-authors have read and approved this manuscript for submission to this journal.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jegh.2012.06.001.
References
Cite this article
TY - JOUR AU - Annette L. Fitzpatrick AU - Quang Van Ngo AU - Kiet A. Ly AU - Thanh G.N. Ton AU - WT Longstreth AU - Tung T. Vo AU - Kristen Heitzinger AU - Chien H. Pham AU - David L. Tirschwell PY - 2012 DA - 2012/08/13 TI - Symptoms and risk factors for stroke in a community-based observational sample in Viet Nam JO - Journal of Epidemiology and Global Health SP - 155 EP - 163 VL - 2 IS - 3 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2012.06.001 DO - 10.1016/j.jegh.2012.06.001 ID - Fitzpatrick2012 ER -
