Assessing the silent epidemic of malnutrition in Palestinian preschool children
- DOI
- 10.1016/j.jegh.2012.12.002How to use a DOI?
- Keywords
- Iron deficiency anemia; Wasting; Stunting; Underweight; Malnutrition
- Abstract
Background: The nutritional status of children living under conflict is an important issue. The aim of the present study is to review all available data on malnutrition in preschool Palestinian children and provide objective results concerning the epidemic of malnutrition.
Methods: The literature for all research on the prevalence of malnutrition on Palestinian children with data collected during the period 1998–2007 was reviewed. Der Simonian-Laird Random effects model for meta-analysis was applied and cumulative analyses were performed to determine time-trends for each outcome measure (iron deficiency anemia [IDA], wasting, underweight and stunting).
Findings: The results showed that 39.5% of the children suffered from IDA, 2.9% from wasting, 4.7% were underweight and 10.9% stunted. The cumulative analyses showed a peak in the prevalence of IDA during 1999, followed by an irregular decrease afterward. The proportion of wasted and underweight children peaked during 2002 and 2004, respectively, both showing a gradual decline afterward. Chronic malnutrition appears to be almost similar during the decade 1998–2007, by demonstrating small, irregular oscillations.
Conclusions: Although the prevalence of malnutrition among Palestinian preschool children has been improved during the studied period, it still remains high. Additionally, the results show that interventions/aid have acute effects on the health of children.
Funding: None.
- Copyright
- © 2012 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/)
1. Introduction
According to the Declaration of the Rights of a Child [1], “a child shall enjoy protection … to develop physically in a normal manner.” Half a century after this declaration and despite multiple public urges for international intervention [2,3], this statement still fails to apply to the Palestinian children. Two uprisings (Intifadas), a military occupation, poverty, parental unemployment, limited food availability, food insecurity, sieges and curfews have all contributed to the deterioration of the health of the Palestinian people, and especially the more vulnerable children [4,5]. Everything points to the fact that the conflict has a direct effect on the health of Palestinian children, making them more vulnerable to undernutrition.
Among the plethora of mental and physical health problems recorded in the Palestinian youth, anemia and malnutrition during preschool ages appear to be the most predisposing factors [6–10]. According to the United Nations Children’s Fund (UNICEF), malnutrition constitutes the new global silent emergency [11,12], merely invisible in the developed countries where obesity – the exact opposite phenomenon – has become an epidemic. The risk of increasing undernutrition and dying from malnutrition in the absence of a long-term nutrition strategy plan is now evident [13]. Despite the importance of the topic, research on childhood malnutrition in Palestine appears to be scattered and heterogeneous. Several studies have been published using samples with non-comparable age-ranges, many of which provide either little or no information at all regarding population recruitment, response rates or even sample sizes. According to the Community and Public Health Masters’ students at Birzeit University [14], high-quality, unbiased and reliable data are needed in order to challenge policy makers. Thus, there is a need for quality assessment of studies assessing malnutrition in order to attain an objective and more accurate picture of the prevalence of childhood malnutrition in Palestine.
The aim of the present study is to review all available data on malnutrition in preschool Palestinian children and provide objective results concerning the epidemic of malnutrition in Palestine.
2. Methods
2.1. Search strategy and selection criteria
Ovid MEDLINE, EMBASE, Google Scholar, Google and Scopus were searched for studies published prior to December 2010 using the meSH terms “children”, “child”, “childhood”, “AND malnutrition OR underweight OR anemia OR anaemia OR stunting OR stunted OR wasted OR undernourished OR nutrition OR anthropometry OR weight OR height OR stature,” “AND Palestine OR Palestinian.” In addition, the references of the retrieved articles were also searched.
2.2. Definition of malnutrition, underweight and iron deficiency anemia
The World Health Organization (WHO) recommends that a z-score cut-off point of −2 is necessary for the diagnosis of global malnutrition (severe and moderate) [15]. Therefore, acute malnutrition (wasting) was defined as weight-to-height z-score ⩽−2 and chronic malnutrition (stunting) was defined as height-for-age z-score ⩽−2. Underweight was defined as weight-for-age z-score ⩽−2. According to the WHO, iron deficiency anemia (IDA) is diagnosed in children with hemoglobin levels below 11 gm/dl [16].
2.3. Inclusion and exclusion criteria
Criteria for inclusion were: (1) research on a Palestinian population; (2) age of participants between 3 and 59 months; (3) classification of wasting (WS), stunting (ST), underweight (UW) and IDA, according to the WHO criteria [15,16]; (4) collection of the sample between 1998 and 2007; and (5) reporting the total sample size (n).
Criteria for exclusion were: (1) reported mean/median z-score values instead of malnutrition categories; (2) diagnosis of malnutrition with different criteria than the WHO; (3) presentation of the prevalence of each malnutrition category without reporting sample size; (4) participation of children aged above 59 months in the reported prevalence; (5) overlapping studies; (6) studies with clinical samples; (7) studies on non-healthy participants; (8) samples with Israeli and Palestinian children grouped together; and (9) samples collected before the year 1998.
2.4. Study quality and sensitivity analyses
Studies of good quality were identified as those: (1) using total samples with at least 300 participants; (2) reporting year of data collection; (3) having weight and height measured by researchers instead of reported by the participants’ families; and (4) reporting a response rate (RR) greater than 70.0%. Studies that did not fulfill the quality assessment criteria were excluded from the sensitivity analyses.
After removal of the studies of lower quality, sensitivity analysis was performed in order to evaluate if the result was statistically significant compared with the pooled result of all retrieved studies. Publication bias was evaluated by using funnel plots. Heterogeneity was determined by I2.
2.5. Statistical analyses
Analyses were performed with Comprehensive Meta Analysis software V2.0 (Biostat Inc., Englewood, NJ, USA). Effect size was pooled from all eligible studies using the Der Simonian-Laird Random effects model (REM) for meta-analysis. Significance was measured at p ⩽ 0.05. Differences in the prevalence of malnutrition and IDA between sensitivity and pooled analyses were assessed with tests for two proportions (MiniTab® version 14.1 Minitab Inc., State College, PA, USA).
Time-trend of each outcome measure was evaluated through cumulative meta-analyses. To avoid systematic bias, studies were entered into the model of each cumulative meta-analysis successively in the order of their chronological data collection time and not in the order of their publication time. Publications not reporting the year of data collection were not included in the cumulative analyses.
3. Results
3.1. Selection of studies
The search retrieved 54 studies, but only 17 of those fulfilled the inclusion criteria. The flow chart for the selection process of the retrieved studies is shown in Fig. 1, and the studies that fulfilled the inclusion criteria are presented in Table 1. Due to the file drawer problem [17], the majority of the retrieved studies involved the collection of data between the years 1998 and 2008, with the latest one having been presented in a conference only. One study did not report the year of data collection [26]. The majority of the studies used samples from the West Bank and the Gaza Strip and four used national representative samples [21,29–31].
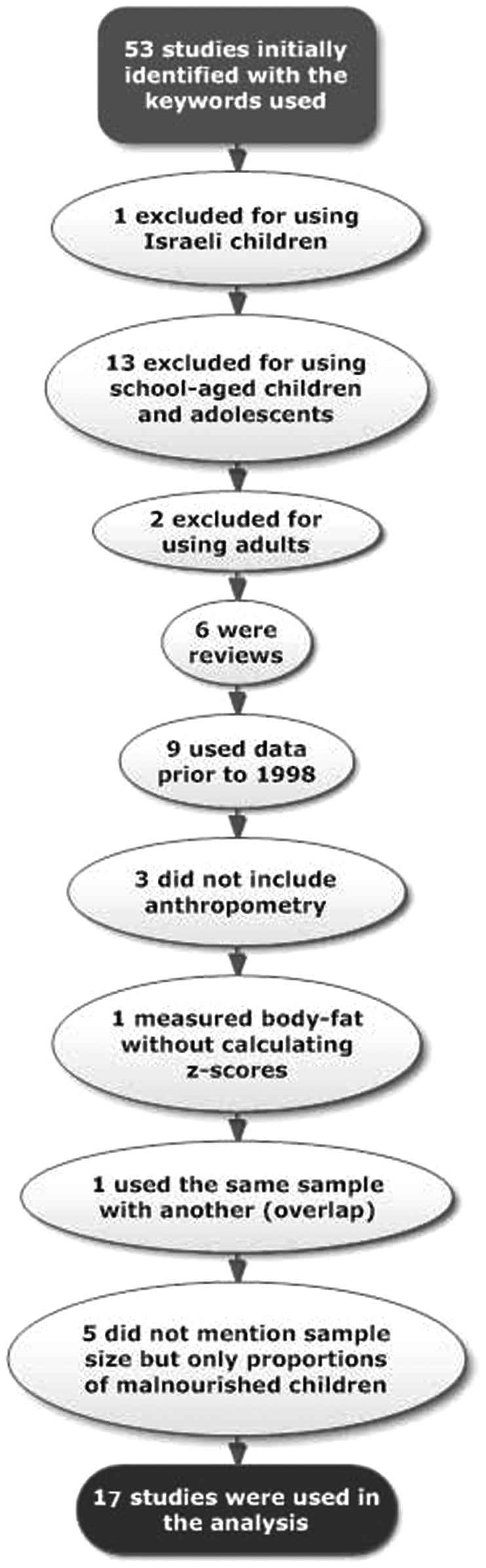
Flow chart of the retrieved and excluded studies of the systematic review.
| Recruitment district | Data collection (year) | Age of participants (months) | Study’s Total sample (n) | Design | Funding | RR (%) | Growth charts/software used | Preschool sample tested for malnutrition (n) | WS (%) | UW (%) | ST (%) | Preschool sample tested for IDA (n) | IDA (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gaza Strip refugees [18] | 1998 | 6.0–35.9 | 1 830c | CSSe | UNRWA, CDC | 98.8 | NCHS/CDC/WHO, EpiInfo™6.01 | 398 | 1.4 | – | 13.0 | 363 | 52.8 |
| West Bank and Gaza Strip Refugees [19] | 1999 | 6.0–36.0 | 8 297 | CSS | – | NR | None needed | – | – | – | – | 3832 | 64.5 |
| National Survey [29] | 2000 | 6.0–59.0 | 11,898c | CSSS | PCBS UNICEF, UNFPA | 99.8 | NCHS/CDC/WHO | 6169 | 1.4 | 2.5 | 7.5 | – | – |
| West Bank and Gaza Strip [20] | 2002 | 6.0–59.0 | 936 | CSSe | USAID | 100.0 | EPINUT, EpiInfo™ | 936 | 7.8 | – | 11.7 | 936 | 43.9 |
| National Survey [21] | 2002 | 6.0–59.0 | NR | CSSe | UNICEF | 95.7 | NCHS/CDC/WHO | 3331 | 2.5 | 3.5 | 9.0 | 3257 | 37.9 |
| West Bank and Gaza [25] | 2002 | 12.0–59.0 | 1127 | CSSe | USAID, PMoH | 98.1 | None needed | – | – | – | – | 1106 | 23.0 |
| West Bank and Gaza Strip [7,22] | 2003 | 6.0–59.0 | 3089 | CSSe | USAID | 99.1 | Anthro 1.02, EpiInfo™6.0 | 3089 | 3.4 | 5.1 | 10.7 | – | – |
| East Jerusalem [23] | 2003 | 9.0–18.0 | 300 | CSSe | – | 100.0 | NCHS/CDC/WHO | 300 | 14.2 | 9.6 | 8.5 | 300 | 41.4 |
| Gaza City [8] | 2003 | 3.0–24.0 | 102 | CSS | – | 100.0 | EpiInfo™ | 102 | 30.4 | 30.4 | 34.4 | 81 | 72.8 |
| Gaza Strip [24] | 2003 | 6.0–59.0 | 1261 | CSS | ECHO | 99.2 | EpiInfo™ 5.0, EPINUT | 1251 | 1.7 | 5.6 | 8.5 | 1251 | 4.7b |
| West Bank and Gaza Strip [26] | NR | 6.0–59.0 | 3331 | CSS | PCBS, UNICEF, PMoH | 95.7 | EpiInfo 2000 | 3331 | – | – | 9.0 | 3331 | 37.9b |
| West Bank motherless orphans [27] | 2004 | 30.0–59.0 | 167d | Lx2 | – | 90.2 | EPINUT, EpiInfo™ | 34 | 8.8 | – | 17.6 | – | – |
| Yatta, Sumu, Dhaharieh and Ramadin [6] | 2004 | 6.0–59.0 | 266a | Lx2 | ECHO | 70.2 | Anthro 1.02 | 266 | 6.0 | 10.9 | 17.7 | 266 | 30.1 |
| National Survey [30] | 2004 | 6.0–59.0 | 9811c | CSSe | CFG, PNA | 96.1 | NCHS/WHO | 4835 | 2.8 | 4.9 | 9.9 | – | – |
| Gaza, Khanyounis and North Gaza [28] | 2005 | 6.0–59.0 | 754 | CSSe | UNICEF | 100.0 | Anthro 2005 | 754 | 2.4 | 2.5 | 10.4 | – | – |
| National Survey [31] | 2006 | 6.0–59.0 | 29,003c | CSSe | PNA, UNICEF, UNFPA, PAFHPP | 99.2 | NCHS/WHO | 4580 | 1.4 | 2.9 | 10.2 | – | – |
| Gaza Strip [32] | 2007 | 6.0–59.0 | 350 | CSSe | UniWin | 100.0 | Anthro 2005 | 350 | – | – | 15.0 | – | – |
RR: response rate; WS: wasting; UW: underweight; ST: stunting; IDA: iron deficiency anemia; NR: not reported; CSS: cross sectional; Lx2: longitudinal at 2 time points; PCBS: Palestinian Central Bureau of Statistics; UNICEF: United Nations Children’s Fund; PMoH: Palestinian Ministry of Health; CFG: Core Funding Group; PNA: Palestinian National Authority; PAFHPP: Pan Arab Family Health Project Partners; ECHO: European Commission Humanitarian Office; USAID: US Agency for International Development; UNRWA: United Nations Relief and Works Agency; CDC: Centers for Disease Control and Prevention; UniWin: University of Wisconsin; UNFPA: United Nations Population Fund.
Study also included children receiving iron supplementation.
IDA data were reported by mothers and not measured.
Sample also included children, adolescents, adults and elderly.
Sample also included older children.
Study included in the sensitivity analysis.
Results of the selected studies assessing the prevalence of malnutrition, underweight and IDA in Palestinian preschool children (1998–2007).
Eleven studies passed the quality assessment and were used in the sensitivity analyses. Due to the increased heterogeneity, random analyses were performed in all studied variables [(Pooled analyses: IDA fixed model I2 = 98.96%, Q = 521.6, p ⩽ 0.001; Wasting fixed model I2 = 92.96%, Q = 108.9, p ⩽ 0.001; Underweight fixed model I2 = 92.94%, Q = 127.5, p ⩽ 0.001; Stunting fixed model I2 = 85.37%, Q = 88.9, p ⩽ 0.001) and (Sensitivity analyses: IDA fixed model I2 = 96.63%, Q = 118.7, p ⩽ 0.001; Wasting fixed model I2 = 93.15%, Q = 116.7, p ⩽ 0.001; Underweight fixed model I2 = 92.35%, Q = 78.4, p ⩽ 0.001; Stunting fixed model I2 = 85.29%, Q = 61.2, p ⩽ 0.001)].
3.2. Prevalence of IDA, wasting, underweight and stunting
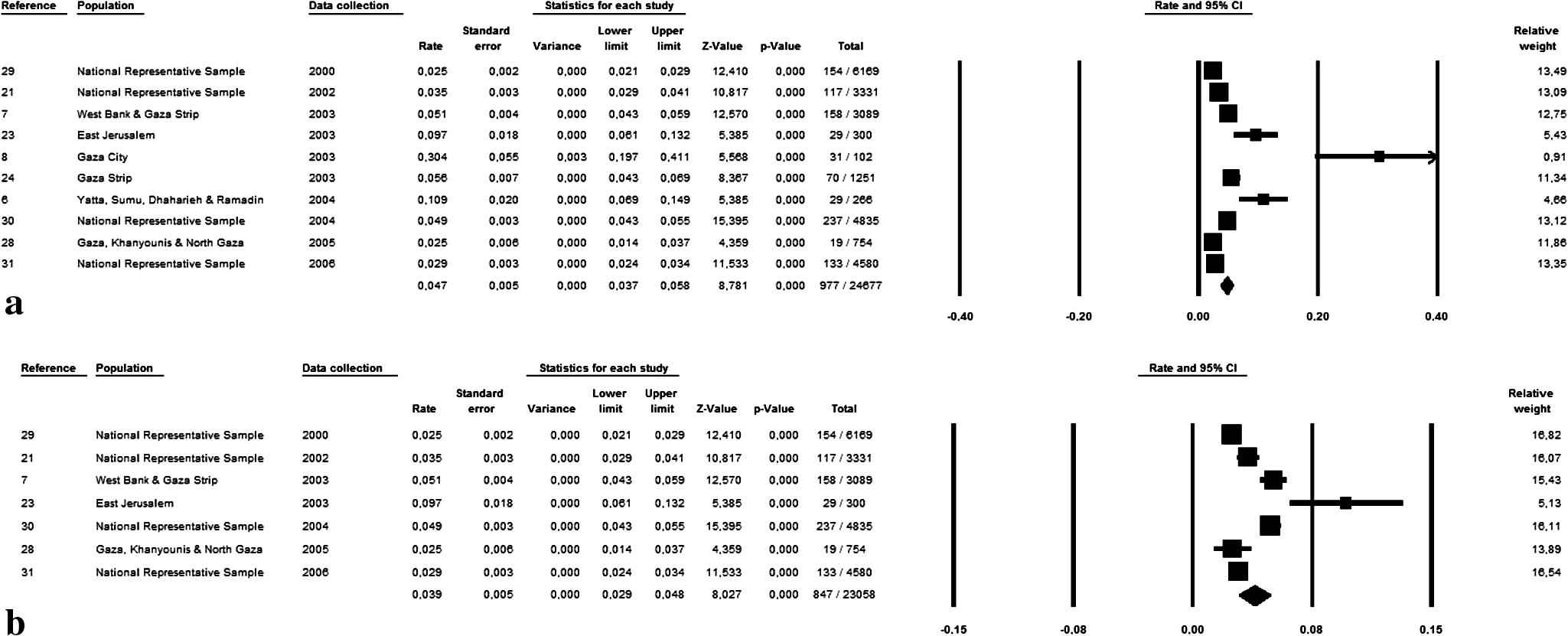
According to the pooled analysis, 44.0% of the Palestinian preschool children suffer from IDA, but the sensitivity analysis revealed a lower prevalence of 39.5% (total n = 5962) (p ⩽ 0.001) (Fig. 2). Wasting was apparent in 4.0% of the pooled sample and 2.9% of the sample used in the sensitivity analysis (total n = 24,392) (p ⩽ 0.001) (Fig. 3). A similar proportion of Palestinian preschool children was underweight according to the pooled and quality analysis (4.7%, total n = 24,677) (Fig. 4). Stunting was apparent in 10.9% of the sample (n = 26,395) (Fig. 5). The collective results and confidence intervals of the pooled and sensitivity analyses are presented in Table 2.
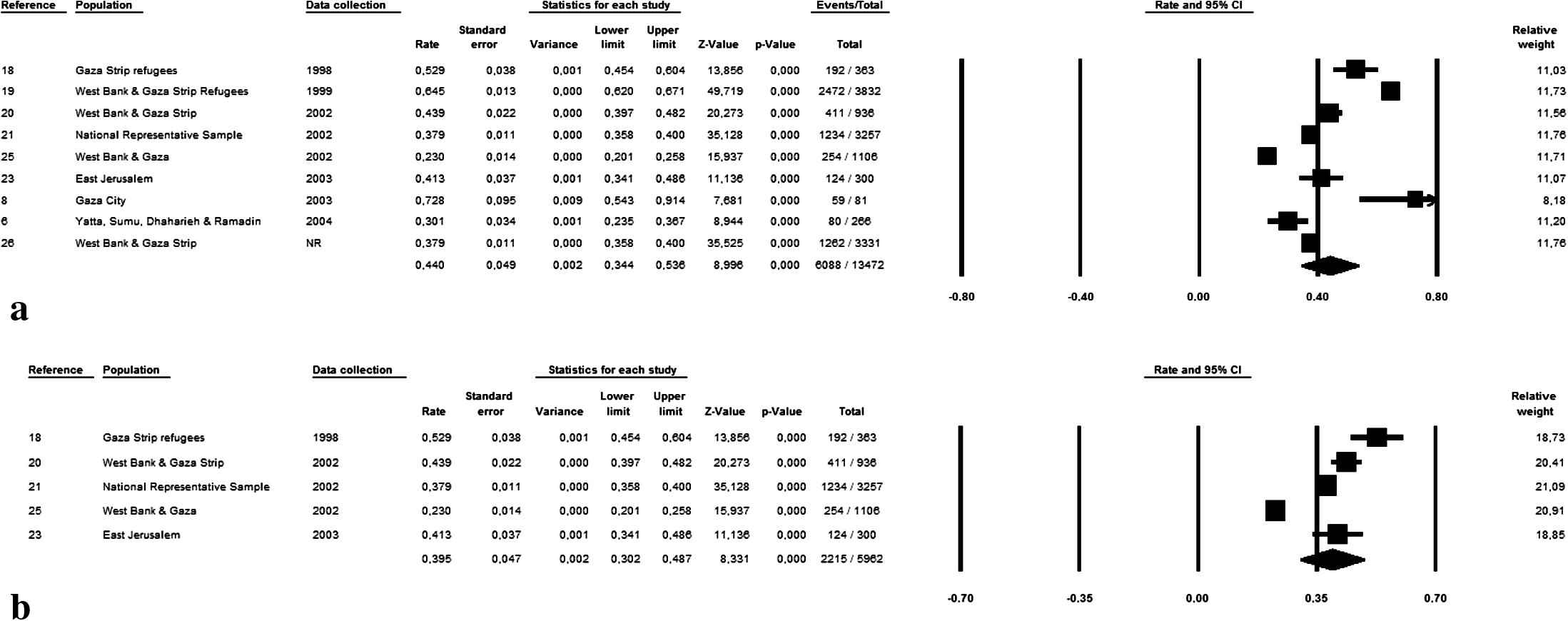
Pooled (a) and sensitivity (b) analysis of the prevalence of IDA in Palestinian preschool children (1998–2007).
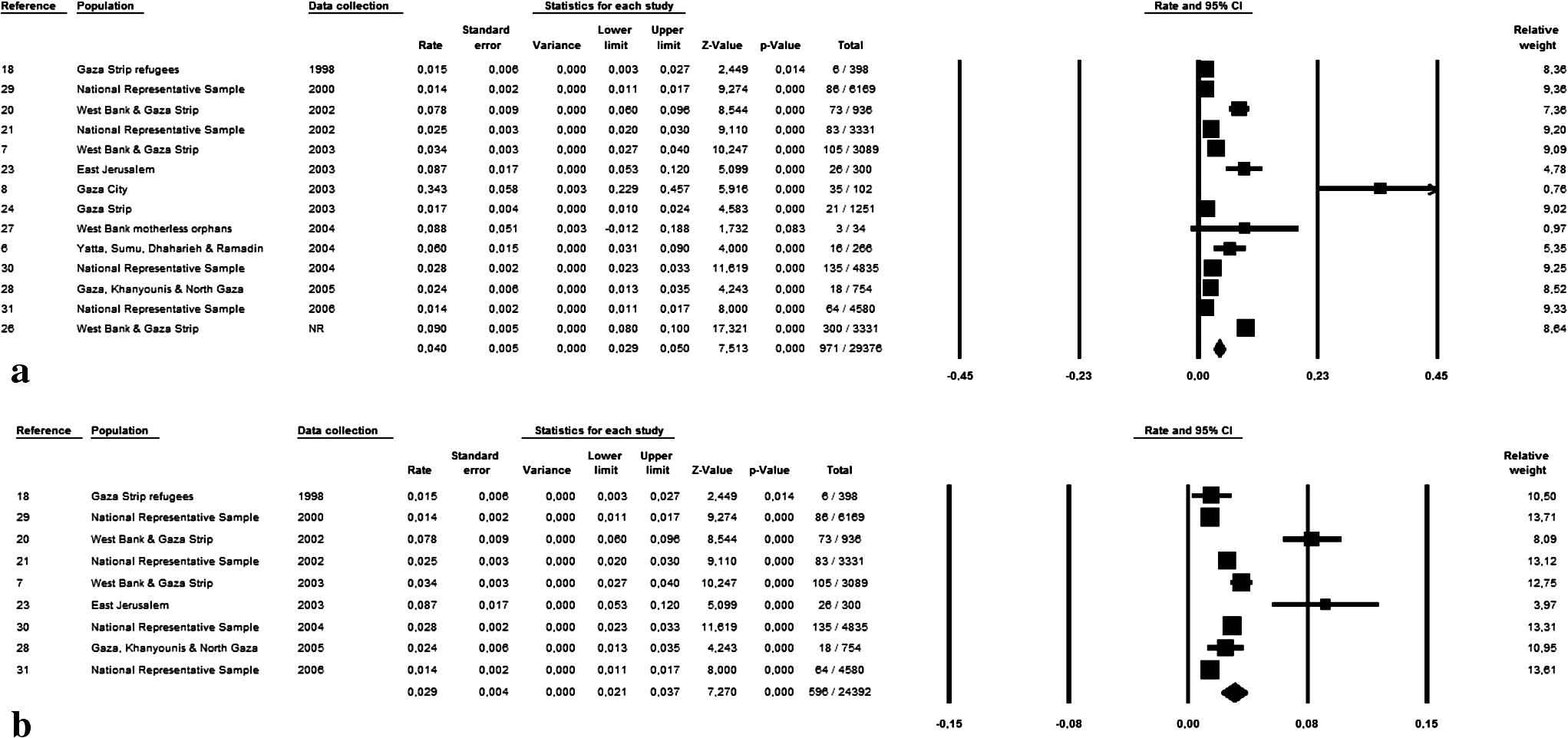
Pooled (a) and sensitivity (b) analysis of the prevalence of wasting in Palestinian preschool children (1998–2007).
Pooled (a) and sensitivity (b) analysis of the prevalence of underweight in Palestinian preschool children (1998–2007).
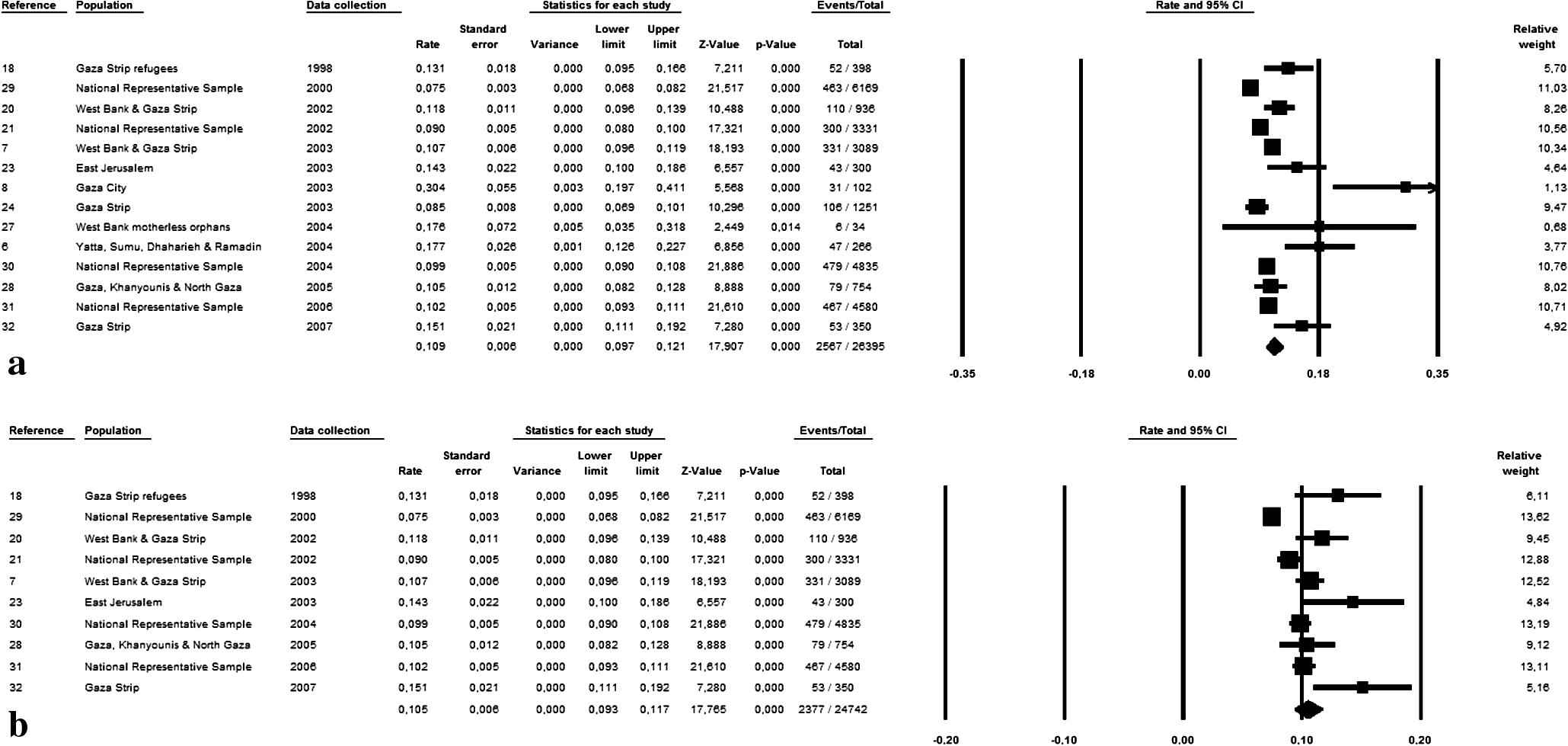
Pooled (a) and sensitivity (b) analysis of the prevalence of stunting in Palestinian preschool children (1998–2007).
| Analyses | Weight status | % | n/total | CI (95%) | I2 (%) | Q |
|---|---|---|---|---|---|---|
| Pooled | IDA | 44.0* | 6088/13,472 | 34.4–53.8 | 98.96 | 521.6 |
| Wasting | 4.0* | 971/29,376 | 2.9–5.0 | 92.96 | 108.9 | |
| Underweight | 4.7 | 977/24,677 | 3.7–5.8 | 92.94 | 127.5 | |
| Stunting | 10.9 | 2567/26,395 | 9.7–12.1 | 85.37 | 88.9 | |
| Sensitivity | IDA | 39.5 | 2215/5962 | 30.2–48.7 | 96.63 | 118.7 |
| Wasting | 2.9 | 596/24,392 | 2.1–3.7 | 93.15 | 116.7 | |
| Underweight | 3.9 | 847/23,058 | 2.9–4.8 | 92.35 | 78.4 | |
| Stunting | 10.5 | 2377/24,742 | 9.3–11.7 | 85.29 | 61.2 |
IDA: iron deficiency anemia.
Significantly different compared with the sensitivity analysis (p ⩽ 0.001).
Collective results of the pooled and sensitivity analyses of studies assessing the prevalence of malnutrition, underweight and IDA in Palestinian preschool children (1998–2007).
3.3. Trends in IDA, wasting, underweight and stunting during the years 1998–2007
According to the cumulative analysis (Fig. 6), the prevalence of IDA peaked during 1999 and has been following an irregular decrease afterward. The proportion of wasted children peaked during the year 2002 and the proportion of underweight during 2004, and both have been following a gradual decline after peaking. The prevalence of chronic malnutrition appears peaked during 1998 and remained almost similar during the years 2000–2007, although demonstrating small, irregular oscillations.
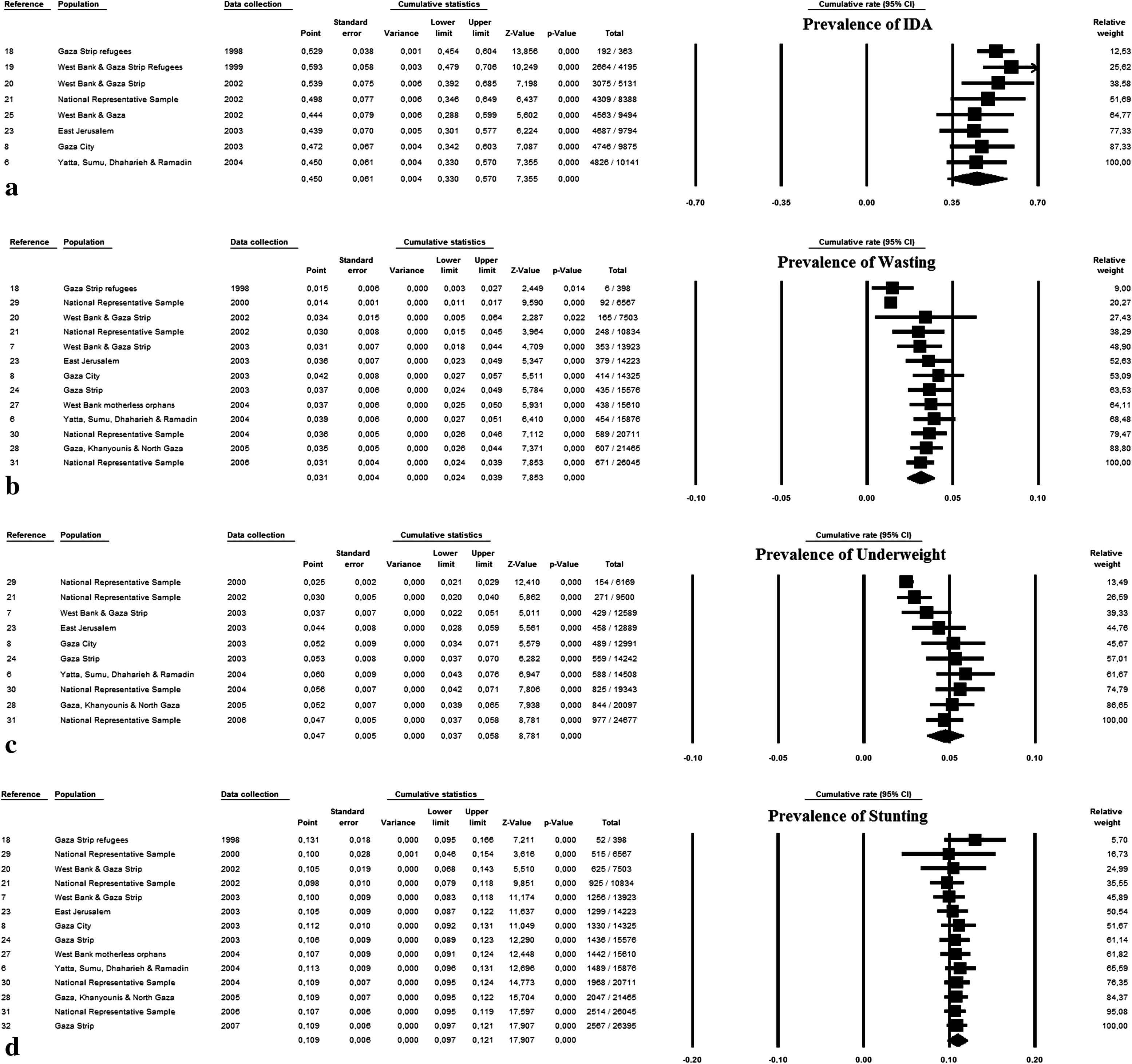
Cumulative analyses of the prevalence of IDA (a), wasting (b), underweight (c) and stunting (d) in Palestinian preschool children (1998–2007).
4. Discussion
The present findings demonstrate a slight decline in the prevalence of malnutrition and IDA in Palestinian preschool children over the last years; however, the numbers are still high. Approximately 39.5% of the children suffer from IDA, 10.9% from global chronic malnutrition, 2.9% from global acute malnutrition and 4.7% are considered underweight. The prevalence of IDA peaked during the year 1999 and has been following a small irregular decrease afterward. The proportion of wasted and underweight children peaked during the years 2002 and 2004, respectively and demonstrated a gradual decrease since then. Chronic malnutrition appears to be almost similar during the decade 1998–2007, just exceeding 10% of the under-five population.
According to Salah [23], several factors appear to affect wasting within a family. For example, firstborn children are less likely to experience competition for food resources and suffer from acute malnutrition, compared with their younger siblings since younger children are more dependent on others for their food intake. In addition, the greater the number of living children in a family, the more likely the children will be wasted [23], as the number of family members is directly associated with the amount of money needed for feeding. Additionally, maternal undernutrition also has effects on children’s nutritional status as undernourished mothers tend to raise undernourished children and experience miscarriages, stillbirths and under-5 mortality more often than not [33]. In Palestine, a great majority of the population is unemployed [34], one third of the population is food insecure [4], more than half of the families receive food donations [32] and are dependent on social aid [24], and more than 60.0% borrow money in order to buy food or other essentials [24]. According to Kanoa [35], the majority of families have reported being unable to provide adequate nutrition for their family members due to poverty and siege. In the Acción Contra el Hambre study implemented during 2003, participants reported a reduction in the consumption of basic food products, mainly meat, fruits and fish, with the latter being consumed once per month on average [24]. In parallel, foods rich in vegetable protein like legumes are being consumed by the majority of preschoolers, 1–3 times per week [35]. All studies stress the inadequacy in energy and protein intake, nutrients essential for growth and development [7,35]. Additionally, the main cause for IDA appears to be the low iron intake, the low bioavailability and the high intake of inhibitors of iron absorption (unleavened bread and tea) [36,37].
The Palestinian population is very young, with nearly half (46.3%) of the total population being under the age of 15 years [38]. This fact adds importance to the present findings as a great proportion of the Palestinian population appears to be malnourished, a state contributing to an increased morbidity and mortality. According to the WHO, more than 50.0% of children’s deaths are directly or indirectly caused by malnutrition. When a child is malnourished during the first two years of life, the child’s physical and mental growth and development are slowed irreversibly [13]. Recent studies on Palestinian adolescents demonstrate a high prevalence of stunting, wasting, underweight and IDA, indicating that when not treated, malnutrition spans a continuum from early childhood to adolescence [39,40].
Throughout the literature malnutrition appears to be a concern in the majority of the neighboring countries of Palestine, spanning from 2.0% among Jordanian children (for underweight and wasted) to 28.0% in Syria and 29.0% in Egypt (for stunted) to other countries in conflict [41]. The state of the World’s Children published annually by UNICEF [41] reported an increase in life expectancy at birth in the occupied Palestinian territory during the last 20 years whereas under-5 mortality has decreased. This has been the result of improved sanitation facilities, antenatal care, delivery care coverage, childhood immunizations, and increment in exclusive breastfeeding [9,10,41]. However, the prevalence of underweight or stunting in the area was not included in the UNICEF report [41], and factors affecting malnutrition, such as birth frequency [9,10], short birth spacing [9,10], rising poverty [10,41,42], unemployment [33], food insecurity [4,43], reduced food quantity and quality [10,24,34,43] or the prevalence of orphaned children have either experienced only slight improvements or have not been measured.
Rahim et al. [10] used data from the Palestinian Central Bureau of Statistics (PCBS) to demonstrate an increase in the prevalence of stunting among preschool children in Palestine during the period 1996–2006. Although at first glance their results appear different than those herein, the children in their study from the Gaza Strip and the West Bank were grouped separately as compared with the present analysis where all children were grouped together. However, when both are grouped together in the PCBS 2006 study, the mean prevalence of stunting appears to be 10.2%, a number akin to that produced by the present pooled and sensitivity analysis (p ⩽ 0.329 and p ⩽ 0.224, respectively).
The cumulative analyses demonstrate the immediate effect of humanitarian aid on the prevalence of malnutrition and IDA. According to the results, the prevalence of acute malnutrition peaked during 2002, as a possible result of the second Intifada and demonstrated a decrease afterward. In the Ard El Insan [24] study, it was noted that after the release of the USAID study results on malnutrition in Palestine during 2002 [20], considerable resources were provided as emergency food aid by several humanitarian agencies in Gaza. According to Rahim [10], wasting consists of an indicator sensitive to factors like humanitarian-aid assistance and military closures. IDA, on the other hand, demonstrated a peak during the year 1999 and decreased afterward. During that time, the first UNRWA/CDC report [18], presenting the increased prevalence of IDA in Palestinian children, was released and since then iron supplementation was introduced in the majority of humanitarian projects [6]. These findings delineate a dynamic relationship between humanitarian aid and the nutritional status of Palestinian children. It also becomes evident that more effective interventions are needed in order to combat the observed prevalence of IDA and malnutrition. Although the prevalence of malnutrition in Palestine is considered a humanitarian emergency [20], the majority of aid, consisting mainly of oil, powdered milk, wheat flour, rice and sugar, is only being donated to refugee families [24].
Magoni et al. [6] evaluated the impact of the Health Project and humanitarian assistance, consisting of iron and vitamin supplementation and medical follow-up of malnourished children. Eight months after the initiation of the Project, the prevalence of IDA had dropped by 50.0% and global acute malnutrition was reduced by 70.0%. According to the World Bank [44], the management of common childhood infections and malnutrition is the intervention likely to have the greatest impact on reducing the global burden of disease, estimated to be the most cost-effective health intervention in both low-income and middle-income countries. Apart from micronutrient, supplementation for combating child malnutrition, UNICEF also suggests food supplementation (for specific micronutrient deficiencies), infection prevention/treatment, growth monitoring, maternal education about infant feeding practices (including breastfeeding and complementary feeding), and school feeding programs [41]. It is also possible that education on reducing birth frequency and increasing birth spacing would result in more food adequacy. In Palestine there is a large number of children graduates of the primary school who do not continue to the secondary school, either because they get married very young, or because they have to work [41]. Research in Tanzania demonstrated that an additional year of parental education reduces child malnutrition by 8.0%, whereas motor-road access in every village produces a further decrease of 5.0% [45,46]. In Palestine, maternal illiteracy has been demonstrated as a pivotal risk factor for chronic malnutrition in preschool children [7].
One of the limitations of the present study is the inability to use the recently developed Surveys v1.6 algorithm for quality scoring of nutrition surveys, introduced by the Health and Nutrition Tracking System (HTNS, 2010). This was attributed to the fact that many of the components scoring each survey in the algorithm were not reported in the majority of retrieved studies. However, a system was produced for assessing the quality of the selected studies that was useful in identifying research with extrapolated results that were excluded from the sensitivity analyses. The present study provided an objective prevalence for IDA and malnutrition, produced through meta-analyses, and such assessments are needed in order to objectively define the burden of a public health problem and the possible need for effective intervention strategies and humanitarian emergency [47].
Despite the importance of childhood malnutrition, the long duration of conflict in Palestine, and the aid provided by several governmental and non-governmental organizations, the present results indicate that changes have actually been implemented on the nutritional status of Palestinian preschool children. According to the WHO [48], treatment of acute malnutrition in children with less than 5 years of age consists of a priority intervention for immediate implementation, but paradoxically according to the present findings only a small reduction has actually been noted since 1998. Malnutrition surveillance information and objective assessments like the present review can trigger a decision to intervene, provide guidance and assist in program design and planning [14,47,49]. However, the present findings corroborate those by independent research conducted by several organizations providing evidence that malnutrition is still apparent in Palestine. It is important to note that research on such important matters should be published in a fast-track manner and the file-drawer [50] effect must be minimized as much as possible, in order to attain up-to-date results. In addition, these results suggest that each aid/intervention provided has had an immediate response to the nutritional status of the children.
Contributors
Both authors participated in the literature review, statistical analyses and writing the report, and both have seen and approved the final version.
Conflict of interest statement
The authors have no conflict of interest to declare.
References
Cite this article
TY - JOUR AU - Maria Tsigga AU - Maria G. Grammatikopoulou PY - 2013 DA - 2013/01/12 TI - Assessing the silent epidemic of malnutrition in Palestinian preschool children JO - Journal of Epidemiology and Global Health SP - 181 EP - 191 VL - 2 IS - 4 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2012.12.002 DO - 10.1016/j.jegh.2012.12.002 ID - Tsigga2013 ER -
