Impact of the Family Health Program on gastroenteritis in children in Bahia, Northeast Brazil: An analysis of primary care-sensitive conditions
- DOI
- 10.1016/j.jegh.2013.03.002How to use a DOI?
- Keywords
- Family Health Program (Programa Saúde da Família; (PSF); National Unified Health System (Sistema Único de Saúde; (SUS); Pediatric gastroenteritis; Primary care
- Abstract
In seeking to provide universal health care through its primary care-oriented Family Health Program, Brazil has attempted to reduce hospitalization rates for preventable illnesses such as childhood gastroenteritis. We measured rates of Primary Care-sensitive Hospitalizations and evaluated the impact of the Family Health Program on pediatric gastroenteritis trends in high-poverty Northeast Brazil. We analyzed aggregated municipal-level data in time-series between years 1999–2007 from the Brazilian health system payer database and performed qualitative, in-depth key informant interviews with public health experts in municipalities in Bahia. Data were sampled for Bahia’s Salvador microregion, a population of approximately 14 million. Gastroenteritis hospitalization rates among children aged less than 5 years were evaluated. Declining hospitalization rates were associated with increasing coverage by the PSF (P = 0.02). After multivariate adjustment for garbage collection, sanitation, and water supply, evidence of this association was no longer significant (P = 0.28). Qualitative analysis confirmed these findings with a framework of health determinants, proximal causes, and health system effects. The PSF, with other public health efforts, was associated with decreasing gastroenteritis hospitalizations in children. Incentives for providers and more patient-centered health delivery may contribute to strengthening the PSF’s role in improving primary health care outcomes in Brazil.
- Copyright
- © 2013 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- Open access under CC BY-NC-ND license. http://creativecommons.org/licenses/by-nc-nd/4.0/
1. Introduction
The Brazilian health care system has become one of the world’s most ambitious and celebrated models of primary health care (PHC), constitutionally reforming its health system to attempt to provide universal health coverage along the lines of the PHC elements defined by the World Health Organization (WHO) emphasizing equity, community participation, integration, shared financing among the different levels of government, participation by the private sector, and decentralization of health governance from the federal to the municipal level [1,2].
Through its National Unified Health System (Sistema Único de Saúde, or SUS), Brazil launched the Family Health Program (Programa Saúde da Família, or PSF) in 1994. The PSF provides a broad range of primary care services through local family health teams, which include at least one physician, one nurse, one nurse assistant, and four community health agents (agentes comunitário de saúde, or ACS) [3]. Each team is assigned to a designated geographical area and is responsible for enrolling and monitoring the health status of up to 3500 people living in its area, providing primary care, health promotion and education services, and making referrals to other levels of care. As of 2009, 27,324 PSF teams covered 98 million people (50% of Brazil’s population) [4]. The program’s participatory health promotion focus attempts to reduce the progression toward expensive hospital-based care.
The coverage goal of the SUS faces serious obstacles from the volume of care needed to achieve universal access as well as the cost to Brazil’s health financing system. Given considerable investments in the PSF program to date, there has been little research into the extent to which the program is associated with changes in health status while controlling for other variables known to affect health [5–9].
With the revitalized interest in PHC, there has been a growing amount of research internationally in the last two decades on indicators measuring PHC effectiveness. One such indicator, Ambulatory Care Sensitive Conditions (ACSC), developed in 1990, refers to a category of diagnoses for which timely and effective outpatient care can help reduce the risks of hospitalization by either preventing the onset of an illness or condition, controlling an acute episodic illness or condition, or managing a chronic disease or condition [10]. ACSC as indicators of access and quality of primary care were first studied in the United States [10] and later in Canada [11] and Spain [12]. Several studies have shown that high rates of hospitalization for ACSC are associated with gaps in coverage of health services and/or deficient PHC [13–15]. The Brazilian Ministry of Health developed and validated a list of conditions sensitive to primary health care and is referred to as “primary care sensitive conditions” or internações por condições sensíveis à atenção primária (ICSAP). The final ICSAP list was based on systematic literature review, workshops with researchers, physicians, and health managers, peer review by the Brazilian Society for Family and Community Medicine and an official public comment period via Internet [16].
A common ICSAP in children in Brazil is gastroenteritis, which can lead to severe dehydration and death. The mortality rate for children aged less than 5 years in Brazil was 34 deaths per 1000 in 2004; approximately 12% of those deaths were attributable to diarrheal diseases (not including neonatal deaths) [17]. Mortality and prevalence of diarrheal diseases are directly related to socioeconomic status [18,19]. Several studies in Brazil have indicated that good hygiene, improvements in sanitation, and disposal of garbage have had significant impacts on the rate of diarrheal illnesses [20,21]. Given the well-known, measureable factors associated with this ICSAP, we examined the possible association between PSF coverage and declines in gastroenteritis hospitalization rates in children.
The purpose of this study was to examine the impact of the PSF on hospitalization rates for gastroenteritis in children aged less than 5 years. Rotavirus vaccination programs for infants less than 16 weeks of age beginning in 2006 have been associated with declines in childhood mortality and hospitalization rates in Brazil [22]. Therefore, we examine years 1999–2007 before rotavirus vaccination would influence gastroenteritis hospitalization rates appreciably in this population. This ICSAP was evaluated through mixed quantitative and qualitative measures as a surrogate for the effect of primary care provision in Salvador, Bahia and its surrounding municipalities.
2. Materials and methods
Our mixed methods approach was utilized in ascertaining the outcomes of interest to (1) corroborate or test the consistency of findings across different methods; (2) elaborate or interpret findings collected using the other method; (3) design our analytic plan; and (4) explore theories or hypotheses based on differing or inconsistent findings using one or both methods. An adapted conceptual framework guided our approach (Fig. 1).
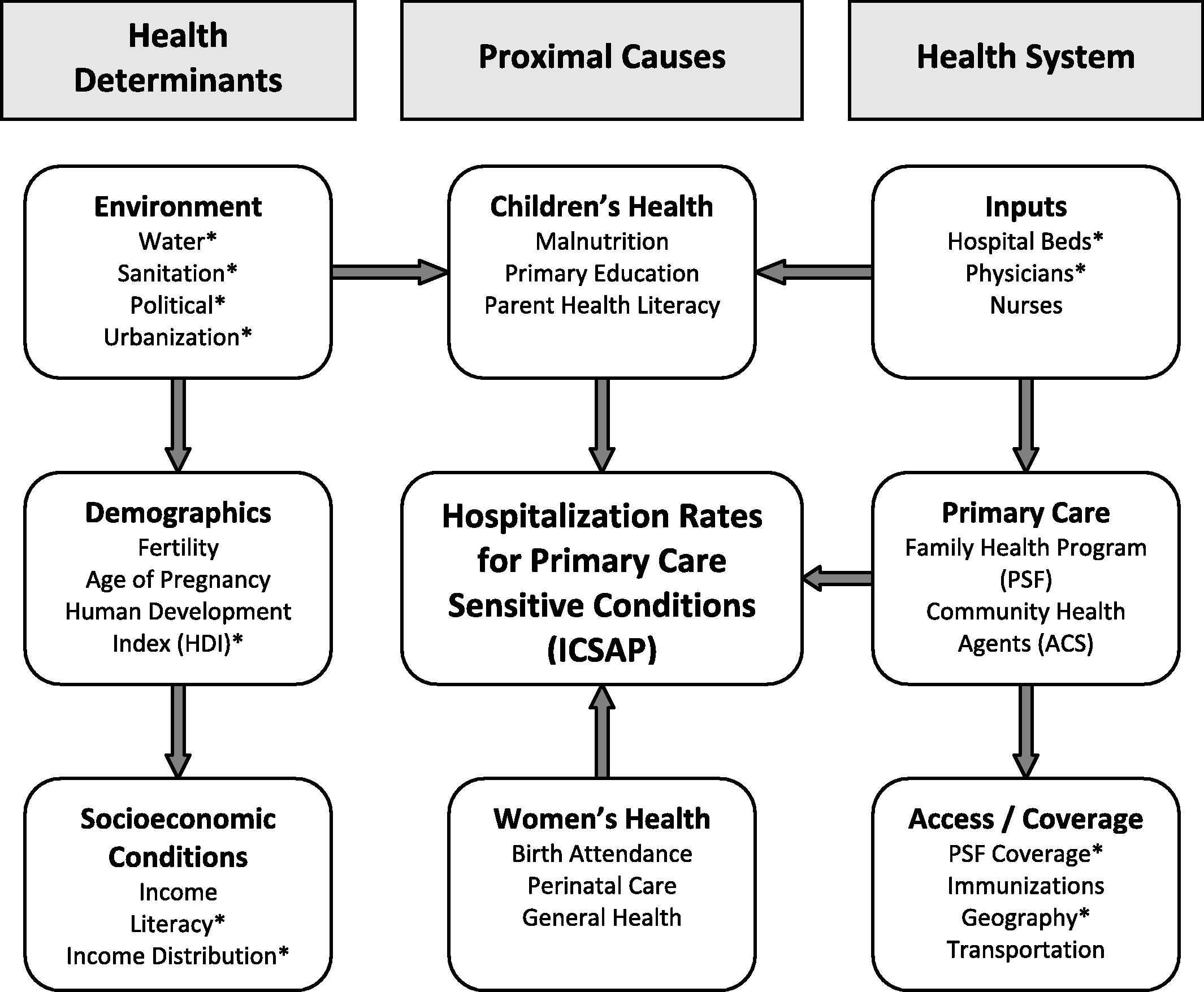
Adapted conceptual framework: determinants of hospitalization for ICSAP [32].
The geographic area of interest for this study was the state of Bahia’s Salvador microregion including the municipal capital, Salvador, Lauro de Freitas, Simões Filho, Candeias, Camaçari, Dias d’Ávila, São Francisco do Conde Madre de Deus, Itaparica, Vera Cruz, and surrounding municipalities of São Sebastião do Passé and Mata de São João. These 12 municipalities (of 417 in the state of Bahia) represent a population of approximately 14 million. The institutional review board and ethics committee of NYU and the ISC-UFBA approved this research study.
2.1. Quantitative analysis
We conducted multivariate longitudinal analyses using panel data for years 1999–2007 to measure coverage by the PSF and corresponding rates of pediatric hospitalizations for gastroenteritis. Data on individual hospitalizations with or without PSF team exposure would be preferred, although no such dataset exists containing the necessary variables per region and year. Hospitalization rates per 10,000 for gastroenteritis (ICD-10 codes: A02.0, A08, A09, J10.8, J11.8, K52.) in children aged less than 5 years were characterized by place of family residence.
The main data source was the SUS Hospital Admissions Information System (SIH–SUS) [23]. These data are produced for the purpose of reimbursing hospitals through the SUS and are made publicly available by the Ministry of Health. The SIH–SUS files were imported for each state monthly for each year of the study period [24]. These files contain detailed information regarding the cause of hospital admission (ICD 10 codes), the age, sex and place of residence of the patient for all SUS hospital admissions. The year of admission was defined by the date of hospital discharge. Population data for calculation of hospital admission rates came from the 2000 census and included projections for 1999 and from 2001 to 2007 [25]. We used the Brazilian government definition of PSF enrollment, number of health teams in each state by average number of enrollees per team, divided by the total yearly state population and expressed as a percentage, used as quintiles [26,27].
Other independent variables known to influence ICSAP include socioeconomic conditions measured by indicators such as proportion of population with adequate water or sanitation [28]; development conditions represented by the human development index (HDI) [29] and proportion of population over age 15 years who are illiterate [23]; and health service indicators including number of physicians per 10,000 [23,28,29].
Fixed effect specification was indicated to correct for serial correlation of repeated measures, accounting for known variability within and between municipalities over time. Regression modeling was used to control for unobservable municipal-level characteristics [30]. Gastroenteritis hospitalization rates were calculated over time for individual municipalities and the aggregate. Modeling was based on stepwise inclusion of exposure variables for regression analyses as well as a priori hypotheses. Analyses were performed using Stata Software (StataCorp. 2007. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP.).
2.2. Qualitative analysis
Key informant interviews were performed in order to further describe and examine findings analyzed from quantitative data sources. Key informants were identified with the assistance of ISC-UFBA in Bahia. Thus, subjects for these interviews were selected by purposive, convenience sampling to achieve descriptive qualitative data on the health system. Interview formats for all subjects were in-depth and open-ended, guided by questions in a semi-structured individual interview guide that was linguistically relevant, and approved by institutional review boards at NYU and ISC-UFBA. A total of 15 key informant interviews were held in private or semi-private designated meeting locations, working with translators as necessary. No incentives were offered to key informants, and no risks were posed to participants.
Interviews were voice recorded with the consent of all individuals present. All voice recordings and interviews were transcribed and translated from Portuguese and/or Spanish to English when applicable. Coding of responses to questions was explored independently, and elucidated descriptive data to be analyzed using an adapted matrix tool [31]. Filtering of data in grounded theory was iterative, occurring first in transcription, dual translation by bilingual research personnel if necessary, and finally coding independently for thematic analysis.
Strategies to address the limitations and subjectivity of qualitative research were employed. To heighten the fidelity and credibility of this study, multiple strategies for rigor in the qualitative methodology were used [31]. Partnership between institutional partners was collaborative and long-standing in an attempt to ameliorate reactivity and respondent bias. Also, prolonged engagement among investigators nurtured an environment of peer debriefing and member checking to ensure ongoing agreement of the study implementation. Lastly, use of a conceptual framework preserved a clear auditing and decision trail.
3. Results
Descriptive statistics (Table 1) show hospitalizations from 1999 to 2007 for gastroenteritis in children aged less than 5 years declined by 39% overall for the region, although rates varied considerably within individual municipalities. Expansion in provision of primary care was described by a ninefold increase in PSF coverage. Where availability of hospital beds increased, the number of doctors per capita decreased during this period. Changes in socioeconomic indicators were mixed. Improvements were made in the HDI, proportion of poor population, and decreasing illiteracy rate. Other factors, including urbanization and income disparity (GINI index), were shown to have a slightly increasing trend but were mostly stable over the period. Notably, considerable increases in the availability of clean water, sanitation, and garbage collection services were observed.
| Mean hospitalization rates | 1999 | 2007 | Change in mean 1999–2007 | (%) | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| 1999 | 2007 | Change in mean 1999–2007 | (%) | |||
| Bahia (12 municipalities) | 599.31 | 524.05 | 362.35 | 356.14 | −236.96 | −39.54 |
| Hospitalization rates by municipality | Change in rate 1999–2007 | |||||
| Camaçari | 181.70 | 193.72 | 12.03 | 6.62 | ||
| Candeias | 163.86 | 394.09 | 230.23 | 140.50 | ||
| Dias d’Ávila | 40.31 | 169.38 | 129.06 | 320.14 | ||
| Itaparica | 1240.04 | 1271.57 | 31.54 | 2.54 | ||
| Lauro de Freitas | 536.10 | 69.72 | −466.38 | −86.99 | ||
| Madre de Deus | 404.04 | 380.23 | −23.81 | −5.89 | ||
| Mata de São João | 1010.10 | 308.55 | −701.55 | −69.45 | ||
| Salvador | 1146.32 | 169.46 | −976.86 | −85.22 | ||
| São Francisco do Conde | 65.62 | 204.20 | 138.58 | 211.20 | ||
| São Sebastião do Passé | 595.39 | 359.80 | −235.59 | −39.57 | ||
| Simões Filho | 213.81 | 201.73 | −12.08 | −5.65 | ||
| Vera Cruz | 1594.46 | 829.99 | −764.48 | −47.95 | ||
| 1999 | 2007 | Change in mean 1999–2007 | (%) | |||
| Mean | SD | Mean | SD | |||
| Independent and control variables | ||||||
| PSF coverage (%) | 7.30 | 16.21 | 66.21 | 33.28 | 58.90 | 806.41 |
| Hospital beds (per 1,000) | 663.25 | 2074.89 | 844.67 | 2597.93 | 181.42 | 27.35 |
| Illiteracy rate (per 10,000) | 14.12 | 4.30 | 9.14 | 3.02 | −4.98 | −35.27 |
| Population with access to permanent clean water supply (%) | 78.66 | 13.03 | 93.96 | 9.77 | 15.29 | 19.44 |
| Population with access to permanent sewage and sanitation services (%) | 54.32 | 19.11 | 75.87 | 30.54 | 21.55 | 39.68 |
| Population with access to permanent garbage collection services (%) | 71.84 | 14.34 | 95.52 | 6.85 | 23.68 | 32.97 |
| Human development index (HDI) | 0.54 | 0.33 | 0.60 | 0.36 | 0.06 | 11.34 |
| Urbanization (%) | 89.43 | 9.08 | 92.60 | 8.75 | 3.16 | 3.54 |
| GINI index | 0.45 | 0.28 | 0.46 | 0.28 | 0.01 | 2.58 |
| Population poor (%) | 47.63 | 8.46 | 42.00 | 7.74 | −5.63 | −11.83 |
| Number of doctors (per capita) | 0.26 | 0.67 | 0.24 | 0.70 | −0.01 | −5.21 |
Descriptive characteristics. Hospitalizations for gastroenteritis, children aged less than 5 years (per 10,000 population).
Rates of hospitalization for gastroenteritis across municipalities were variable in distribution across the region (Fig. 2). Trends in hospitalizations per capita by municipality were variable, but in general showed decreasing hospitalization rates among children aged less than 5 years for gastroenteritis (Table 1). When not assuming equal variances between the individual municipalities, the mean hospitalization rates for gastroenteritis among children aged less than five years were not significantly different (P = 0.766). This apparent variation between municipalities was further illustrated by both high PSF coverage and greatest hospitalizations being linked together (rather than being inversely proportional) in municipalities such as Vera Cruz, Mata de São João and São Sebastião do Passé. Other municipalities of Bahia tended to follow the hypothesis that as PSF coverage increases gastroenteritis hospitalizations will decrease.
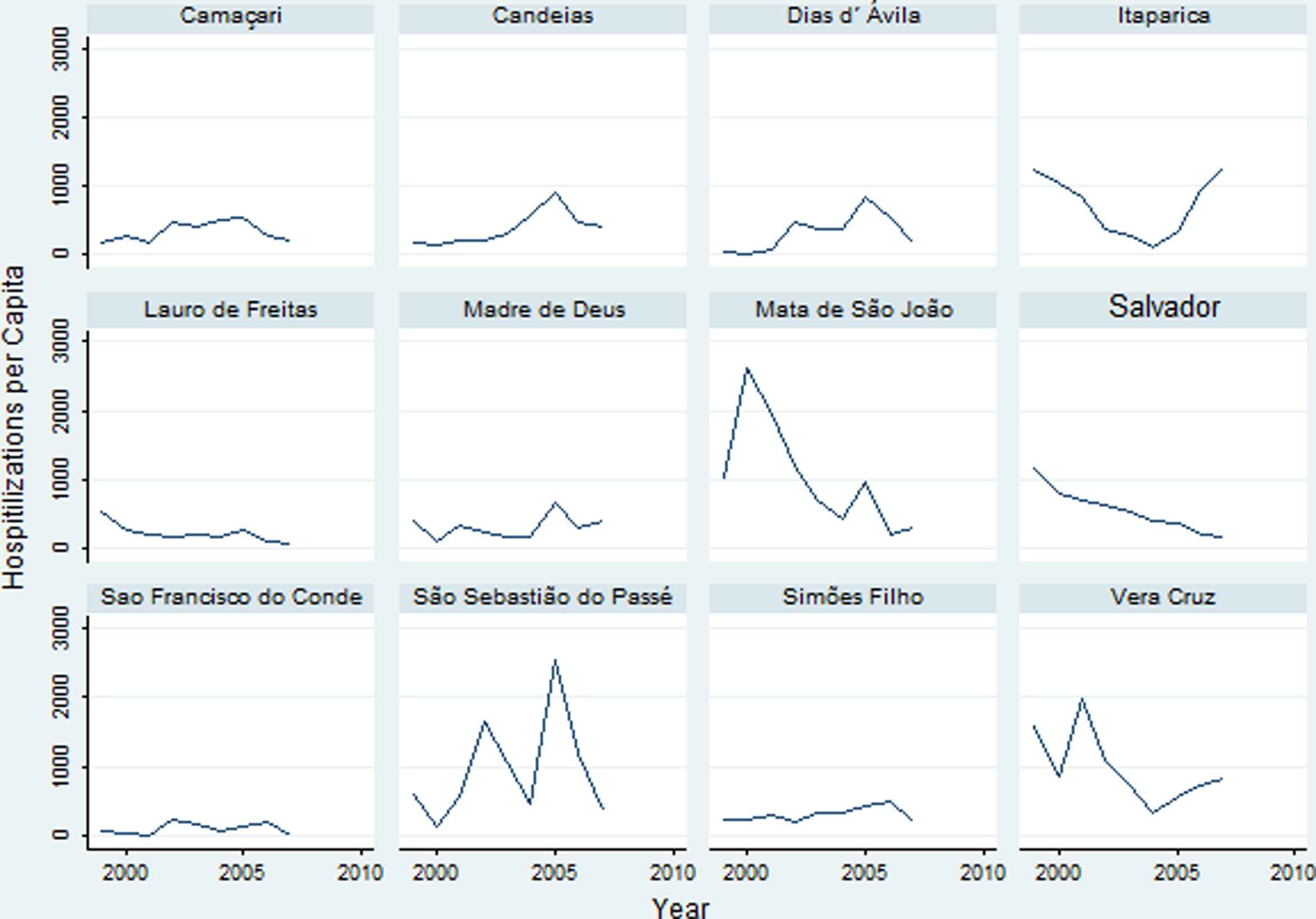
Rates of gastroenteritis hospitalizations in children ages <5 years per capita, 1999–2007.
PSF coverage is described in regression models (Table 2) that control for within municipal variation of socioeconomic factors with fixed effects specification. Coverage by PSF was significantly associated with decreases in hospitalization rates with adjustment for increases in the HDI. However, after accounting for increasing clean water availability, permanent sanitation, and garbage collection services (Model 3) this association was no longer statistically significant. Thus, this measure of primary care provision was not shown to be a significant predictor independent of the effects of water availability, sanitation, and garbage collection.
| Model 1a | Model 2c | Model 3 | |
|---|---|---|---|
| Coefficient | Coefficient | Coefficient | |
| Coverage by PSF (SE)b | −3.07 | −3.12 | −1.83 |
| (1.14) | (1.15) | (1.60) | |
| Constant | −1792.86 | −1211.50 | −2565.02 |
| (2503.20) | (2430.06) | (3210.28) | |
| Observations | 12 | 12 | 12 |
| Municipalities | 12 | 12 | 12 |
| R-squared (within) | 0.11 | 0.12 | 0.30 |
| P-value | 0.021 | 0.020 | 0.278 |
Robust standard errors are in parentheses. All models are adjusted for number of hospital beds per 1000 population, illiteracy rate, urbanization, GINI index, proportion of poor, and number of doctors per capita.
Model 1: Adjusted specification for PSF coverage.
Model 2: Adjusted specification for PSF coverage, controlling for HDI.
Model 3: Adjusted specification for PSF coverage, controlling for HDI, permanent sanitation structure, clean water availability, and garbage collection service.
Significant at P < 0.05.
Family Health Program (PSF) Coverage. Fixed effect regression modelsc for Bahia municipalities, 1999 to 2007.
Qualitative results do suggest some effect of PSF on health outcomes in the region. Results are grouped using domains identified in the adapted conceptual framework (Fig. 1). Health determinants affecting gastroenteritis included factors in the physical and political environments, demographics, and socioeconomic conditions (Fig. 3).
3.1. Environment
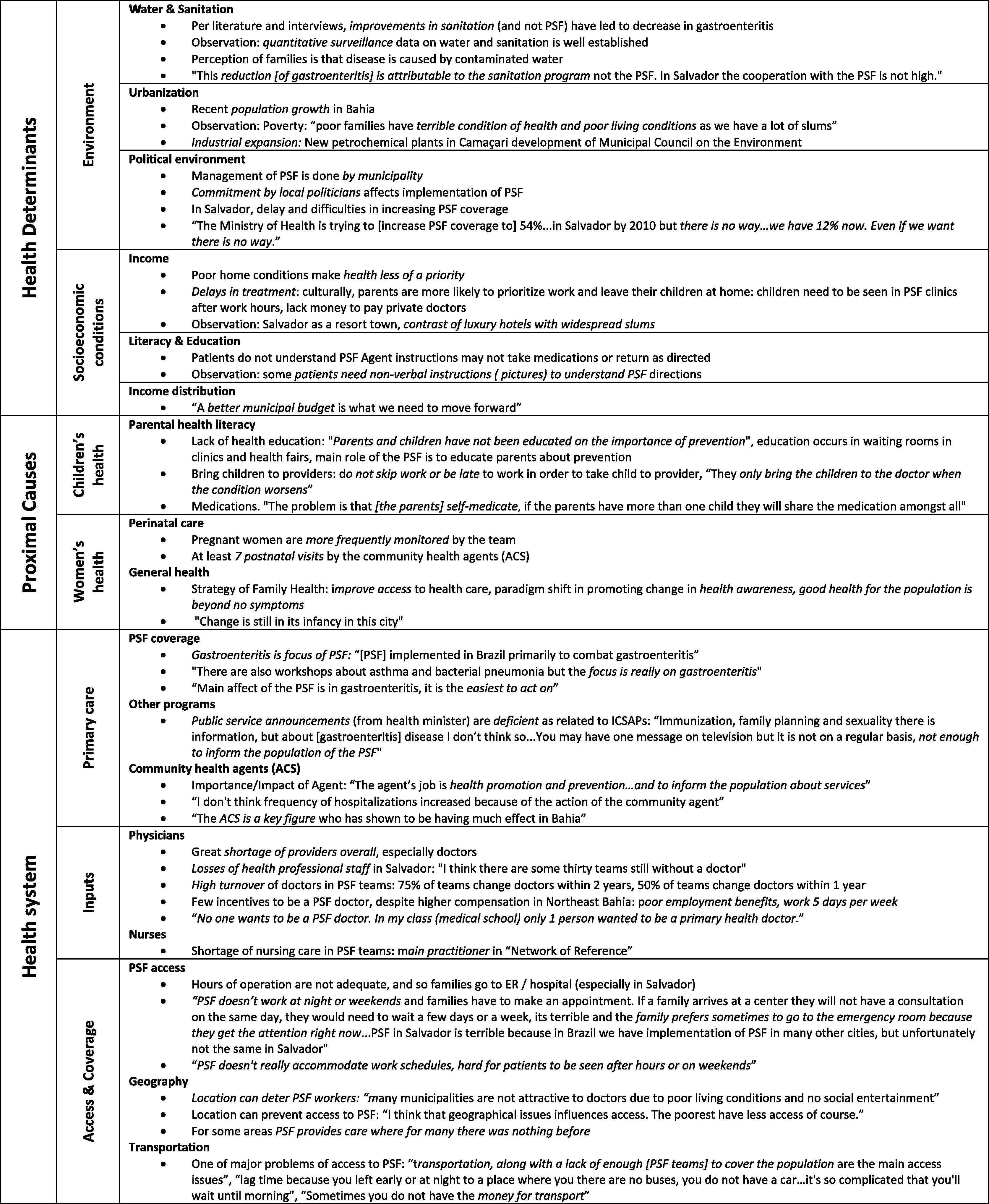
Matrix of topics, themes, and sub-themes. Qualitative analysis from key informant interviews on gastroenteritis.
A number of key factors surfaced in both physical and political environments. One major theme emerging from key informant interviews in terms of physical environment was that decreases in hospitalizations for gastroenteritis were due to improvements in sanitation, not health systems. “This reduction [of gastroenteritis] is attributable to the sanitation program not the PSF. In Salvador the cooperation with the PSF is not high.” Anxiety was expressed over urbanization and its effect on health. When asked about living conditions, another informant remarked, “poor families have terrible condition of health and poor living conditions as we have a lot of slums.” An unexpected theme emerging from several interviews was the effect of the political environment on PSF coverage. Management of the PSF is decentralized and directed by each municipality. Thus, local politicians’ priorities affect implementation of the PSF. In Salvador, there have been delays and difficulties in increasing PSF coverage partly due to changes in the political arena and prioritization of PSF improvements.
3.2. Socioeconomic conditions
Salvador is regarded as a resort town in Northeast Brazil but contains a considerable amount of poverty. Compelling contrasts between luxury hotels and widespread slums were observed. Some key informants remarked that poor home conditions make health less of a priority. Parents delay care because the PSF is unavailable after working hours or they cannot afford a private physician. Regarding literacy and education, some informants commented that patients do not always understand instructions given by the PSF agents and may not return to clinics for follow-up. One informant observed, “some patients need non-verbal instructions (e.g. pictures) to understand PSF directions.”
3.3. Proximal causes women’s health and parental health literacy
In Bahia, pregnant women, particularly first-time mothers, are provided with a vast amount of information. Key informants described this situation as a “key entry point” for accessing health services through the PSF. While this point seems clear, observations and discussion with researchers and health professionals in Salvador divulged the complexity of navigating the health system by parents. Unavoidable in conversations of parental health literacy, key informants described how socioeconomic factors affected health-seeking behaviors for ICSAP among parents. One key informant stated: “They only bring the children to the doctor when the condition worsens... to avoid not skipping work or being late.” Another key informant described the problematic factors related to the observed, apparent increase in hospitalizations for some ICSAP as failures to address access to care, stating: “Good health for the population is beyond no symptom of illness... the strategy is to improve access to care... and this change is still in its infancy in this city.”
3.4. Health system
Most key informants had opinions about the health system overall, as well as the PSF specifically. At state and municipal levels, shortage of doctors willing to work in the PSF was cited as a major reason why implementation was not more pervasive. Upstream issues, including medical school culture, result in fewer doctors engaged early on in becoming primary care professionals. One PSF doctor noted, “In my class at medical school, only 1 person [of 200] wanted to be a primary care doctor.” Even those who are attracted initially tend to leave early on. Informants noted that about one-half of PSF teams changed doctors within 1 year and few remained unchanged after 2 years. Reasons given for the high turnover included poor benefits, lack of job security, longer working hours (versus private or specialty practice), and lower perceived professional status.
3.5. Primary health care
Informants described gastroenteritis among children as “the focus of the PSF”, given “it is the easiest to act on.” The ACS has the primary promotion and prevention role. They are required to live in the community in which they work and these are seen as good positions. “The ACS is a key figure who has shown to be having much effect in Bahia.” Other programs were also described to have an effect. Disease-specific public information does not appear to be widespread, however. One informant noted, “[for] immunization, family planning and sexuality there is information, but about disease I don’t think so.”
4. Discussion
The overall goal for this project was to assess the effect of the PSF on hospitalizations in children aged less than 5 years in the context of the ICSAP, gastroenteritis. According to the analysis, gastroenteritis hospitalizations trended downward between 1999 and 2007 in the 12 municipalities examined in Bahia. Using the conceptual framework (Fig. 1), there were a number of factors in addition to PSF contributing to hospitalization rates. From a quantitative perspective, factors related to permanent sewage systems and garbage collection were significantly associated with decreasing hospitalizations for gastroenteritis, whereas after controlling for these factors PSF coverage was not. These negative correlations were found to remain significant when controlling for factors including HDI, urbanization, and the proportion of poor population in a given municipal unit. Private/permanent water supply was not significantly associated with gastroenteritis hospitalization rates in regression models, although other studies describe water sources’ greater impact on mitigating burden of gastroenteritis among children [32].
Qualitative analysis and the literature review were both strongly supportive of sanitation system improvements as the primary reason for the decrease in gastroenteritis hospitalizations. The PSF, however, has had an impact by providing families with education on recognition of symptoms, oral rehydration therapy, and use of proper hand-washing techniques in preventing the spread of infection. Health care prevention activities have been disseminated through radio, community health fairs, in clinic waiting rooms and by agents in families’ homes.
The paradigm shift described by officials in the PSF has increased the level of health awareness, but not necessarily changed conditions predisposing poorer families to delay care, failing to see a primary care provider early, and resulting in child hospitalizations. Anecdotal evidence from qualitative interviews described poor individuals and families in Bahia spending an entire month’s salary to purchase health services for their sick child because of both an aversion to being seen as “lower” socioeconomic status and concerns for having their children’s needs met, such as being seen in a timely manner and when parents are available during late hours. Despite such concerns, the PSF also provides a place for acute medical care outside of the hospital setting, offering more preventive care. In municipalities with limited access to care and low PSF coverage, such as in Salvador, the PSF most likely has less of an impact than in those with better coverage. Further, larger studies using time-series analysis of the Northeast region of Brazil or all Brazilian municipalities covered by the PSF have described a robust effect on childhood gastroenteritis and other ICSAPs. For instance, in an analysis of aggregated data from Brazil’s 558 microregions important variation was present in hospitalization rates for ICSAPs stratified by municipalities with predominantly private or nonprofit hospital beds [33].
Alternatively, recent studies of gastroenteritis hospitalization rates associated with national programs for rotavirus vaccination in infants. Following the initiation of routine vaccination in 2006, significant declines were observed in rates of ages less than 5 years diarrhea-related mortality and hospital admissions in Brazil, with most pronounced decreases among children less than age 2 years where vaccine exposure was most prevalent [22]. The stabilization of gastroenteritis following control of sanitation and hygiene-related factors along with evidence of subsequent declines after initiation of routine rotavirus vaccination lends support to global and national recommendations for vaccination of infants as an important component to control this primary care-sensitive hospitalization.
SIH–SUS is a limited dataset; only information from the public payer system is included. Less than 20% of the population in Bahia has private health insurance; however this does not preclude them from coverage by the PSF. This makes it challenging to look broadly at public health in the region and make comparisons between outcomes in the private versus the public systems. The data are aggregated at the municipal level, making it difficult to infer individuals’ risk (ecological fallacy). The dataset for our particular investigation did not include some variables of interest, such as mortality due to gastroenteritis, all relevant disease codes, and data were missing or incomplete for some included variables (e.g. number of nurses per capita). Also, greater variation in rates in some municipalities can be described qualitatively as a function of changes in access to care or clinic infrastructure and controlled in regression analyses; validation of reporting to SUS prompted us to analyze all municipalities versus only those with stable rates, using fixed-effect specification to account for this variability. Despite this specification, it is possible that residual confounding by important covariates that are unknown or unmeasured exists in our model.
Qualitative data were limited to only a small purposive sample. Although information obtained was rich in content, such sampling may have contributed to a selection bias since all of those interviewed were or had been at an administrative level in the health system with the exception of two physicians. Language and cultural barriers may have contributed to misunderstanding or misinterpretation of key informant comments. Exposure to more clinics would have benefitted the study in terms of additional direct observations and increasing the number of interviews. The study also has limited generalizability due to the small geographic area examined relative to all of Brazil.
With the use of these ecological data and our qualitative findings, this analysis is limited to answering scientific questions specific to the Salvador microregion only. Thus, our study is intended to be hypothesis-generating rather than providing a basis for causal inference. Our investigation adds to the current literature describing associations between PSF coverage and ICSAPs, including childhood gastroenteritis hospitalizations, by providing a qualitative context (conceptual framework) to covariates typically only measureable at an ecologic level.
5. Conclusions
We conclude that public health efforts in the Salvador microregion, particularly those pertaining to infrastructure for sanitation and hygiene, rather than coverage by the PSF explain greater variation and improvement in hospitalization rates for gastroenteritis in children. Direct inputs into the PSF, such as incentives for provider entry and more patient-centered, convenient working hours, could contribute to strengthening the PSF’s role in improving primary health care outcomes in Brazil.
Competing interests
None.
Ethics approval
This study was conducted with the approval of the institutional review board at New York University and the ethics committee at Universidade Federal da Bahia.
Contributorship
All authors (L.J.M., G.S.C., P.N., M.S., M.C., E.M. and I.D.) were involved in the study design. G.S.C. and M.S. developed epidemiologic causal models. G.S.C. performed the statistical analysis and is the corresponding author for the paper. L.J.M. wrote the initial draft, and G.S.C., P.N. and M.S. assisted with the formatting and editing of the manuscript. All authors participated in the interpretation of the results, revising of the manuscript for important intellectual content and approval of the final draft.
Financial support
Funding for research in the New York University, Global Institute of Public Health was granted by the Macy Foundation. G.S.C. is supported by the National Institutes of Health Cancer Prevention Training Grant in Nutrition, Exercise & Genetics at the University of Washington and Fred Hutchinson Cancer Research Center (R25CA094880).
Acknowledgements
We are grateful to the following individuals and for their assistance and support: The Macy Foundation; at Instituto de Saúde Coletiva-UFBA, Bárbara Laisa Alves Moura and Renata Castro da Cunha; New York University Global Public Health faculty, Kristin Bright and James Macinko, and coordinator, Amy Joyce; Data Services and Support, Frank Lopresti, Mashfiqur Khan, Melissa Reese, and Himanshu J. Mistry; Language interpreters and translation, José Tadéu Tramontini Filho, Rita Soto, and Solange Figueiredo; Our colleagues at New York University, especially Ana Krieger. We are thankful to the editor and two referees whose constructive comments have helped us to improve the presentation of the paper.
References
Cite this article
TY - JOUR AU - Laura J. Monahan AU - Gregory S. Calip AU - Patricia M. Novo AU - Mark Sherstinsky AU - Mildred Casiano AU - Eduardo Mota AU - Inês Dourado PY - 2013 DA - 2013/04/13 TI - Impact of the Family Health Program on gastroenteritis in children in Bahia, Northeast Brazil: An analysis of primary care-sensitive conditions JO - Journal of Epidemiology and Global Health SP - 175 EP - 185 VL - 3 IS - 3 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2013.03.002 DO - 10.1016/j.jegh.2013.03.002 ID - Monahan2013 ER -
