Acute Pancreatitis: An Exploratory, Cross-sectional, Single-center Study of the Epidemiological Features of the Disease in a Sample of Saudi Patients
- DOI
- 10.2991/jegh.k.190524.001How to use a DOI?
- Keywords
- Acute pancreatitis; epidemiology; etiologies; mortality; Saudi Arabia
- Abstract
Epidemiological studies on Acute Pancreatitis (AP) are significantly scarce in the Saudi Arabian Literature. In this paper, we aim to explore the current trends of AP in a sample of Saudi patients. This is a cross-sectional study in which we reviewed AP-related admissions from 2014 to 2017. Data collected included demographics, clinical presentation, investigations, severity, complications, and the outcome at the end of hospitalization. During the study period, 107 patients were admitted due to AP. Fifty-seven (53%) were males. Biliary pancreatitis was the most common etiology found among our patients (39.3%; 95% CI: 30.5–48.7), followed by alcoholic pancreatitis (11.2%; 95% CI: 6.5–18.6) and hypertriglyceridemia (8%; 95% CI: 4.5–15.2). Pancreatic pseudocysts were the most common complication we found in this series (15%; 95% CI: 9.4–23). Of all the hospitalized patients in this study, eight patients (7.9%) died (95% CI: 3.8–14.1). The number of AP-related admissions and mortality rate appear to have increased as compared with the numbers in earlier national studies. The etiological groups have also changed. As compared with Western/Asian studies, however, there was almost no difference in the epidemiological patterns except for the mortality rate.
- Copyright
- © 2019 Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Acute Pancreatitis (AP) is a medical emergency that can vary in presentation from mild- or self-limiting disease to severe or fatal when it extends beyond the pancreas to cause multiorgan damage. Understanding the pattern of the disease including the etiology, severity, mortality, and its predictors in a given population is essential in guiding the management, preventing recurrence, decreasing morbidity and mortality, and ensuring optimal delivery of care [1]. However, epidemiological studies that address these factors, especially in the Middle East, are lacking significantly. In the Saudi Arabian literature, the most recent studies on the subject were published in 2001 and 2003 by Al-Karawi et al. [2] and Singal et al. [3], respectively. Both were single-center-studies that analyzed the hospital admissions due to AP over an extensive period (12 years). In these two studies, there was a remarkable difference in the number of AP-related hospitalizations between different regions of the kingdom. Mortality also varied between 1.8% in the south and 4.2% in the central areas. Biliary pancreatitis was the most common etiology found in both studies.
Although these studies were helpful in establishing a basic understanding of the epidemiological features of AP in the Saudi population, a lot has changed over the past 15–17 years. Risk factors such as smoking [4], obesity [5], and alcohol consumption [6] have become major health concerns worldwide and have been, of late, contributing to more health issues than ever. However, significant advances in critical care, surgical, and endoscopic management have taken place. Accordingly, one can only assume that both the incidence and AP-related complications and deaths have also changed. The existing evidence from Western countries on these two variables shows conflicting trends [7]. Over the past decade, some studies reported an overall decrease in the incidence [8], whereas others reported a steady increase in the number of AP-related hospitalizations [9]. Contrarily, mortality was consistently reported to decrease in most American and European studies [10–12].
In this paper, using data from a single, high-volume, tertiary care center in Riyadh, we aim to explore the current trends of AP in a sample of Saudi patients, the main areas of focus being the number of hospitalizations per year, etiologies, severity, mortality, and complications.
2. MATERIALS AND METHODS
This is an exploratory, cross-sectional, single-center study in which we retrospectively reviewed all the admissions that took place due to AP between September 2014 and November 2017. The criteria used for diagnosis were: (1) new-onset upper abdominal pain/tenderness; (2) elevation in serum levels of pancreatic enzymes of three or more folds; and (3) radiological changes suggestive of AP. The diagnosis was made if two of these criteria were present [13]. Data collected included basic demographics (age and gender), clinical presentation, etiologies, radiological and lab abnormalities, complications, and the outcome at the end of admission (death or discharge). In addition, the Bedside Index for Severity in Acute Pancreatitis (BISAP) score was calculated based on the clinical evaluation, vital signs, and lab values during the first 24 h of presentation.
The etiology of pancreatitis was determined based on the admission notes (i.e., medical history, medications, alcohol intake, and other risk factors), and on the investigations that were undertaken during the hospital course. Biliary pancreatitis was diagnosed if there was radiological evidence of cholelithiasis or choledocholithiasis. Alcohol-induced pancreatitis was diagnosed based on the patient’s history, and when no other causes of pancreatitis could be identified on investigations [1]. Autoimmune and metabolic causes (i.e., hypertriglyceridemia and hypercalcemia) were investigated through biochemical lab tests. Although many references suggest a triglycerides (TG) level of ≥1000 mg/dL to make the diagnosis of hypertriglyceridemic pancreatitis [14], the risk for AP is present across all individuals with high TG levels [14–16]. In addition, many of our patients who were known to be suffering hypertriglyceridemia were already undergoing treatment when they were admitted, which disqualified many of them on the 1000 mg/dL criterion. Therefore, the diagnosis of hypertriglyceridemic AP was based on high TG levels and the absence of other etiologies. The patient was labeled to have traumatic or Endoscopic Retrograde Cholangio-Pancreatography (ERCP)-induced pancreatitis solely based on history. However, they were labeled to have recurrent acute pancretitis when at least two episodes of AP occurred with complete resolution of symptoms in between, and when the morphological criteria for chronic pancreatitis were absent on imaging. As for idiopathic pancreatitis, as the name suggests, the diagnosis was made when imaging did not reveal any biliary or malignant causes; the patient had no history of ERCP, alcohol intake or use of pancreatitis-inducing medications, and biochemical investigations failed to identify any other etiologies.
2.1. Statistical Analysis
All tests in this section were performed using Minitab®, LLC (Pennsylvania, USA) 18 statistical analysis software. Patient demographics and clinical characteristics were reported as percentages or proportions for dichotomous or polychotomous variables, or as means ± standard deviations (SD) for numerical variables. Etiological groups were then differentiated within the sample and were represented by percentages and 95% confidence intervals (CIs). Mortality, severity, and the prevalence of complications were calculated similarly.
After analyzing the data to extrapolate the essential characteristics of the sample, the sample was divided into subgroups based on age, gender, and, in some parts, etiology to allow making comparisons between them. Differences between these subgroups in terms of mortality, complications, and the relative prevalence of etiologies were compared. The method of comparison was CIs and two-tailed hypothesis testing. Because hypotheses generation in this study was done post hoc and multiple comparisons were made, Bonferroni adjustment was used to correct for type I error. The significance level (alpha level) after correction is mentioned in the subsequent section for each corresponding hypothesis.
When hypothesis testing showed a statistically significant difference between subgroups, further analysis was performed using Chi-square test of independence and logistic regression analysis to examine the relationship between variables.
3. RESULTS
During the study period, 107 patients were admitted due to AP, fifty-seven of whom (53%) were males. The participants’ ages ranged between 14 and 98 years (mean age ± SD: 48 ± 19 years). Expectedly, the most common presenting symptom was abdominal pain (97%), followed by nausea or vomiting (76%). Only 11 patients (10.3%; 95% CI: 5.8–17.5) were admitted with a BISAP score of 3 or more (severe AP).
Etiological groups were as follows: biliary pancreatitis was the most common etiology found in this series of hospitalizations. Of the 107 patients included, 42 patients (39.3%; 95% CI: 30.5–48.7) had evidence of a biliary cause. Alcoholic pancreatitis was the second most common etiology leading to 11.2% of the admissions (95% CI: 6.5–18.6). Other etiologies of AP included hypertriglyceridemia (8% of patients; 95% CI: 4.5–15.2) and post-ERCP pancreatitis (4.7%; 95% CI: 2–10.5). Medications and pancreatic malignancies both contributed to an equal number of hospitalizations (2.8%; 95% CI: 1–7.9) and were followed by traumatic and autoimmune causes (1.9% of hospitalizations for each; 95% CI: 0.5–6.6). Eight participants in this series (7.5%; 95% CI: 3.8–14.1) were found to have multiple etiologies that may have contributed to their pathology. With that in mind, the number of AP cases that were caused by an underlying biliary pathology, autoimmune processes, ERCP, medications, and hypertriglyceridemia increased as shown in Table 1. In addition, a group of four patients was identified to have infectious causes. Less common causes and risk factors of AP in this series included Bioenteric Intragastric Balloon compression [17], perforated duodenal ulcers [18], congenital anatomical pancreatic ducts alterations (divisum) [19], and peritoneal dialysis [20]. Each of these factors contributed to one admission only (0.9%; 95% CI: 0.2–5.1). Despite thorough investigations, 16 patients in our review (15%; 95% CI: 9.4–22.9) had no identifiable causes of AP. Recurrent AP occurred in 33 patients (31%; 95% CI: 24–42), most commonly due to biliary stones (33% of recurrent cases), hypertriglyceridemia (18%), alcohol (15%), and idiopathic causes (12%).
| Etiology | Number (%) (95% CI) | Including patients who had multiple etiologies |
|---|---|---|
| Biliary | 39.3 (30.5–48.7) | 46.7 (37.6–56.1) |
| Hypertriglyceridemia | 8 (4.5–15.2) | 11.2 (6.5–18.6) |
| Post-ERCP | 4.7 (2–10.5) | 7.5 (3.8–14.1) |
| Drug-induced | 2.8 (1–7.9) | 6.5 (3.2–12.9) |
| Infectious | None | 3.7 (1.5–9.2) |
| Autoimmune | 1.9 (0.5–6.6) | 5.6 (2.6–11.7) |
CI, confidence interval.
Etiologies with patients who have multiple causes
Gender-based differences between males and females in the relative prevalence of etiologies were pronounced in most etiological subgroups Figure 1. However, running a Z-test of two-tailed hypotheses showed that none of these differences was statistically significant at p < 0.004 except for alcoholic pancreatitis.1 Males had 12 times more admissions for the latter (p = 0.00058). Comparison among different age groups in the relative prevalence of etiologies Figure 2 showed that biliary pancreatitis was most commonly seen among elderly patients (64% of cases; 95% CI: 45–80; p = 0.0039). However, middle-aged patients (30–59 years) exhibited the highest relative prevalence of alcoholic pancreatitis (p < 0.001).2 These differences between age and gender subgroups were further examined using the Chi-square test of independence. As shown in Tables 2–4, our sample showed statistically significant associations between biliary pancreatitis and patients above 60 years (p < 0.009) and between alcoholic pancreatitis and middle-aged (p < 0.005) males (p < 0.001).
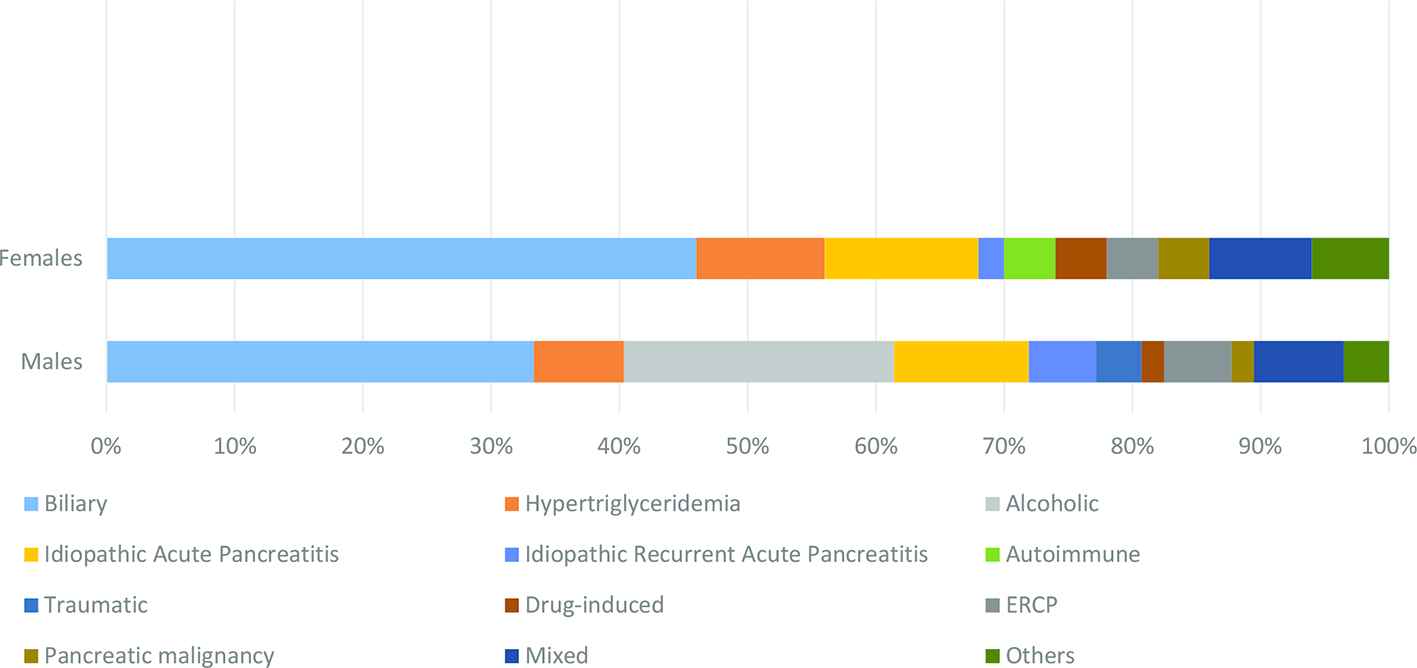
Etiological groups by gender.
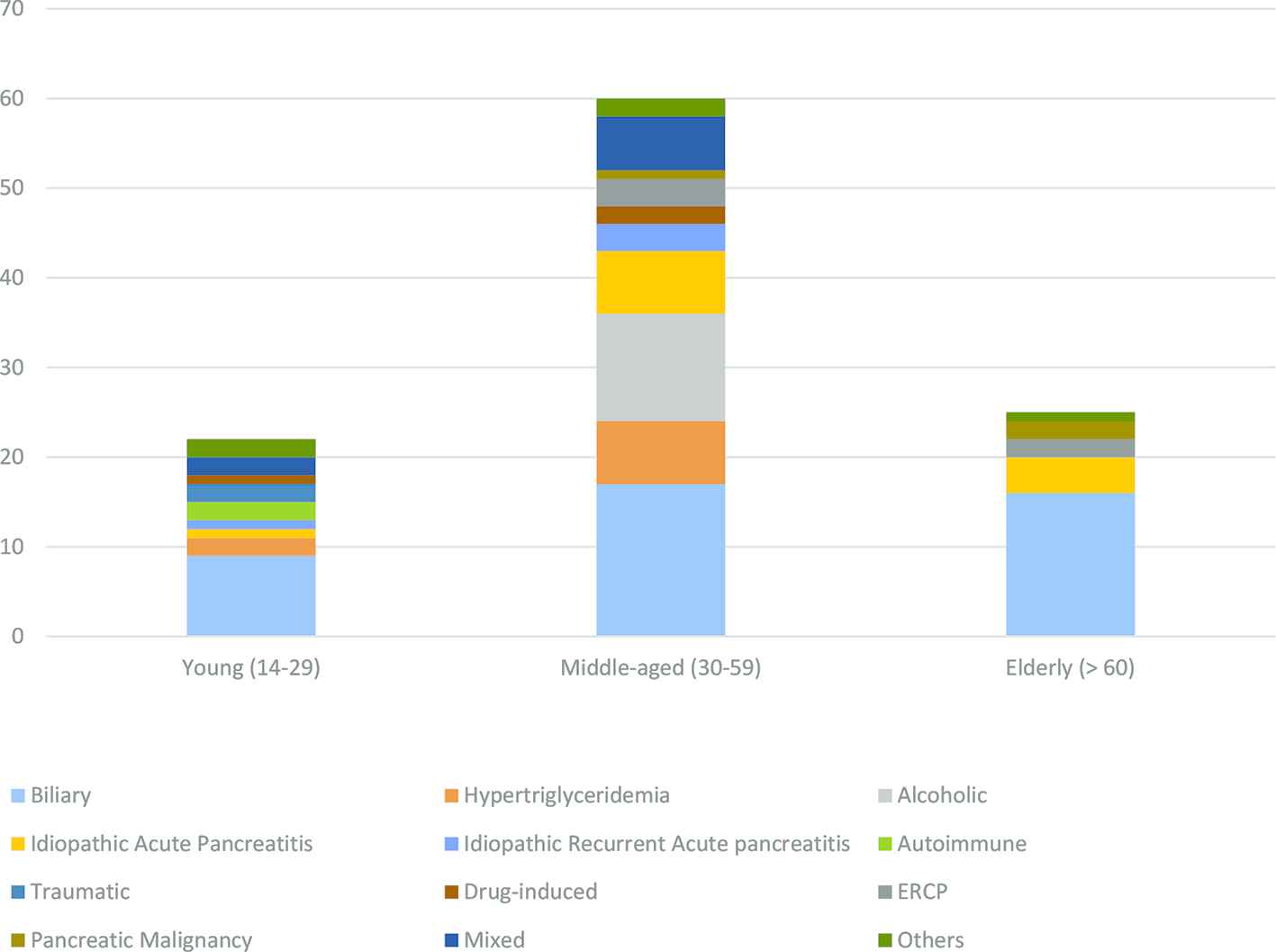
Age distribution of etiological groups.
| Alcoholic | Non-alcoholic | All | |
|---|---|---|---|
| Males | 12 (6.393) | 45 (50.607) | 57 |
| Females | 0 (5.607) | 50 (44.393) | 50 |
| All | 12 | 95 | 107 |
| Chi-square | DF | p-value | |
| Pearson | 11.856 | 1 | 0.001* |
Alpha level 0.05.
Association between gender and alcoholic pancreatitis using Chi-square test
| Biliary | Non-biliary | All | |
|---|---|---|---|
| Young (14–29) | 9 (8.64) | 13 (13.36) | 22 |
| Middle (30–59) | 17 (23.55) | 43 (36.45) | 60 |
| Old (>60) | 16 (9.81) | 9 (15.19) | 25 |
| All | 42 | 65 | 107 |
| Chi-square | DF | p-value | |
| Pearson | 9.446 | 2 | 0.009* |
Alpha level 0.025.
Association between age and biliary pancreatitis using Chi-square test
| Alcoholic | Non-alcoholic | All | |
|---|---|---|---|
| Young (14–29) | 0 (2.467) | 22 (19.533) | 22 |
| Middle (30–59) | 12 (6.729) | 48 (53.271) | 60 |
| Old (>60) | 0 (2.804) | 25 (22.196) | 25 |
| All | 12 | 95 | 107 |
| Chi-square | DF | p-value | |
| Pearson | 10.587 | 2 | 0.005* |
Alpha level 0.025.
Association between age and alcoholic pancreatitis using Chi-square test
The most common complication that was found in this series was pancreatic pseudocysts (15%; 95% CI: 9.4–23). Peripancreatic fluid collections were also present in 9% of cases (95% CI: 4.3–15.7). Less commonly, necrotic changes to the parenchyma of the pancreas were seen in 3.7% of patients (95% CI: 1.5–9.2), one patient progressed into chronic pancreatitis (0.9%; 95% CI: 0.16–5), and another developed splenic vein thrombosis. Males had a higher rate of developing pancreatic pseudocysts and peripancreatic fluid collections than females (p < 0.005).
Of the 107 patients who were hospitalized during the study period, eight patients died (7.9%; 95% CI: 3.8–14.1). Of all the variables collected for the study and incorporated into the logistic regression analysis, the BISAP score was the only significant factor associated with mortality.
4. DISCUSSION
Acute pancreatitis is an inflammatory condition that varies in presentation from mild- and self-limiting disease to a severe and fatal one. There is a significant dearth of epidemiological studies on AP in the Middle Eastern literature. In this literature, there have been conducted only two studies on the subject in the early 2000s [2,3], and none after 2005. Over 18 years, one can assume that changes in the incidence of AP might have occurred with the continuous growth of the Saudi population and the changing epidemiological distribution of risk factors. In addition, advancements of critical care management and endoscopic/surgical interventions might have played a role in changing the disease outcome and mortality. This research is a cross-sectional, epidemiological study carried out in a single, high-volume, tertiary care center in Riyadh to compare the current trends of AP with the patterns reported in the past Saudi and international studies in terms of annual admissions, etiologies, severity, mortality, and complications.
As mentioned hereinbefore, the most recent Saudi studies on AP date back to 2001 [2] and 2003 [3]. In both studies, the authors collected data from centers in two different regions of the kingdom and analyzed the hospital admissions due to AP at their respective centers over an extensive period of time (12 years). Comparing the results of those studies, there was a remarkable difference found in the number of hospitalized cases between different regions of Saudi Arabia. In Riyadh, the central region, 218 admissions due to AP took place over 12 years (18.2 hospitalizations/year) [2]. In Jizan (the southern region), however, only 62 patients were admitted for AP over the same period (5.2 admissions/year) [3]. Expectedly, the number of annual hospitalizations at our center in Riyadh was almost double the figures shown in Al-Karawi et al.’s [2] study in 2001 (107 admissions to our center in 3 years; 35.7/year). This could be due to the change in the diagnostic criteria used to label patients with AP [21], easier access to health care services and more liberal laboratory testing [9], or, an actual increase in the incidence due to the rising prevalence of risk factors (obesity, gallstones, hypertriglyceridemia, etc.) [9].
Similar to the findings of Al-Karawi et al. and Singal et al.’s studies, biliary pancreatitis remained the most common etiology of AP found among our patients. In contrast, alcoholic pancreatitis went from leading to a few to no admissions in 12 years to being the second most common cause of AP in our study. Mortality of AP in Saudi patients in earlier publications varied between 1.8% [3] and 4.2% [2], but increased to 7.9% despite the advances in management. However, the upper limit of mortality (4.2%) is included in our 95% CI of mortality rate. Therefore, this difference in the death rate is still likely to have occurred by chance.
With regard to international studies, recent publications presented conflicting results on the incidence of AP in the United States [7]. Some studies reported a falling incidence rate such as Sellers et al., whereas another study that included data from a more diverse database reported a 13.2% increase in AP-related hospitalizations. The authors explained this increase by the same reasons we mentioned hereinbefore. Non-U.S. studies, particularly European ones, also showed similar increases in the incidence over time [22]. Gallstone pancreatitis seems to universally have the most significant contribution to the rise in the number of cases [9,11,22,23]. However, alcohol appears to be the cause that remained steady over time across different countries. In other words, most U.S., U.K., and other European studies report that alcohol consumption has remained the same or even decreased [9,11]. Accordingly, one should expect that the incidence of alcohol-related AP cases has also declined or remained unchanged. The only study that reported epidemiological features of AP that were very similar to the ones we found in our sample of Saudi patients was by Zheng et al. [24] in Beijing.
One of the main differences between our study and the international literature was the overall higher mortality. Most reviews from the all over the world report a mortality rate of AP of 1–2% [1,9,23], and many of them also suggest that a decrease in case fatality rate has occurred over time [9,11]. One major reason for that difference could be the selection bias in our study. Although one measure to avoid biased sampling was adopted in our methodology (consecutive sample), one should keep in mind that single-center case series, particularly those from tertiary care or referral centers, always have a higher risk of including sicker patients and more complicated cases, thus ending up not being representative of the population [25]. However, population-based studies, such as most of those we cited in this discussion, use large databases either from administrative sources or national or regional hospital discharge registries, which are not yet available in Saudi Arabia.
Another limitation of this study is that, although we tried to test as many associations in our data as possible, the variables collected were not enough to provide a complete risk factor profile in our sample. Also, some of the associations drawn from our data run the risk of potential confounding. For example, the significantly higher number of alcoholic pancreatitis in males could be affected by considering the social confounders that limit the females’ access to alcoholic drinks. Data from better-designed, more extensive case-control or cohort studies are needed to draw better causal inferences on these variables.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHOR CONTRIBUTIONS
A.A.L. and A.W. contributed in study conception and design. A.A.M., S.A., T.A., K.A.S., A.A.K., A.A. and A.A.G. contributed in project administration and data acquisition. A.Q. contributed in funding acquisition. A.A.B. contributed in data curation, analysis, and manuscript writing.
FUNDING
The authors of this research article would like to acknowledge the grant provided by the Research Center at King Fahad Medical City, which funded the costs of retrieving and reviewing the medical records for this study.
Footnotes
p-value was adjusted using the Bonferroni method to test 12 post-hoc hypotheses.
Bonferroni-adjusted alpha level was 0.i025.
REFERENCES
Cite this article
TY - JOUR AU - Abed Al Lehibi AU - Mohammad Abdullah Wani AU - Abdullah Al Mtawa AU - Shameem Ahmad AU - Tauseef Azhar AU - Khalid Al Sayari AU - Abdullah Al Khathlan AU - Ahmad Al Eid AU - Adel Qutub AU - Ahmad Al Ghamdi AU - Areej Al Balkhi PY - 2019 DA - 2019/06/01 TI - Acute Pancreatitis: An Exploratory, Cross-sectional, Single-center Study of the Epidemiological Features of the Disease in a Sample of Saudi Patients JO - Journal of Epidemiology and Global Health SP - 158 EP - 162 VL - 9 IS - 3 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.190524.001 DO - 10.2991/jegh.k.190524.001 ID - AlLehibi2019 ER -
