COVID-19 in the Shadows of MERS-CoV in the Kingdom of Saudi Arabia
Additional information: MB, mbarry@ksu.edu.sa; MAA, malamari70@kfshrc.edu.sa
- DOI
- 10.2991/jegh.k.200218.003How to use a DOI?
- Keywords
- SARS-CoV-2; MERS-CoV; COVID-19; Saudi Arabia
- Abstract
Middle East Respiratory Syndrome Coronavirus (MERS-CoV) has plagued the Middle East since it was first reported in 2012. Recently, at the end of December 2019, a cluster of pneumonia cases were reported from Wuhan city, Hubei Province, China, linked to a wet seafood market with a new coronavirus identified as the etiologic agent currently named SARS-CoV-2. Most cases are in Mainland China with international spread to 25 countries. The novelty of the virus, the rapid national and international spread, and the lack of therapeutic and preventative strategies have led the WHO International Health Regulation emergency committee to declare the disease as Public Health Emergency of International Concern (PHEIC) on January 30, 2020. As it relates to countries with the ongoing MERS-CoV community cases and hospital acquired infections, there will be a huge challenge for HCWs to deal with both coronaviruses, especially with the lack of standardized and approved point of care testing. This challenge will now be faced by the whole global health community dealing with COVID-19 since both coronaviruses have similar presentation. Those patients should now be tested for both MERS-CoV and SARS-CoV-2 simultaneously, and with the continuing wide international spread of SARS-CoV-2, the travel history to China in the last 14 days will be of less significance
- Copyright
- © 2020 The Authors. Published by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Middle East Respiratory Syndrome Coronavirus (MERS-CoV) has plagued the Middle East since it was first reported in 2012 [1]. As of January 2020, the World Health Organization (WHO) has been notified of 2494 laboratory-confirmed cases with 858 mortalities [2], with the majority of cases reported from the Kingdom of Saudi Arabia (KSA), which—at the time of this writing—has a total of 2131 laboratory-confirmed cases with 827 deaths [3], making the case fatality rate (CFR) 39%. Currently, KSA continues to report MERS-CoV cases on weekly basis, but the overall number of nosocomial transmissions has significantly been reduced [4–7]. Recently, at the end of December 2019, a cluster of pneumonia cases were reported from Wuhan city, Hubei Province, China, linked to a wet seafood market with a new coronavirus identified as the etiologic agent currently named Severe Acute Respiratory Syndrome (SARS-CoV-2) [8,9]. To date, the virus has rapidly spread causing—at the time of this writing—a total of 50,272 laboratory-confirmed cases and 16,522 clinical cases (total cases 66,794) with 1524 deaths (CFR 3%). Most cases are in Mainland China (66,576), with 25 other countries affected [10] (Figure 1, adapted from WHO) including eight cases in the United Arab Emirates. The novelty of the virus, the rapid national and international spread, and the lack of therapeutic and preventative strategies have led the WHO International Health Regulation (IHR) emergency committee to declare the disease as Public Health Emergency of International Concern (PHEIC) on January 30, 2020. According to the latest China Corona Virus Disease (CDC) update, COVID-19 suspected case definition needs to fulfill an epidemiological criterion and at least two of the clinical criteria, and in the absence of an epidemiological link, fulfill all clinical criteria. Confirmed case is a suspected case with a laboratory confirmation. Epidemiological and clinical criteria are highlighted in Table 1.
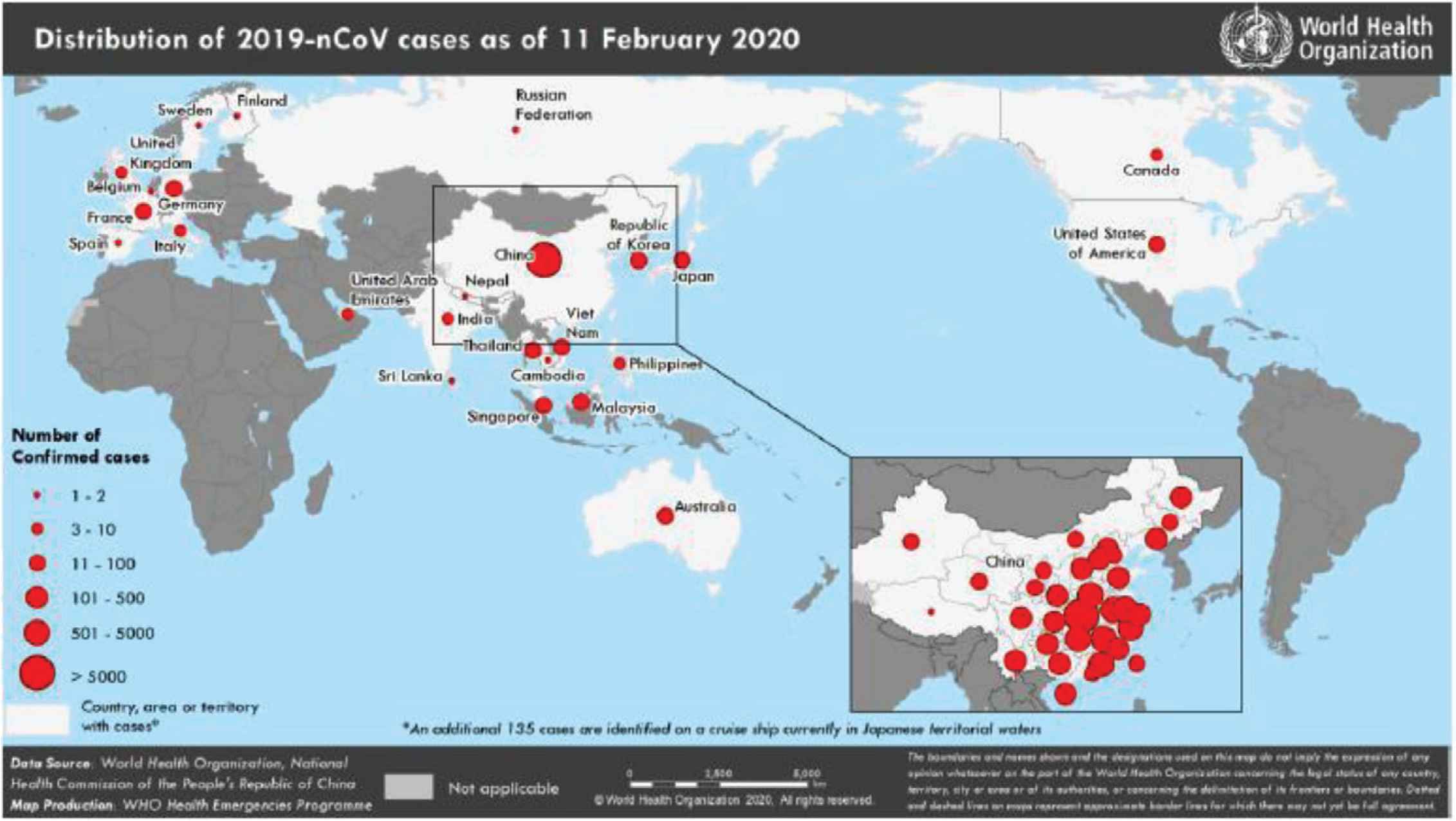
Countries, territories, or areas with reported confirmed cases of 2019-nCoV, February 11, 2020
| Epidemiological link to confirmed case or a part of symptomatic cluster and any two of |
|---|
Clinical criteria
|
Chinese CDC epidemiological and clinical criteria definitions
The Global Surveillance Interim guidance by WHO developed [11] the following case definition for suspect case: a patient fulfilling either criteria A or B as detailed in Table 2.
|
WHO suspected case definition for COVID-19
In contrast, the Saudi Center for Disease Prevention and Control (SCDC) defined a suspected case as the following [12]:
A person with acute respiratory illness (ARI) (fever with cough and/or shortness of breath) AND any of the following:
- 1.
A history of travel to China in the 14 days prior to symptom onset.
- 2.
A close physical contact in the past 14 days with a confirmed case of COVID-19 infection.
As it relates to KSA and with the ongoing MERS-CoV community cases and hospital acquired infections, there will be a huge challenge for health care workers (HCWs) to combat both viruses, MERS-CoV and SARS-CoV-2. The current MERS-CoV case definition by Saudi CDC is highlighted in Table 3.
Clinical criteria
|
Epidemiological link any of the following:
|
In adults and does not need an epidemiological criterion.
In adult and children and both need an epidemiological link within 14 days before symptoms onset.
ARDS, Acute Repiratory Distress Syndrome.
MERS-CoV case definition for suspected case as per the command and control center
After 7 years of MERS-CoV circulation in KSA, intensive efforts by the Saudi Ministry of Health (MoH) have led to drastic improvement in infection control practices in Health-Care Facilities (HCFs) kingdom wide and most health-care workforce having a very high index of suspicion for any suspected MERS-CoV cases, especially at HCF’s emergency rooms and hemodialysis units across the kingdom.
But with the lack of standardized and approved point of care testing for MERS-CoV, HCWs continue to be challenged with rapidly detecting and properly isolating patients with MERS-CoV, especially among patients with congestive heart failure (CHF) and chronic kidney disease (CKD) who present with unexplained deterioration of their chronic conditions. This challenge will now be faced by the whole global health community dealing with COVID-19 since the disease tends to be more prevalent and more severe in patients with CHF or CKD. Those patients can present with broad range of signs and symptoms and should now be tested for both MERS-CoV and SARS-CoV-2 simultaneously, and with the already wide international spread of SARS-CoV-2, the travel history to China in the last 14 days should be ignored.
The new COVID-19 guidance document [12] produced by Saudi CDC provides HCFs with a new visual triage (VT) for ARI that has a checklist for placing patients in isolation precautions with score ≥6, with the weight of the points to history of travel to China in the last 14 days prior to symptoms onset, which is given five points. This contrasts with the MERS-CoV MoH guiding document [13] in which VT for ARI requires a score of ≥4 to place patients in isolation. None of these VT scores have been validated to show effectiveness.
With the ongoing MERS-CoV circulation in animal reservoir (dromedary camels) in the Arabian Peninsula and the continuing zoonotic spillover with 70% of cases resulting from nosocomial transmission [14], the risk of emergence of COVID-19 within the same community would be overwhelming to the health-care infrastructure of the countries affected by MERS-CoV. This is a true concern with the already rapid international spread to 25 countries outside China, especially with the ability of SARS-CoV-2 to spread from a totally asymptomatic person [15].
Since the declaration of PHEIC by WHO on January 31, 2020 [16], 16 cities in mainland China with a population of around 60 million people remain under quarantine [17]. Many countries including Japan, the United States, France, Australia, Sri Lanka, Germany, Saudi Arabia, Russia, and Thailand among others evacuated their citizens through chartered flights [18], and several countries have recommended travelers to avoid nonessential travel to China and cancelled scheduled flight in and out of China [19]. Many countries [12] enforced public health measures at ports of entry with trained staff, appropriate space, and equipment and supplies for managing potential ill travelers, implementing entry screening including temperature recording for travelers arriving from China (directly or indirectly), and mandatory declaration of recent travel to china to immigration and passport officers. Although these measures may prevent the entry of active COVID-19 cases, history taught us that this system is not fully effective in preventing virus introduction into a country.
As per Saudi CDC, other public health measures include obligatory reporting of HCFs by calling a specific number and through the Health Electronic Surveillance Network. This would activate a rapid response team tasked with completing epidemiological investigation in HCFs and community spontaneously, categorizing household and community contacts as per their symptoms, which, as with MERS-CoV, underplays the need for more liberal testing or isolating asymptomatic contacts [20].
A comparative analysis of factors influencing MERS-CoV outbreak in KSA compared to South Korea identified several exacerbating factors: which includes poor access to health-care professionals at general practitioner level, which can result in delays between disease development, progression, and diagnosis, individuals who relied on camels for daily living denied the relation between camels and MERS-CoV: kicking off the “Kiss Your Camel campaign,” which became increasingly popular in Social Media in 2015, and 75% of HCWs were unaware of how disease spreads, with a general feeling of workers and citizens is largely that MERS was not a substantial problem [21]. Similarly, the current COVID-19 outbreak and response have been accompanied by a massive “infodemic”—an overabundance of information—some accurate and many not—that makes it hard for people to find trustworthy sources and reliable guidance [10], as most turn to social media, it is vital to track and respond to myths and rumors, an up-to-date reference should be maintained.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
The authors contributed equally to the article.
REFERENCES
Cite this article
TY - JOUR AU - Mazin Barry AU - Maha Al Amri AU - Ziad A. Memish PY - 2020 DA - 2020/02/21 TI - COVID-19 in the Shadows of MERS-CoV in the Kingdom of Saudi Arabia JO - Journal of Epidemiology and Global Health SP - 1 EP - 3 VL - 10 IS - 1 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.200218.003 DO - 10.2991/jegh.k.200218.003 ID - Barry2020 ER -
