Little Old Ladies’ Eye
- DOI
- 10.2991/artres.k.191105.001How to use a DOI?
- Keywords
- Masked aortic hypertension; visual-field defect; blind spots
- Copyright
- © 2019 Association for Research into Arterial Structure and Physiology. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
We recently encountered an older patient with severe hypertensive retinopathy on her right eye who had been normotensive all her life as documented not only by serial office blood pressure measurements but also with ambulatory blood pressure monitoring. Unappreciated hypertension, is said to be masked from view and therefore, unappreciated and untreated. Masked hypertension is currently defined as existent hypertension even though office indirect brachial artery measurements with syphygmomanometry are normal. The condition can be detected by 24-h Ambulatory Blood Pressure Monitoring (ABPM) or with home blood pressure measurements. However, our concern here is not the blood pressure at the brachial artery. The hand is seldom the site of target-organ damage. Our issue is what happens centrally. Can the central aortic hypertension be masked when only brachial artery measurements are considered? This is obviously the case with our patient.
Augmentation designates the added systolic pressure contributed by the reflected pulse wave in stiff arteries with increasing age. As a result, the central aortic pressure progressively increases and is subsequently higher than the peripheral pressure at the brachial artery. The stiffer the vessels and the shorter the aorta as in short patients, the faster the pulse-wave velocity and the reflected pulse-wave, and the greater is the augmentation effect on systolic central aortic blood pressure.
2. THE CASE
A 78 year-old woman (159 cm, BMI 23 kg/m2) had previously enjoyed life-long good health. Her office blood pressure measurements had invariably been normal. She had never required antihypertensive medication. ABPM had recently been performed that revealed a day time mean blood pressure of 137/75 mmHg and night time mean of 129/69 mmHg. Echocardiography had even been performed that showed normal dimensions of the left ventricle with some evidence of diastolic dysfunction.
The patient consulted an ophthalmologist because of difficulties in reading small texts. Her ophthalmologist detected changes in her retinal vessels funduscopically that were consistent with hypertension, an unexplained right-sided visual-field defect, and early cataract formation in the left eye. He referred her to special ophthalmological circulatory laboratory for a more detailed evaluation. Objective findings were a visual acuity of 20/20 right eye and 10/20 left eye. The intraocular pressure was estimated at 21 mmHg in both eyes. The visual field map of right eye revealed an enlarged blind spot and arcuate scotomas within 30° (Figure 1A and 1B). The left eye showed only slight diffuse defects presumably due to early cataract formation. Retinoscopy revealed bilateral diffuse narrowing of the retinal arterioles (Figure 2A and 2B). In the right eye, changes suggested possible residual cotton-wool spots within the large vascular arcade. The optic disks were flat and showed no evidence of papilledema. Haemorrhages were not observed.
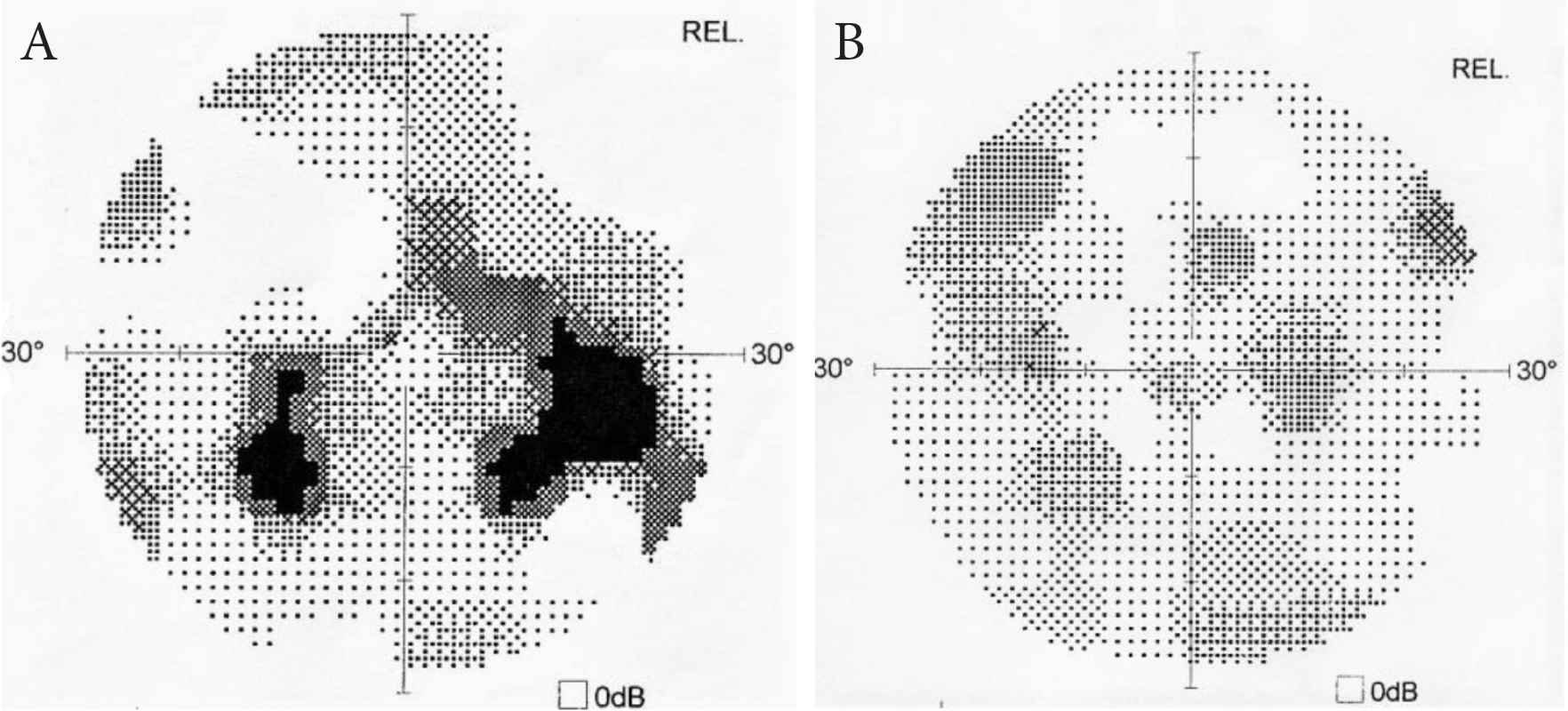
(A) and (B) Visual fields of right and left eye before therapy of aortic hypertension.
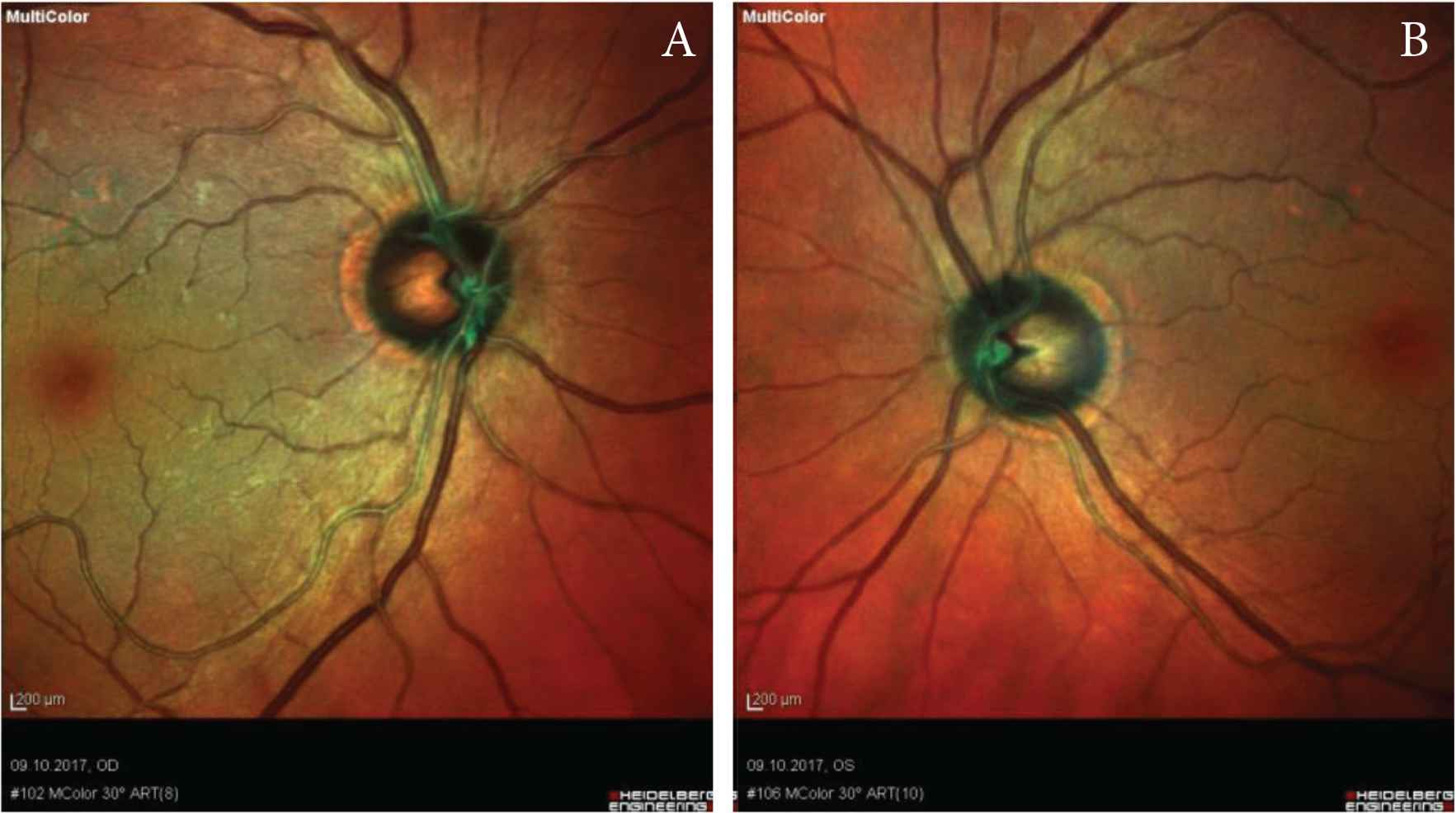
(A) and (B) Multicolor-image (Heidelberg Instruments Optical Coherence Tomography) of right and left eye posterior pole.
Intravenous fluorescein angiography with digital measurements of systemic and retinal perfusion times was then performed in both eyes (Heidelberg Retina Angiograph). Videoangiography showed patchy filling of choroid in the right eye, which was not seen in left eye. The patient’s blood pressure was monitored during angiography at 140/65 mmHg and her heart rate ranged between 84 and 88 beats/min. A relatively short injection-to retina time was observed, which could be attributed to her heart rate (Table 1). The injection-to-retina time in the right eye was longer than in the left, perhaps consistent with the funduscopic differences.
| Normal | Right eye before and after therapy | Left eye before and after therapy | |||||
|---|---|---|---|---|---|---|---|
| Right eye before | Right eye after | Difference (%) | Left eye before | Left eye after | Difference (%) | ||
| IRT | 7–15 s | 8.0 s | 9.5 s | +12.5 | 9.6 | 11.2 | +16.6 |
| RPT | 6–10 s | 8.0 s | 8.3 s | +4 | 6.9 | 6.8 | −1.4 |
| RPT–IRT-ratio | 0.8–1.2 | 1.5 | 1.3 | −13 | 1.08 | 0.91 | −16 |
IRT, time difference between intravenous injection of fluorescein-bolus and first appearance of dye in the central retinal arteries reflecting the velocity of systemic circulation (brachial vein, heart, lung, carotid artery) mainly depending on heart rate; RPT, time difference between first appearance of dye within retinal arteries and complete filling of retinal venous vessels reflecting the capillary transit time of the fluorescein-bolus is regulated by retinal autoregulation; RPT–IRT-ratio, relation between systemic and retinal blood flow velocity.
Injection-retina-time (IRT), retinal-perfusion-time (RPT) and ratio of IRT/RPT before and after therapy of aortic hypertension
The patient was next referred to the Munich Hypertension Center for further cardiovascular analysis. The brachial blood pressure was 136/85 mmHg at the right arm and 137/82 mmHg at the left arm. Nonetheless, the pulse-wave analysis was abnormal (Figure 3) showing an elevated central aortic blood pressure at the right arm with a systolic pressure 142.8 mmHg (normal for age <120 mmHg) [1] and an aortic augmentation index of 51.7% (normal for age <40%). The pulse-wave velocity was 11.8 m/s (normal for age <11 m/s). We subsequently initiated antihypertensive medication with 5 mg amlodipine in the morning. Two months later, the pulse-wave analysis showed a brachial blood pressure of 135/83 mmHg, systolic central aortic blood pressure 127.4 mmHg, aortic augmentation index 22.0% and pulse-wave velocity 8.8 m/s (Figure 4).
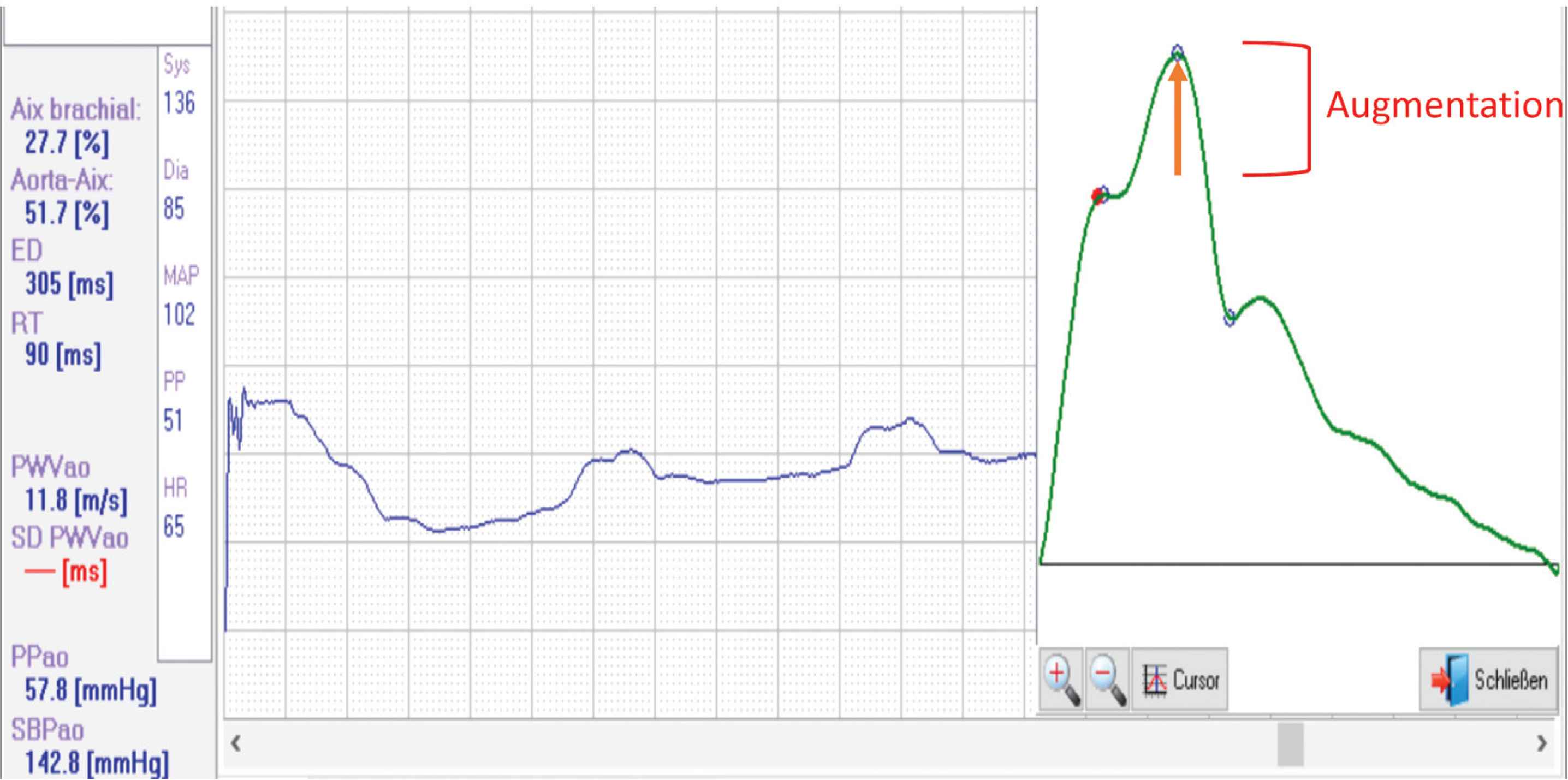
Original graph of arterial pulse wave measured with Arteriograph (Tensiomed, Budapest, Hungary) [3] before antihypertensive medication. Augmentation designates the added systolic pressure by the reflected pulse wave.

Pulse-wave analysis under antihypertensive medication after 2 months. Systolic augmentation is supressed and Augmentation Index reduced from 51 to 22%.
We repeated the ophthalmologic angiographic measurements after the masked central aortic hypertension was treated. The injection-to-retina time was increased by 12.5% in the right eye and by 16.6% in the left eye. Interestingly, the retinal perfusion time remained nearly the same in both eyes showing that the medical influence on systemic circulation did not have a negative effect on retinal circulation. The ratio between systemic and retinal circulation velocity, which was raised in right eye prior to therapy returned to near normal values with treatment (Table 1). Furthermore, the visual field defects that were present at the first evaluation were no longer detectable after treatment of the masked central aortic hypertension (Figure 5A and 5B).
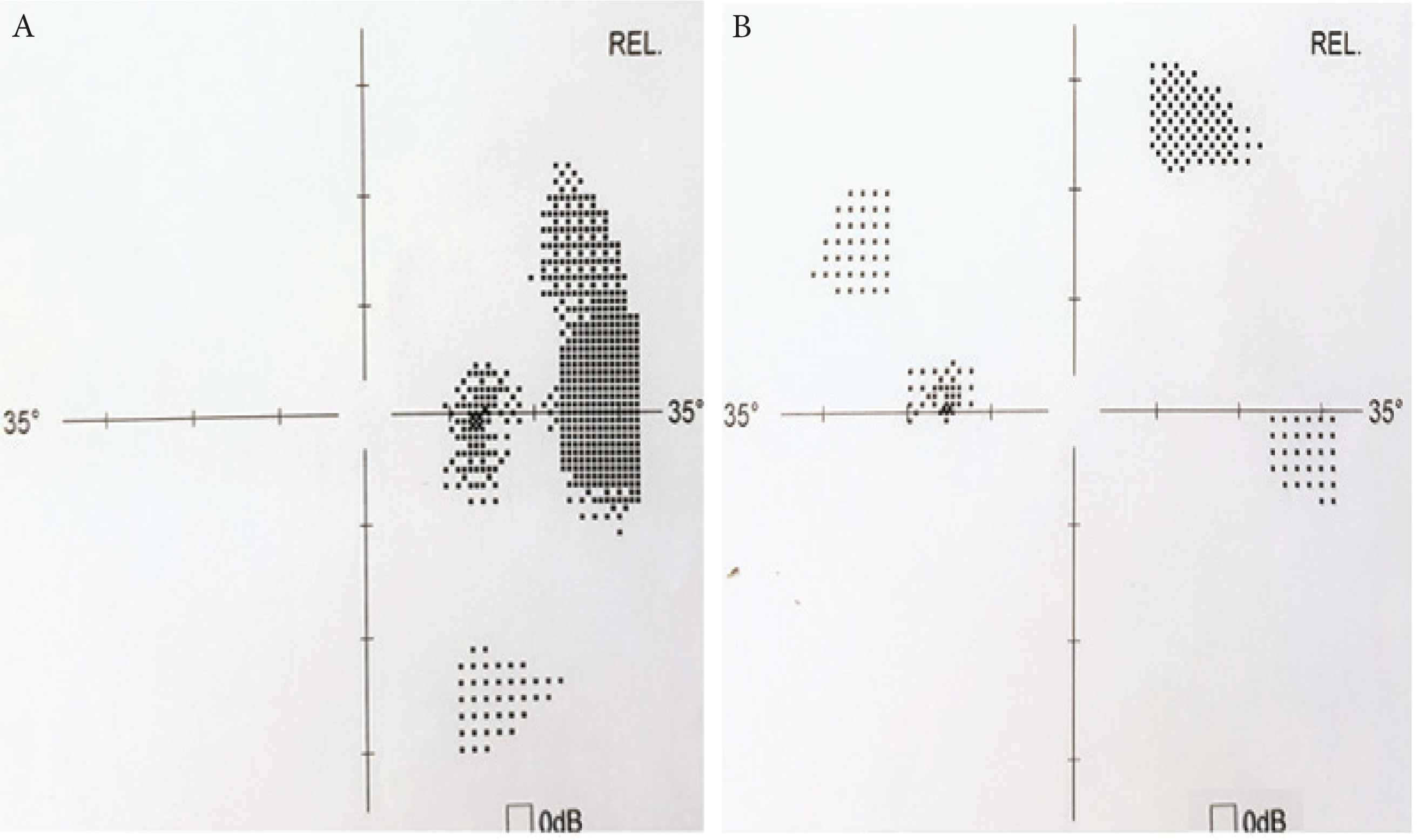
(A) and (B) Visual fields of right and left eye after therapy of aortic hypertension.
3. DISCUSSION
Our patient developed severe hypertensive retinopathy on her right eye without hypertension as defined by conventional blood pressure measurement on the upper arm including ambulatory blood pressure monitoring over 24 h. However, pulse wave analysis revealed an elevated central aortic blood pressure. Measuring blood pressure only at the brachial artery is no longer adequate in estimating cardiovascular health. Especially when hypertensive organ damage is present and brachial blood pressure is normal we need to assess central blood pressure. This important parameter remains masked when blood pressure is measured only at the brachial artery. However, available technology can unmask the situation and provides us with improved risk assessment. With aging and vascular risk factors, central vessels stiffened and the augmentation of systolic blood pressure becomes progressively greater. Pulse wave analysis is essential here. Simple noninvasive techniques are available for recording a high-fidelity waveform from an accessible pulse, permitting the estimate of an aortic or central waveform by application of a generalized transfer function. Determining pulse-wave velocity in meter per second is an important parameter of vascular elasticity and a predictor of cardiovascular health [2]. An increase in reflected pulse wave due to increased velocity leads to a continuously increased systolic blood pressure augmentation. Augmentation designates the added systolic pressure contributed by the reflected pulse wave. As a result, the central aortic pressure progressively increases and is subsequently higher than the peripheral pressure at the brachial artery. The stiffer the vessels and the shorter the aorta as in short patients like little old ladies, the faster the pulse-wave velocity, and the greater is the augmentation effect on systolic central aortic blood pressure due to a faster and higher retrograde reflected wave.
The heart, kidneys, brain, and eye are more subject to central pressures, compared with peripheral pressures. With increased vascular stiffness, the laminar flow component becomes progressively less and the pulsatile component increases. This pulsatile stress becomes progressively greater with advancing age. Particularly the afore-mentioned target organs are adversely affected and subjected to damage [4–7]. Little old ladies’ heart is described as diastolic heart failure as a consequence of increased arterial stiffness, augmentation of central aortic pressure and increasing left ventricular tension and load [8]. Interestingly, in our patient the eye was the most important target organ. She had an increase in blind spots, detectable by visual field determinations. Moreover, her funduscopic picture was less healthy than her brachial artery blood pressure determinations or even ABPM results. Treating and decreasing central aortic blood pressure resolved the visual problem in our patient.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHOR CONTRIBUTIONS
MM and JN had full access to all of the data and take responsibility for the integrity of the data and the accuracy of the data analysis and interpretation. FCL contributed in Critical revision of the manuscript for important intellectual content.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Martin Middeke AU - Joachim Nasemann AU - Friedrich Cameron Luft PY - 2019 DA - 2019/11/18 TI - Little Old Ladies’ Eye JO - Artery Research SP - 77 EP - 80 VL - 25 IS - 1-2 SN - 1876-4401 UR - https://doi.org/10.2991/artres.k.191105.001 DO - 10.2991/artres.k.191105.001 ID - Middeke2019 ER -
