Arterial Stiffness, Central Blood Pressure, and Cardiac Biomarkers in Long-Distance Walkers
- DOI
- 10.2991/artres.k.191106.002How to use a DOI?
- Keywords
- Walking; vascular stiffness; cardiovascular physiological phenomena; arterial pressure
- Abstract
The cardiovascular effects of long-distance and -duration activities and their relationship with arterial stiffness and cardiac biomarkers are still unclear. This study aimed to assess arterial stiffness and Central Blood Pressure (cBP) and correlate them with cardiac biomarkers in long-distance walkers (271 km in 4 days). This longitudinal study assessed Peripheral Systolic Blood Pressure (pSBP), Peripheral Diastolic Blood Pressure (pDBP), Central Systolic Blood Pressure (cSBP), Central Diastolic Blood Pressure (cDBP), Pulse-Wave Velocity (PWV), Central Pulse Pressure (cPP), Augmentation Index (AIx), and total vascular resistance, using the Mobil-O-Graph® device and biomarkers creatine kinase-MB, troponin T, and brain natriuretic peptide. All items were assessed 30 days before the event (A0) and at the end of the 1st (A1), 2nd (A2), 3rd (A3), and 4th (A4) days of walk. Data were analyzed using Stata Software and p-values < 0.05 were considered significant. This study included 25 men, with mean age of 46 ± 10.5 years and body mass index of 20.2 ± 2.3 kg/m2. pSBP level reduced from A0 (122.8 ± 2.2) to A1 (111.6 ± 2.1) (p = 0.004) and cSBP level reduced from A0 (110.2 ± 2.2) to A1 (101 ± 1.8) (p = 0.035). CK-MB enzyme correlated with PVR in both A1 (r = 0.445, p < 0.033) and A4 (r = 0.554, p < 0.006). Troponin T showed correlation at A4 with cSBP (r = 0.468, p < 0.024) and pSBP (r = 0.470, p < 0.023). There was no change in PWV. This study showed that this exercise modality did not cause harmful alterations related to arterial stiffness behavior.
- Copyright
- © 2019 Association for Research into Arterial Structure and Physiology. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
There have been an increasing number of people practicing long-distance and -duration exercises worldwide. However, the effects of this exercise type on cardiovascular health, especially acute and subacute effects, are still controversial [1]. The relationship between vascular damage, early aging, and cardiovascular risk factors and the damages and benefits of physical effort can explain important associations to optimize preventive measures and approaches [2,3].
Arterial stiffness measurements are health markers and predictors of cardiovascular outcomes [2,4]. An alternative to practically assess arterial stiffness is the measurement of Central Blood Pressure (cBP), which is a better predictor of cardiovascular outcomes than the Peripheral Blood Pressure (pBP) [4]. Cardiac biomarkers are also important elements to assess and monitor individuals who have undergone prolonged exercise [1,5].
Physical exercise acts by decreasing Pulse-Wave Velocity (PWV) and chronically reducing Central Pulse Pressure (cPP) and other parameters of arterial stiffness [6]. In prolonged races, arterial stiffness decreases in the post-effort phase and returns to baseline levels [7]. Aortic compliance and distensibility increase in active practitioners of this exercise modality [8].
As for biomarkers, prolonged running significantly increases Creatine Kinase-MB (CK-MB) enzyme, cardiac troponin, and Natriuretic Peptide Type B (BNP) [1,5]. Elevated CK levels were reported in recreational runners [9]. Increased serum levels of these biomarkers in the general population are a predictor of increased risk of cardiac events. However, the significance of this increase in athletes is hardly known [10]. Some studies also suggest a correlation between arterial stiffness and BNP [11,12].
Correlations between variables of arterial stiffness and cardiac biomarkers in long-distance and -duration walking have not been established yet. This analysis may help to understand the cardiovascular risk assessment of long-term and moderate-intensity exercise. This analysis may improve the invasive understanding of cardiovascular risk in this exercise modality [13].
In healthy people, whether changes after this model of physical activity are a consequence of physiological adaptations or a result of damages caused by prolonged exposure to effort is still unclear. This understanding is important to better evaluate the risks and benefits of this exercise modality [1]. Thus, the objective of this study was to assess arterial stiffness and central pressure for 4 days and to correlate them with cardiac biomarkers in long-distance and -duration walkers.
2. MATERIALS AND METHODS
This longitudinal study included male participants of a 310 km walk that lasted 5 days, with a mean of 62 km/day, held in Brazil in 2015. This annual event, which is called Goiás Ecological Walk Brazil (CEG), exists for more than 25 years, being the largest of its kind in Latin America, encourage environmental preservation, ecological awareness and the practice of sports. It involves long-distance and -duration exercise of moderate to severe intensity. The intensity is variable because of speed changes in different stages of the race, alternating fast-paced walking with running. The average speed is 7.6 km/h, and there are varied inclination levels and important temperature variations throughout the day.
CEG participant selection is independent and voluntary. Registration was online and participants were adults, practicing regular exercise, without contraindications to this type of activity as attested by a physician. After registration, participants went through selective competition, in which they had to run 56 km in 2 days (28 km/day). Best time runners were selected.
The study took place in two stages. The first stage occurred 30 days before CEG, when the participants signed the informed consent form and went through an initial evaluation (A0) composed of anamnesis, BP measurement, and blood collection for evaluation of cardiac biomarkers (Figure 1). The sociodemographic and health variables evaluated were age, family history of cardiovascular disease, medication use, Body Mass Index (BMI) obtained by dividing weight by square of height, smoking, aerobic physical activity, exercise type and duration, orthopedic problems, and other events in the running competitions and in other CEG editions. BP and vascular stiffness variables were Peripheral Systolic Blood Pressure (pSBP), Peripheral Diastolic Blood Pressure (pDBP), Central Systolic Blood Pressure (cSBP), Central Diastolic Blood Pressure (cDBP), cPP, Augmentation Index (AIx) corrected for heart rate, PWV, and total vascular resistance (Total VR) obtained with the Mobil-O-Graph® device on the right upper limb.
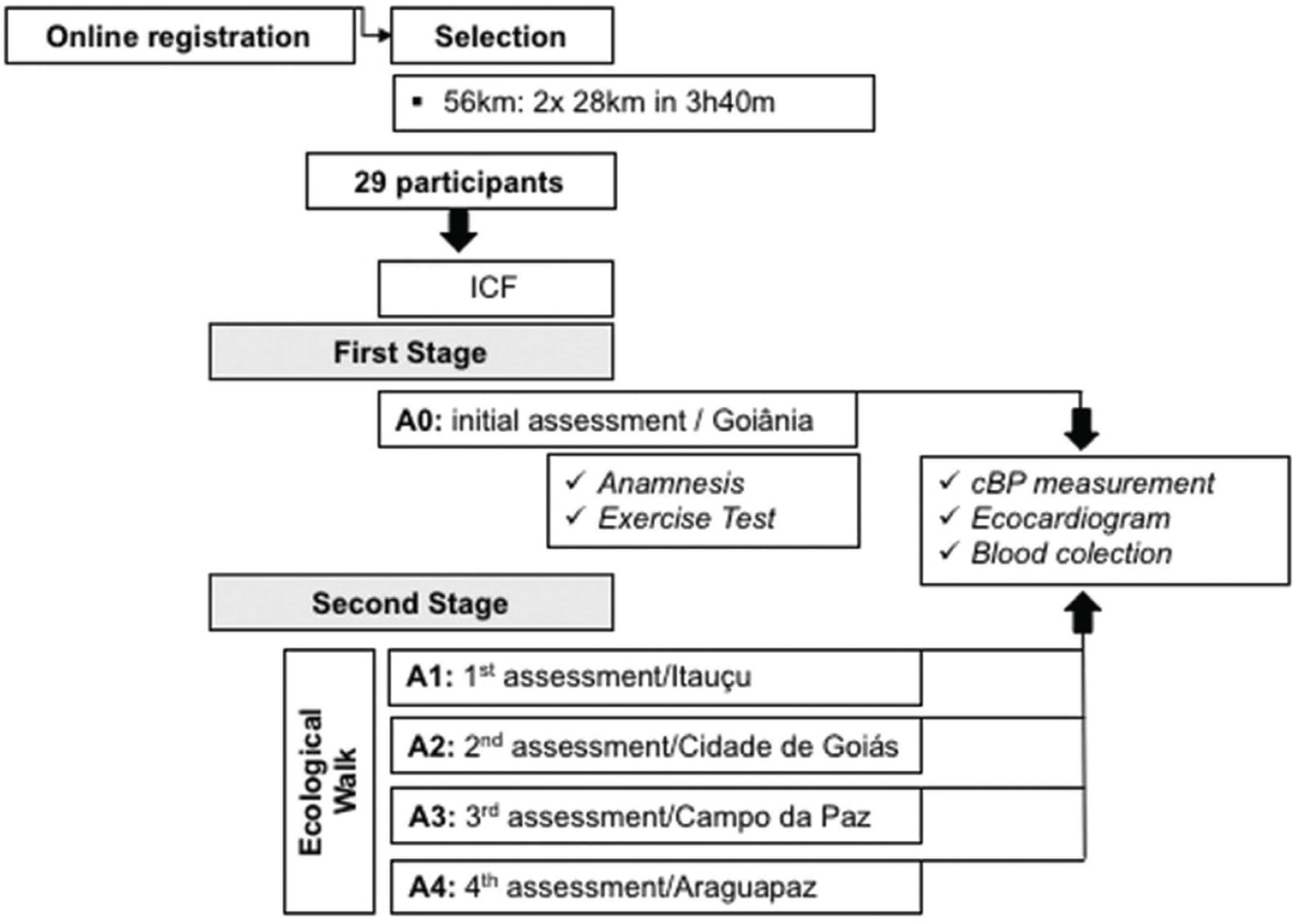
Flowchart of the study phases. A0, initial assessment; A1, first assessment; A2, second assessment; A3, third assessment; A4, fourth assessment; BP, blood pressure; ICF, informed consent form; h, hours; km, kilometers; m, minutes; cBP, central blood pressure.
The biomarkers evaluated were CK-MB enzyme, troponin T and BNP. Standardized procedures were used for the analysis [14].
The second stage included four assessments, one on each CEG day: assessment at days 1 (A1), 2 (A2), 3 (A3), and 4 (A4). Participants were assessed 30–120 min after the end of the walk, when they arrived in the lodgings (early evening) in the city where they would sleep. In all assessments, the central pressure was measured and venous blood was collected (Figure 1). There was no assessment at day 5.
2.1. Statistical Analysis
Data were independently typed in duplicate, and inconsistencies were corrected. Qualitative variables were presented with frequencies and proportions and quantitative variables with mean, standard deviation, and 95% confidence interval. The Shapiro–Wilk test was used to verify data distribution of quantitative variables, and the Pearson or Spearman tests for the correlations. The analysis of variance (ANOVA) for repeated measurements with Bonferroni’s post hoc was used to compare variables among the days. Significance level was p < 0.05.
The study was approved by the Human Research Ethics Committee of the Pontifical Catholic University of Goiás (proposal 1.107.021).
3. RESULTS
Twenty-five men with a mean age of 46 ± 10.5 years and BMI 20.2 ± 2.3 kg/m2 were assessed. The distance covered in 4 days was 271 km, and the average walk distance was 67.7 km/day. Night rest period during the walk lasted 6–7 h.
Among the participants, 24% (six) had a family history of cardiovascular disease and 16% (four) used medications such as antihistamine, polyvitamin, levothyroxine sodium, and biguanide. No participants were smokers at the time of assessment, and 20% (five) reported being ex-smokers (Table 1).
| Variables | n (%) |
|---|---|
| Age group (years) | |
| 19–39 | 5 (20) |
| 40–59 | 19 (76) |
| ≥60 | 1 (4) |
| Family history of cardiovascular disease | |
| Systemic arterial hypertension | 5 (20) |
| Valvopathy | 1 (4) |
| Personal history of cardiometabolic diseases | |
| Diabetes mellitus | 1 (4) |
| Hypothyroidism | 1 (4) |
| Medication use | |
| No | 21 (84) |
| Yes | 4 (16) |
| Type of aerobic exercise | |
| Running | 24 (96) |
| Walking | 17 (68) |
| Others | 13 (52) |
| Anaerobic exercise (body building) | |
| No | 21 (84) |
| Yes | 4 (16) |
| Other participations in running events (km) | |
| 5 | 6 (24) |
| 10 | 17 (68) |
| 21.097 (half marathon) | 12 (48) |
| 42.195 (marathon) | 4 (16) |
| Participation in editions of the Goiás Ecological Walk | |
| First | 6 (24) |
| 1–5 | 9 (36) |
| ≥6 | 10 (40) |
Socio-demographic, health characteristics and physical exercise practice of the participants of the Goiás Ecological Walk, Goiânia, GO, Brazil, 2015, n = 25
All participants practiced aerobic exercise with an average frequency of three times and duration of 97.9 min a week for more than 14.3 years. Of these participants, 68% (17) had already participated in running events. Orthopedic problems were reported by 12% (three) of the participants: left knee pain, plantar fasciitis, and hamstring muscle cramps. Nineteen walkers (76%) had participated in other CEG editions (Table 1).
Moreover, pSBP reduced from A0 (122.8 ± 2.2) to A1 (111.6 ± 2.1) (p = 0.004) and cSBP reduced from A0 (110.2 ± 2.2) to A1 (101 ± 1.8) (p = 0.035) (Table 2). CK-MB enzyme correlated with TVR at A1 (r = 0.445, p < 0.033) and at A4 (r = 0.554, p < 0.006). Troponin T correlated with cSBP (r = 0.468, p < 0.024) and pSBP (r = 0.470, p < 0.023) at A4. No correlations were observed between other blood pressure and arterial stiffness parameters with cardiac biomarkers (Figure 2).
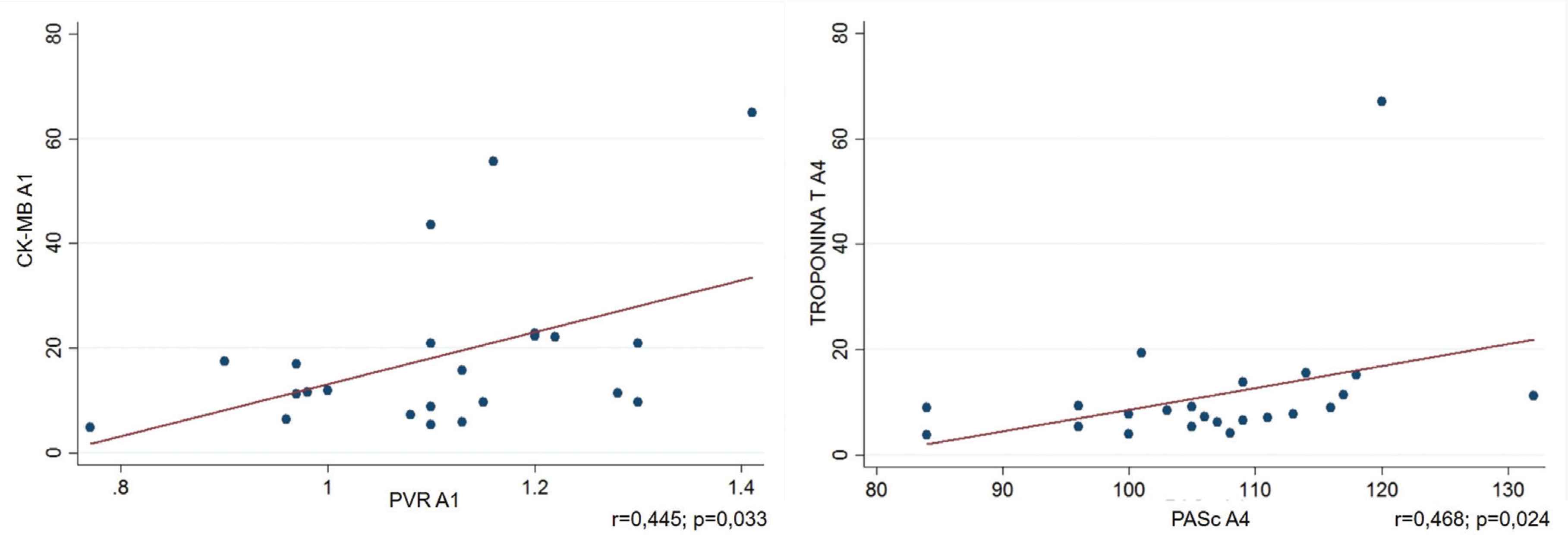
Correlation between blood pressure parameters and arterial stiffness with the cardiac biomarkers of participants from the Goiás Ecological Walk, Goiânia, GO, Brazil, 2015, n = 25. A1, first assessment; A4, fourth assessment; cSBP, central systolic blood pressure; pSBP, peripheral systolic blood pressure; PVR, peripheral vascular resistance.
| Parameters | Mean ± SD | 95% CI | F | Post hoc | Parameters | Mean ± SD | 95% CI | F |
|---|---|---|---|---|---|---|---|---|
| p | p | |||||||
| pSBP | pDBP | |||||||
| A0 | 122.7 ± 2.21 | 118.29–127.45 | 3.99 | A0–A1* | A0 | 76.75 ± 1.88 | 72.84–80.65 | 1.64 |
| A1 | 111.60 ± 2.16 | 107.13–116.06 | 0.004 | A1 | 71.48 ± 1.97 | 67.39–75.56 | 0.17 | |
| A2 | 114.44 ± 1.91 | 110.48–118.39 | A2 | 73.04 ± 1.68 | 69.55–76.52 | |||
| A3 | 114.79 ± 1.89 | 110.88–118.70 | A3 | 72.45 ± 1.49 | 69.36–75.54 | |||
| A4 | 114.90 ± 2.33 | 110.08–119.74 | A4 | 71.08 ± 1.63 | 67.69–74.47 | |||
| cSBP | cDBP | |||||||
| A0 | 110.25 ± 2.21 | 105.67–114.82 | 2.68 | A0–A1* | A0 | 78.16 ± 1.80 | 74.42–81.90 | 1.73 |
| A1 | 101.00 ± 1.87 | 97.12–104.87 | 0.035 | A1 | 72.8 ± 1.96 | 68.73–76.86 | 0.15 | |
| A2 | 106.04 ± 1.84 | 102.21–109.86 | A2 | 74.29 ± 1.73 | 70.70–77.87 | |||
| A3 | 105.70 ± 2.03 | 101.49–109.92 | A3 | 73.83 ± 1.49 | 70.73–76.93 | |||
| A4 | 106.87 ± 2.20 | 102.31–111.43 | A4 | 72.41 ± 1.61 | 69.07–75.75 | |||
| cPP | AI | |||||||
| A0 | 32.70 ± 1.31 | 29.98–35.43 | 2.04 | A0 | 12.24 ± 2.19 | 7.69–16.78 | 2.26 | |
| A1 | 32.72 ± 1.99 | 28.59–36.84 | 0.11 | A1 | 17.82 ± 1.93 | 13.83–21.80 | 0.06 | |
| A2 | 34.88 ± 1.44 | 31.90–37.85 | A2 | 19.48 ± 2.10 | 15.14–23.83 | |||
| A3 | 37.20 ± 2.00 | 33.05–41.36 | A3 | 14.56 ± 1.86 | 10.69–18.42 | |||
| A4 | 38.29 ± 1.42 | 35.34–41.23 | A4 | 13.47 ± 1.97 | 9.39–17.55 | |||
| PWV | PVR | |||||||
| A0 | 6.84 ± 2.21 | 6.36–7.32 | 0.41 | A0 | 1.11 ± 0.03 | 1.04–1.19 | 0.76 | |
| A1 | 6.54 ± 0.20 | 6.13–6.96 | 0.80 | A1 | 1.09 ± 0.02 | 1.03–1.15 | 0.55 | |
| A2 | 6.57 ± 0.19 | 6.17–6.98 | A2 | 1.10 ± 0.02 | 1.04–1.16 | |||
| A3 | 6.56 ± 0.19 | 6.15–6.97 | A3 | 1.09 ± 0.02 | 1.03–1.14 | |||
| A4 | 6.75 ± 0.21 | 6.30–7.19 | A4 | 1.04 ± 0.02 | 0.99–1.10 |
p < 0.05 (repeated measures analysis of variance and Bonferroni’s post hoc). A0, initial evaluation; A1, first evaluation; A2, second evaluation; A3, third evaluation; A4, fourth evaluation; CI, confidence interval; cDBP, central diastolic blood pressure; cSBP, central systolic blood pressure; cPP, central pulse pressure; pDBP, peripheral diastolic blood pressure; pSBP, peripheral systolic blood pressure; SD, standard deviation.
Comparison of peripheral and central blood pressure, central pulse pressure, augmentation index (AIx), pulse-wave velocity (PWV), and peripheral vascular resistance (PVR) among assessments, Goiânia, GO, Brazil, 2015, n = 25
4. DISCUSSION
The assessed volunteers showed cSBP and pSBP reduction from A0 to the end of A1 without subsequent changes. Arterial stiffness variables (PWV, AIx, and cPP), cDBP, and pDBP did not change during the race course.
The researchers did not control the activities practiced by the study participants between A0 and A1. Physical preparation in this period prior to the event was free and individualized. We believe there was an increased practice of physical exercise and optimization of eating habits in this period, which may justify the improvement observed in cSBP and pSBP levels [6].
Significant reductions in BP values were not expected along the race course since participants already had optimal BP levels on the first day [15]. This may show that despite the long-distance and -duration, there is a cardiovascular adaptability that preserves arterial compliance and cSBP and pSBP levels soon after the end of physical effort.
Results are still controversial for the acute effects of physical exercise on arterial stiffness. A study that evaluated arterial stiffness in intermediate- and long-distance runners identified that moderate or severely intense exercise causes a temporary increase in arterial stiffness, which returns to values below resting levels after 30 min. An increased inflammatory activity during this exercise modality might influence the temporary increase in arterial stiffness parameters [2]. In our study, the participants were assessed 30–120 min after exercise, which may explain why we did not identify changes related to arterial stiffness.
A study that evaluated long-distance (195 km) runners showed reduced arterial compliance. On the contrary, arterial compliance was increased at a distance of 80 km. The authors suggest that excessively long distances may be associated with increased arterial stiffness [16]. Another study evaluating PWV before and after a 30-h ultramarathon showed a significant reduction of this biomarker [17].
Arterial stiffness may also present variations throughout the exercise. The assessment of nine male marathon runners identified that PWV decreased at 45 km and then returned to baseline at 75 km, which may indicate that effort exposure time has a variable role in interfering with vascular compliance response [7].
Other publications that assessed marathoners presented results similar to ours, with no significant changes in arterial stiffness parameters during the exercise period [18,19]. A previous study on CEG also found no significant changes in PWV [20].
Other studies that examined arterial properties and cardiovascular health of long-distance runners in relation to arterial stiffness are controversial [2,7]. It is still unclear how regular and prolonged aerobic exercise acts on arterial compliance. Regular physical activity may influence artery elasticity through endothelium-dependent vasodilation [21]. In this case, it would be a more important action in the arterial intima layer, without much interference in the middle layer structure. More significant and lasting changes in these parameters would require changes in the muscular layer structure (mean), which would require a longer exposure time to exercise (chronic effects) [22,23]. PWV changes relate to arterial structure and resistance and elasticity, which are associated to the amount of collagen and elastin [4]. It means that significant changes in this parameter might also be identified only after longer periods [8]. This is the possible reason we did not identify changes in arterial compliance, since the acute effects of physical exercise were evaluated after 30–120 min of exposure to physical effort.
The collected data related to women participating in the CEG were not considered for inclusion in the analysis, since they totaled only four and the change in arterial stiffness behaves differently between the sexes. These factors could represent a bias in the analysis of the results.
As for biomarkers, this study was not supposed to verify their development during walking, but how much they are related to arterial stiffness parameters and cBP during walking. Some studies showed an association of BNP with vascular stiffness [11,12]. In our study, CK-MB enzyme had positive correlation with PVR at A1 and A4, although PVR remained stable throughout the walk. Prolonged exposure to physical effort may increase ventricular afterload and contribute to increase myocyte oxygen uptake by elevating CK-MB, which is a sensitive enzyme marker for muscle damage that is generally elevated in marathoners [24,25].
No relationship was found between BNP and other variables of arterial stiffness or cBP. This can be explained by the assessment of acute responses to the activity and by a relationship among these variables that would only happen in case of a greater exposure and during physical effort. Another consideration is that arterial stiffness involves vessel elasticity, compliance, and distensibility, while BNP production starts from volume and pressure overload. This correlation tends to be limited, as there were no changes in arterial stiffness parameters.
Troponin T protein showed positive correlation with both cSBP and pSBP at day 4. Troponin T is a specific marker of myocardial necrosis, a gold standard for this diagnosis [26]. Further, the increase of this marker is a consequence of cardiomyocyte damage, whether acute or chronic. In another study, after the marathon, BNP and troponin increased in 13 women and 12 men, suggesting that increased wall tension and dilated cardiac chambers could explain the elevation of these cardiac biomarkers when associated with intense and prolonged exercise [5]. The correlation with BP levels at the end of the race course at A4, when a great distance had already been traveled, may have been influenced by the same mechanisms that increase troponin, such as wall tension and dilated cardiac chambers.
On the contrary, a lack of consistency and regularity in the correlation analyses between arterial stiffness and inflammation in this healthy population and with this exercise model may indicate the presence of a pathophysiology in a different location.
Considering these data, the behavior of inflammation and arterial stiffness in healthy people may be different from their behavior in people with cardiovascular diseases or risk factors. Individuals with normal body weight and BMI who are regular practitioners of physical activity appear to be protected even with intense and prolonged physical effort. Clearly, this effort model, assessed by arterial stiffness parameters and biomarkers, is a safe practice in this population.
This study had some limitations. The parameters were evaluated in the pre-walk period (30 days before) and during the exercise (30–120 min after), without assessments at the beginning of each day during the CEG race course. Other characteristics of the study were different conditions and time of A0, which occurred during rest time in the morning and evening, in relation to assessment during exercise, always after the effort and at the end of the day. In addition, there was no control of the activities developed by the participants during the 1-month period between A0 and subsequent assessments.
Future investigations should include a timeline of continuous PWV measurement, as well as intermittent measurements during prolonged exercise to better characterize the vascular effects of this form of physical activity.
5. CONCLUSION
There were no significant changes in arterial stiffness parameters and central arterial pressure during the event, except for a decreased cSBP in relation to baseline assessment on the first day, which did not change along the race course. There was a positive and moderate correlation between CK-MB and peripheral vascular resistance on days 1 and 4, as well as between troponin T and cSBP on day 4.
According to the results during the assessed period, this exercise modality did not appear to change arterial stiffness and cBP in functionally active and healthy adult men.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHOR CONTRIBUTIONS
WMS, MBE, PVOV and WKSB contributed in research concept and design; data collect; data analysis and interpretation and writing the article. PVOV, ALS, TVJ, PCVJ, AC, GG, ECDB and WKSB contributed in critical revision of the article. PVOV and WKSB contributed in final approval of article.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Wátila Moura Sousa AU - Maicon Borges Euzébio AU - Priscila Valverde de Oliveira Vitorino AU - Ana Luiza Sousa AU - Thiago Veiga Jardim AU - Paulo Cesar Veiga Jardim AU - Antonio Coca AU - Gonzalo Grazioli AU - Eduardo Costa Duarte Barbosa AU - Weimar Kunz Sebba Barroso PY - 2019 DA - 2019/11/18 TI - Arterial Stiffness, Central Blood Pressure, and Cardiac Biomarkers in Long-Distance Walkers JO - Artery Research SP - 71 EP - 76 VL - 25 IS - 1-2 SN - 1876-4401 UR - https://doi.org/10.2991/artres.k.191106.002 DO - 10.2991/artres.k.191106.002 ID - Sousa2019 ER -
