Assessment of Arterial Stiffness by Brachial Oscillometry in Community Pharmacies for Managing Hypertension (COPHARTEN)☆
 , Rosa Prats2,
, Rosa Prats2,  , Otón Bellver2,
, Otón Bellver2,  , Javier Reig2,
, Javier Reig2,  , Pedro Cunha3, †,
, Pedro Cunha3, †,  , María Teresa Climent2,
, María Teresa Climent2, 
Iberian Network on Arterial Structure, Central Hemodynamics and Neurocognition, Universidade do Minho, Department Escola de Medicina, Braga, Portugal.
- DOI
- 10.2991/artres.k.191124.001How to use a DOI?
- Keywords
- Arterial stiffness; target organ damage; pulse wave velocity; brachial oscillometry; prehypertension; community pharmacies
- Abstract
Background and Objective: Arterial Stiffness (AS) measured as pulse wave velocity has emerged in recent years as a hypertension mediated organ damage with independent prognostic value for Cardiovascular (CV) diseases that has also been discussed as a potential cause of Hypertension (HTN). The aim of this study is to (1) evaluate how measurement of AS modifies CV risk calculation by SCORE, (2) to measure the predictive value of AS for incident hypertension in normotensive patients, and (3) to analyze the association between control of HTN and presence of AS in sustained HTN.
Patients and Methods: A longitudinal, prospective, observational trial under conditions of daily pharmaceutical and clinical practice will be conducted in approximately 60 community pharmacies of the Iberian Peninsula in normotensive and/or hypertensive patients entering a pharmacy spontaneously. In the first cross-sectional step, AS will be estimated with a semi-automatic, validated device (Mobil-O-Graph®, IEM), followed by a 10-item questionnaire. The patients will be referred to Primary Care for stratifying risk by SCORE tables and standard evaluation. In the second longitudinal step, patients will be asked to repeat the visit after 12 months.
Discussion: This study aims to improve CV risk stratification and to investigate the potential of AS in predicting incident HTN in normotensive subjects. Besides, it will analyze the role of arterial stiffness as an associated factor to prevent control in sustained HTN in a setting of cooperation between community pharmacies and physicians in daily clinical practice.
- Copyright
- © 2019 Association for Research into Arterial Structure and Physiology. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
1.1. Unmet Needs in Hypertension Research
Cardiovascular (CV) diseases remain the main cause of death in Spain and Western Europe with rapidly increasing incidence in Latin America. Hypertension (HTN) is the most important determinant of CV death. It firstly became 2016 the most prevalent chronic disease in Spain with 18.5% of the whole population affected, overtaking chronic back pain [1]. According to recent estimations, approximately 12 million subjects suffer HTN in Spain, but only 7 million Spaniards are aware of, less than half of them are treated, and only 2.5 millions thereof are adequately controlled. These numbers are equivalent to 9.5 million people with uncontrolled HTN in Spain, translating into an estimate of 100 CV deaths daily [2].
There are four main uncovered needs intimately associated with the natural history of HTN. The first uncovered need refers to the role of HTN in the CV risk stratification of patients. CV risk stratification has been long recognized as an important tool for treating hypertensive patients and the population, in general. Several risk charts have been proposed and most countries do use nationally adapted tables to predict CV risk [3]. Although the specific weight of HTN varies from chart to chart, all of them include HTN as a pivotal item in risk calculation. However, even though relative risk is undoubtedly associated to higher risk predicted by charts, more CV events take place in absolute numbers in the intermediate and low risk groups than in the high risk group, simply because the latter is numerically much smaller than the first groups [4]. In other words, CV risk charts fail in identifying patients at high risk and the inclusion of HTN is clearly not sufficient to guarantee an accurate risk prediction in risk tables. Introducing new terms—such as arterial stiffness (AS)—in the equation of risk chats should improve their capability to recognize high risk.
The second call for action results from estimating incident HTN and whole life risks. For normotensive adults 45 years of age, the 40-year risk of developing HTN varies between 84% and 93%, depending on ethnicity [5]. Motivated by promising results in large randomized trials [6], ESH-Guidelines underlined 2007 the principle of “the lower, the better”, but the reappraisal 2009 moved to the recommendation of “the sooner, the better”, focusing on early diagnosis and treatment of HTN and estimation of CV risk. Nevertheless, studies analyzing factors causally related to incident HTN are scarce, because most of the research is directed to treating established HTN. Primordial prevention of HTN is therefore a population-oriented strategy that would reduce enormously the incidence and costs in the management of HTN [7]. A tool directed to identifying healthy subjects who later will develop HTN would improve precociously the management of HTN.
The third controversy related to HTN affects the treatment goal in established HTN. Once HTN is diagnosed, it exhibits in the vast majority of cases a progressive, chronic and worsening profile [8]. HTN can be controlled, but not cured, and even well controlled hypertensives have a higher residual risk than the normotensive population [9]. Recent studies claim for a more aggressive approach, even in high-risk patients [10]. The latest Guidelines of the AHA/ACC have reopened a great debate about treatment targets [11]. Conversely, the concept of fragility associated to high risk has emerged as an important argument against excessive lowering of treatment goals [12], even in studies apparently supporting lower targets [13], reinforcing the concept that simple blood pressure-derived goals must be complemented with other considerations. Very recently released Guidelines of the ESH/ESC stick to the previously defined thresholds of HTN, but have slightly decreased the targets of treatment, reinforcing the modifying role of Hypertension Mediated subclinical target Organ Damage (HMOD) on CV risk stratification [14].
The fourth and last debate in relation with HTN points to a fundamental structural dimension. Health systems vary in a series of different parameters. Grade of control of HTN in each country is a frequently used indicator, showing huge differences and ranging between 17.8% in Western Europe and 27.1% in Eastern Europe [15]. Access to health care services represents a key variable that could explain some of these differences. Ambulatory Blood Pressure Measurement (ABPM) may serve as an example, because it is performed routinely in many countries [16], but rarely in others [17]. Another characteristic, strongly varying item that characterizes each health system is the grade of interaction between the different actors, specifically between pharmacists and physicians. The introduction of electronic prescriptions has led to a growing responsibility of pharmacists in health systems, because measurement of adherence is now more feasible than with handwritten recipes. Besides, pharmacists retain in most countries a key position in the management of patients, even in societies where health care systems are 100% managed by the state administration, and where physicians’ ability to influence structural changes is only marginal or restricted to the private sector. As a consequence, the possibilities of pharmacists to interact with patients and improve their adherence is high and independent of administrative restrictions. The increasing role of pharmacists in health systems [18] opens new opportunities to promote a collaborative effort with physicians to early identify subjects at risk of CV Diseases (CVD) or non-compliant to prescribed treatments—a strategy that could unify the action of pharmacists and physicians toward a common pathway to achieve a better BP control and early identification of individuals that could deserve a more stringent follow-up. Assessment of BP, either as office, punctual determination, or as ABPM is an example of an existing, structural conflict between these collectives. As a result, even normal values for pharmacy BP measurements are still a matter of debate [19]. A strategy that could unify the action of pharmacists and physicians toward a common pathway to achieve better BP control is urgent.
1.2. Proposed Solutions
Several strategies have been undertaken to stop the epidemic growth of HTN, including the development of new drugs or fixed-dosed drug combinations, as well as lifestyle interventions. The last pharmacological class entering the market of antihypertensive drugs was the group of Angiotensin Receptor Blockers (ARBs) in 2005. Besides, other drugs with intrinsic, a priori not anticipated BP-lowering effect have been developed in the field of diabetes, such as gliflozines. Similarly, lifestyle interventions using new technologies, such as online-programs to improve adherence and self-empowerment, are in progress [20], but access to the web, especially at higher ages, and lack of consciousness for CV diseases, are important limitations to these individual-based strategies. Management of HTN remains therefore poor in the vast majority of countries, achieving <50% of adequate control.
In recent years much attention has been placed on the so-called HMOD, defined as intermediate markers of organ systems that on the long run lead to overt CV clinical diseases. HMODs are said to emerge in the middle of the CV continuum, integrating the influence of several CV risk factors during the life of individuals. They affect several systems, show different characteristics and can be assessed by a vast variety of methods, even within the same organ. For example, cardiac damage can be defined by a pathological increase of left ventricular mass, leading to left hypertrophy. ECG as well as echocardiography are adequate techniques to measure left ventricular mass, according to clinically well-established thresholds. But diastolic function has been equally recognized as a valuable parameter to identify cardiac damage caused by HTN. Similarly, urinary albumin excretion and estimated glomerular rate function are appropriate markers of subclinical renal damage, while cerebral lacunar infarcts and abnormalities of the retinal microvasculature demonstrate early damage in brain and eyes, respectively.
At least as important as the mentioned organ systems is the arterial tree. Vascular, arterial damage plays a key role in HTN, because virtually every organ in our body, and especially the heart, the kidneys and the brain, is target of the arterial conduits. Measurement of intima-media thickness, presence of atherosclerotic plaques or ankle-brachial index are classical examples of subclinical HMOD in the arterial system. Common to the latter markers of vascular damage is their independent prognostic value to predict CV events, but also the fact that they represent mainly markers of advanced CV disease. Besides, contrary to left ventricular hypertrophy or pathological urinary albumin excretion, there are no available data showing that these HMODs are susceptible of regression [21] or that this regression, if feasible, is beneficial for prognosis.
1.3. Arterial Stiffness
A new marker of HMOD emerged in the last two decades, Arterial Stiffness (AS), defined as increased Pulse Wave Velocity (PWV), measurable in large, elastic arteries with different techniques. AS shares with all the other HMODs the ability to improve prediction of CV events independently from other known risk factors and is equally recommended by the latest Guidelines of Management of HTN [14]. However, AS possesses three unique characteristics that justify the present study.
First, AS is recognized as a potential abnormality implied in the genesis of HTN at the very beginning of its natural history. In other words, some observations suspect a causal relationship between AS and HTN, where AS would precede the appearance of HTN. Though a definite answer to the question who is the chicken and who the egg is still lacking, there is growing evidence for interpreting AS as a causal factor of HTN [22–24], while others still consider AS a consequence rather than a cause of HTN [25].
Second, presence of AS complicates control of HTN as shows the fact that isolated HTN is associated with AS [26]. To which extent HTN itself is implied in worsening AS, is again a matter of debate, for the relationship between AS and HTN probably resembles a vicious circle that is difficult to interrupt [27]. The interaction between AS and HTN through time has been referred to as conundrum. AlGhatrif and Lakatta [28] and Scuteri et al. [29] showed that AS presents higher rates of change with age and influencing BP levels.
The third and most attractive trait of AS refers to its accessibility. Even the strongest recommendation for implementing HMODs in the management of HTN does not make the diagnostic devices needed to assess them more available. Echocardiography, carotid damage and cerebral lacunae require ultrasound and magnetic resonance tomography, respectively, often at disposal only in specialized units, but far from the reach of Primary Care physicians. The gold standard for measuring AS non-invasively is carotid-femoral applanation tonometry, a time-consuming procedure that demands operator skills. Recently, a new technology has been developed, Brachial Oscillometry (BO), which is operator-independent, patients-friendly, and doable simultaneously with a measurement of blood pressure. It has been validated against invasive coronariography, tonometry and magnetic resonance tomography and offers very similar results to applanation tonometry [30–34]. In addition, the estimated aortic PWV by oscillometry has already been shown to be independently predictive of mortality [35].
The potential of AS measured by BO for planning broad screening programs is enormous. Given the hypothesis that increased AS may precede HTN, assessing PWV by BO should be able to identify subjects who present elevated PWV and who are supposed to develop HTN in the following period of time. And, of note, these patients would initially still show normotensive blood pressure values. In other words, measuring AS by BO in the large group of normotensive patients could target prehypertension, identifying prehypertensive patients and achieving primordial prevention of HTN at a large scale.
Although much less expensive and less complicated than other techniques for measuring HMOD, assessment of AS by BO does not skip the need for financial investment. Spain has been punished by a severe economic crisis for the last decade, leading to an unemployment rate of approximately 50% in subjects younger than 30 years and a decrease of public health care expenditures in the range of 6–7% in the period from 2008 to 2016 [36]. Assessment of AS remains therefore nowadays and probably in the next decade beyond the reach of Primary Care.
Measuring AS in community pharmacies could contribute to developing a large-scale project in the Iberian Peninsula to face the mentioned unmet needs in HTN: to identify prehypertensive patients within the group of normotensive subjects, who spontaneously enter community pharmacies for whatever reasons and who might develop HTN during the following 12 months. Furthermore, determining AS would allow to characterize patients with accelerated vascular aging, at risk of CVD, independently of their BP status,—sparkling a strict cooperation between pharmacies and health care centres, the first identifying such subjects and referring them to the latter, where physicians would perform a thorough CV phenotype and determine pharmacological and non-pharmacological measures fitted to each individual risk factors.
This project would be also useful to answer the first controversy concerning AS: to analyze the role of AS in the CV risk-stratification and check to which extent the risk prediction by SCORE is modified by the presence of AS. Besides, our study offers the possibility of approaching the third question related to the association between AS and HTN, by comparing the rate of BP control at baseline and follow-up between individuals with elevated AS and those with normal PWV. Finally, the design of our study demands a close collaboration between pharmacists and physicians, strengthening the frame of a bidirectional relationship between them and offering the patients a palpable example of teamwork.
2. OBJECTIVES
The main objective of this study is to develop and implement a protocol to test the hypothesis that AS measured by BO in patients entering community pharmacies can identify prehypertensive subjects and individuals at increased risk of CVD independently of BP status, in other words, to analyze the predictive value of AS for incident HTN and CV disease after 1 year of observation. Secondary objectives are: (1) to measure the added value of AS for the risk-stratification achieved by SCORE, including the comparison of the prevalence of AS with that of other markers of subclinical target organ damage available in Primary Care, such as left ventricular hypertrophy by ECG and microalbuminuria [37,38]; (2) to measure the frequency of white-coat and determine the influence of AS on the frequency and level of control of sustained HTN; and (3) to establish a pathway for patients shared by pharmacists and physicians for a comprehensive determination of BP and CV risk that includes ABPM and AS. On the long run, Community Pharmacies for Managing Hypertension (COPHARTEN) should be understood as a pilot study to integrate AS in the CV risk assessment together with SCORE (Figure 1).
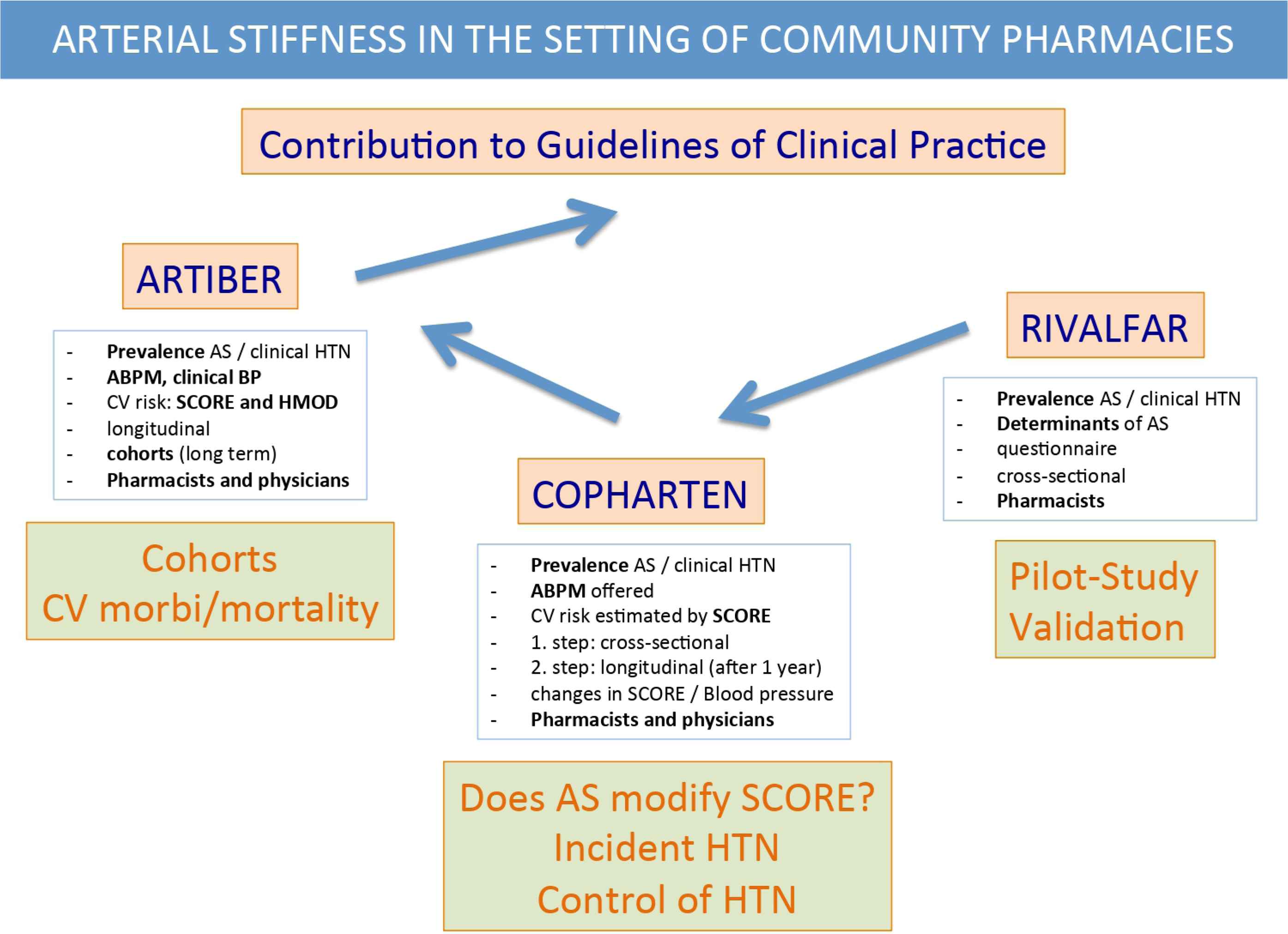
Long-term frame of COPHARTEN. ARTIBER: Arterial stiffness in the Iberian Peninsula.
3. METHODS
3.1. Study Design
This is a two-armed, multicentric, descriptive, observational study, comparing primarily two groups of patients: (a) normotensive subjects with normal arterial stiffness and (b) normotensive participants with elevated AS, measured by brachial oscillometry. The study will be conducted following the Consolidated Standards of Reporting Trials (CONSORT) statement (http://www.consort-statement.org [39,40]) and CONSORT-EHEALTH guidelines [41]. Besides, as a secondary objective, hypertensive patients under treatment will be also divided into those with normal and those with elevated PWV.
3.2. Setting and Study Sample
3.2.1. Pharmacies
This study will be conducted in the daily pharmaceutical setting of community pharmacies (Farmacias Comunitarias) and public Health Centers (Centros de Salud) of the Spanish National Health System (Sistema Nacional de Salud) at national level. Community Pharmacies are mandatorily affiliated to the local Official Pharmaceutical Association (Colegio Oficial de Farmacéuticos, COF) in each of the 52 provinces in Spain, accounting for a total amount of 21,854 pharmacies, with 18,980 (86.8%) in individual property and 35.9% of them located in the capital of each province [42]. The mean number of inhabitants per pharmacy is 2.140, with 4.7 pharmacies per 10,000 inhabitants and 386 subjects older than 65 years of age per pharmacy. The Spanish Association of Community and Family Pharmacies (Sociedad Española de Farmacia Familiar y Comunitaria, SEFAC), a scientific society of pharmacists, including approx. 4900 pharmacies in Spain, plays a pivotal role in the study. Recruitment of pharmacies will take place by public announcement of the protocol in the websites of COFs and SEFAC simultaneously, as well as with attendant meetings. It will thereby be guaranteed that the totality of pharmacies will have access to learn about the conditions and the protocol to voluntarily participate in the project. About 32 pharmacies, all of them members of SEFAC, out of 2301 community pharmacies (1.4%) in the Valencia Community, participated in the pilot study RIVALFAR (Estudio epidemiológico para cuantificar la prevalencia de hipertensión arterial y RIgidez arterial en las FARmacias Comunitarias de la Comunidad VALenciana), representing 9.1% of the 350 pharmacies ascribed to SEFAC [43]. Calculating a similar level of engagement in the whole territory, the number of recruited pharmacies would reach approx. 300 pharmacies. The minimum required to convey a solid and homogeneous sample of pharmacies would be three pharmacies in each Spanish province, with a total of approx. 150 participant pharmacists.
3.2.2. Physicians
Physicians of Primary Care will be invited to participate following the standards of daily clinical practice and to calculate the CV risk of the participating individuals according to SCORE by ordering the determination of lipids in an ordinary blood sample analysis. Within the Spanish public health system, Primary Care physicians are assigned to each individual usually for the whole professional life of the physician. Our Project will therefore involve all those physicians that actually have been taking and will take care of the individuals that are included in the Study. The pharmacist referring the patient will include a written explanation of the project, also containing a link to the website of the study. As part of a sub-study, the physicians will be asked to measure left ventricular mass by four different indices of ECG as well as urinary albumin excretion in a morning urine probe. Management of the patients will follow the daily clinical practice.
3.2.3. Sample size
The RIVALFAR-study [43] contains the real world data on which our calculations for the sample size are based. The proportion of participants with normal blood pressure and no antihypertensive treatment was 58%. Previous studies in prehypertensive patients show that an N of 124 patients was enough to find a significant difference of 4 mmHg between patients lying at baseline below the median value of AS versus the patients who were placed above the median value of AS, after 1 year of follow-up. According to the results obtained in RIVALFAR, the proportion of normotensive patients with elevated AS was approx. 10%. Accepting an α-risk of 0.05 and a β-risk of 0.2 in bilateral contrast, we would expect 1808 subjects in the first and 180 in the second group for detecting a significant difference between two proportions, which in the first group should be 0.09 and in the second group 0.03. The rate of follow-up losses has been estimated to be approx. 30%. The ARCOSENO approach has been used. Besides, a recruitment of one subject per week per pharmacy is expected, leading to at least 2400 patients during 4–6 months recruitment.
3.2.4. Patients
Paneling outside and inside the pharmacies will provide accessible information about the project. Subjects consecutively entering the pharmacies for any reason and showing interest for the study will be asked to participate by the personnel working in the pharmacies. Interested patients will be given an explanation, where they will receive more detailed information. If patients agree to participate, they will be asked for their informed consent, and after signing, they will get a copy. Participants should meet the following criteria: age older than 18 years. Exclusion criteria are refusal to participate, pregnancy or any disability that prevents or hinders understanding of the protocol.
3.3. Procedures, Measurement of Blood Pressure and Arterial Stiffness
To correctly identify real normotensive subjects and following international guidelines [14], office and ABPMs are mandatory, characterizing sustained HTN (elevated BP in office and ABPM), white coat HTN (elevated BP in office and normal ABPM) and masked HTN (normal BP in office and pathological ABPM). Subjects without previous antihypertensive treatment showing normotensive values in the pharmacy will understandably be reluctant to perform ABPM. Therefore, they will be considered “normotensive”, according to the RIVALFAR-protocol. ABPM will not be recommended for them, except elevated PWV is present. Similarly, treated hypertensive patients with normal BP and PWV will not be asked to perform ABPM. Consequently, ABPM will be indicated whenever arterial stiffness or high BP is recorded, either in never treated individuals or known hypertensive subjects.
In the last years, new devices have emerged to provide non-invasive estimates of PWV. The Mobil-O-Graph® (IEM GmbH, Stolberg, Germany, called Agedio® in pharmacies) uses a standard, inflated, brachial cuff and performs oscillometric measurements of the brachial artery pulse wave, its adaption to pharmacies is called Agedio®. Brachial oscillometry is based upon the registration of the arterial pulse wave on the brachial artery with a standard inflated cuff. This wave is then used to apply the so-called ARCSolver algorithms to calculate PWV according to gender, age, BP of the subject and the impedance of the registered curve [44]. It has been validated by direct comparison with applanation tonometry [45], by invasive angiography [30] and by magnetic resonance tomography [33]. Agedio® is also validated for performing ABPM according to the ESH-Guidelines [46]. Table 1 shows the ABPM-protocol [47].
|
ABPM protocol according to ESH-Guidelines
3.4. Training and Recruitment of Pharmacies, Physicians and Patients
Sociedad Española de Farmacia Familiar y Comunitaria will offer the possibility to take part in the study. The acceptance to participate will necessarily imply a pre-study qualification of the pharmacies by an online educational program (IMPACHTA, Programa de capacitación en Hipertensión Arterial), developed in conjunction between SEFAC and the Spanish Hypertension Society (Sociedad Española de Hipertensión, Liga Española para la Lucha contra la Hipertensión Arterial), which has been running for the past 2 years [48]. Similarly, physicians will be encouraged to deepen their knowledge in vascular medicine by making actual contents about AS available online.
The study has been reviewed for approval by the Committee for Ethics of the University CEU Cardenal Herrera. This observational study does not imply the randomization of the sample or the application of additional interventions. After receiving a general explanation of the study, participants will get an Informed Consent document to sign. Before accessing the data, all researchers are required to sign a document assuring confidentiality. All information collected will be considered confidential and documented anonymously, according to the legal frame valid in the Valencia Region (Law 5/1999 and consecutive norms). This information cannot be used to identify the patients, being the only link between the data and the patient a code used exclusively for this study.
4. PROCEDURES
The study will take place in two consecutive steps, an initial cross-sectional phase, and a longitudinal phase after 1 year.
4.1. Baseline Visit
In all patients, personal history will be assessed by means of a standard questionnaire (see Appendix 2). Body weight, height, and waist circumference will be measured and Body Mass Index (BMI) will be calculated. BP measurement will take place using brachial oscillometry with Agedio® (IEM GmbH, Stolberg, Germany), a semi-automatic tensiometer validated by the ESH, with the patient resting alone quietly. The Agedio® performs automatically a first measurement for the purpose of calibration. After an interval of respectively 1 min, a second and a third measurement is realized for determination of PWV, the mean value of the last two are used for calculating peripheral, central BP, PWV, Augmentation Pressure (AP) and Augmentation Index (Table 2). HTN is defined as systolic BP ≥ 140 or diastolic BP ≥ 90 mmHg. BP was measured according to ESH recommendations [14] as the mean value of the last two out of three consecutive measurements and taking into account published quality standards [49]. Arterial stiffness will be defined as measured PWV exceeding the 90-percentile of the median value of the corresponding age group, according to seven 10-year intervals from 20 to over 70 years of age (see Appendix 3) [44]. In order to increase the comparability of the measured results, we will also include and discuss other reference values, according to carotid-femoral PWV (cfPWV) obtained by applanation tonometry (The Reference Values for Arterial Stiffness’ Collaboration) [50]. Patients with elevated PWV and/or elevated BP will be offered to perform an ABPM in the following days (Figure 2).
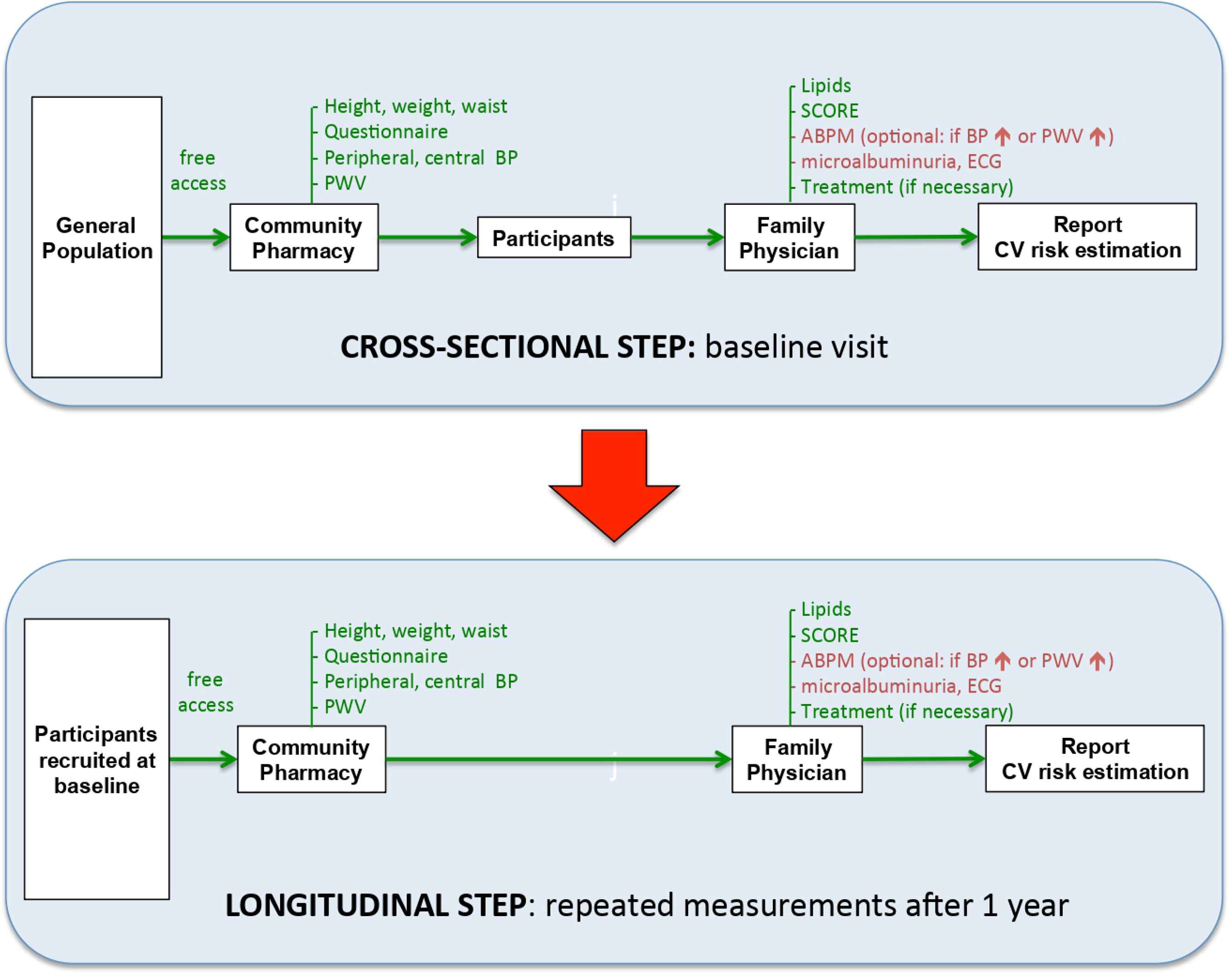
Flow-chart of participants and variables measured. Green: variables measured in Community Pharmacies and Primary Care. Red: optional measurements.
|
Measurement of pharmacy blood pressure, pulse wave velocity and other stiffness-related variables throughout the study
The results of these procedures will be documented in form of a report handed over to the subject, together with an explanation of the objectives of the study and an invitation to collaborate for the physician. All the participating individuals will then be asked to visit their family physician to present the results and to stratify the subject’s CV risk according to the SCORE table, mainly by measuring blood lipids. ABPM should be performed whenever possible in the Primary Care Centers. Willing, participating physicians will be given the possibility to determine left ventricular mass by ECG according to the ESH-Guidelines (Sokolow-Lyon index >3.5 mV/modified Sokolow-Lyon >3.5 mV/RaVL >1.1 mV/Cornell voltage duration product >244 mV*ms) and/or microalbuminuria on morning spot urine (>30 mg/g). Clinical data will be centralized and documented anonymously in a database, respecting confidentiality, according to the legal frame valid in the Valencia Community, as stated before. Participants will be given a written appointment for the follow-up visit after 12 months.
4.2. Follow-up Visit
All the procedures described in the Baseline Visit, including the questionnaire, the measurement of anthropomorphic variables and PWV in the pharmacies, as well as lipids and stratification of CV risk by the physicians will be repeated 1 year later.
4.3. Statistical Data Analysis
The results will be expressed as mean ± SD for continuous variables and as percentages for categorical variables. Variables with skewed distributions will be given as the median and Interquartile Range (IR). Variables found to deviate from normality will be log transformed (log) before statistical analysis. Differences in parameters of interest between patients will be sought by the Mann–Whitney U test or Wilcoxon test. Comparison of proportion among groups will be performed using the Chi-square test. Statistical significance is assumed if p < 0.05 (two-tailed). IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp. will be used for statistical analysis.
4.4. Endpoints
The primary endpoints of the study are: (1) the difference in the rate of incident hypertension between normotensive patients with elevated PWV versus normotensive patients with normal PWV at baseline and (2) development of CV disease (MACE, Major Adverse Cardiac Events).
Secondary endpoints include: (1) the difference in the proportion of BP control between hypertensive patients with elevated PWV versus hypertensive patients with normal PWV at baseline and follow-up; (2) the change of CV risk stratification by the fact of adding arterial stiffness to the SCORE calculation at baseline as well as at follow-up. Patients classified as “low” or “intermediate risk” by SCORE who show elevated PWV would per definition move to the “high-risk”; (3) the contribution of ABPM to correctly determine BP control in study participants; (4) the proportion of successful pharmacist–physician pathways, i.e., how many patients establish a communication channel between the pharmacist and the treating physician.
5. DISCUSSION
Although managed for many decades with a huge arsenal of drugs, HTN is far from being well controlled in our environment. The importance of subclinical target organ damage for risk stratification is increasing beyond traditional, well-established risk tables, because they convey additional prognostic value. Arterial stiffness measured as PWV represents an example of how HMOD can improve risk prediction. However, although recommended by Guidelines, PWV is as a matter of fact not part of daily clinical practice. The restricted access to measuring HMOD is counterbalanced by the development of new technologies, capable of tackling HTN on a large scale, even raising the possibility of its primordial prevention or, at least, of recognizing subjects at high risk to develop HTN in a very early stage. Nevertheless, such a global strategy requires the collaboration of all the global players in the health system, pharmacists, physicians, nurses, administrators, as well as empowered subjects who act self-confidently and guided by evidence-based medicine and transparency.
The present study combines the unmet need of approaching HTN on a population basis with the Guidelines recommendation of assessing subclinical target organ damage by implementing the use of innovative technologies to measure PWV and improve risk prediction. Our protocol assumes a close collaboration between pharmacists and physicians that simultaneously encourages individuals to realize the meaning of CV risk stratification. The study induces and empowers the subjects to serve as self-confident link between pharmacists and physicians as long as the participants carry medical information of their own, provided by the pharmacists, to be complemented by the other partner in the health system, the physicians. This pathway pharmacist–physician should be bidirectional and complementary. The proposed collaboration between pharmacists and physicians in our protocol may serve to consolidate a model based on mutual confidence and evidence-based medicine, accounting for the specific roles of both players.
5.1. Limitations
The intention of our study is to enroll a huge number of subjects in the setting of Community Pharmacies, but it cannot nor is it intended to determine the prevalence of arterial stiffness at a population level. To which extent the measured frequencies of stiffness and incident HTN might correspond to real prevalence of both, cannot be assessed by this protocol, because the recruitment is based on subjects who spontaneously enter a pharmacy. We could not perform an active search for individuals according to a population census. Moreover, the proposed patients’ pathways might be specific for the Spanish Health System, where physicians are public servants used by the administration and possess very limited capability to invest autonomously in technology, and where patients lack freedom to choose their Primary Care physicians. Nevertheless, the high number of participating pharmacies in different cities and environments will increase the external validity of our data.
Blood pressure and central hemodynamics are characterized by a circadian rhythm. According to Guidelines, our study will recommend measurement of BP in pre-specified periods of the day. As COPHARTEN takes place in a Mediterranean setting, our recommendation will be 9:00 am–1:00 pm and 4:00–8:00 pm, but measurements outside these ranges will be also admitted, carefully registering exactly the time of measurement.
Pharmacists are attributed a key role in the longer-term management of hypertension in the 2018 ESC/ESH Guidelines for the management of arterial hypertension. However, ABPM measurement in pharmacies is still unusual and may prevent some individuals or physicians from performing it, therefore ABPM should be also allowed to be done in Primary Care whenever it is indicated.
Another important limitation is the assumption of a smoothly flow of information between pharmacists and physicians. In our environment, approximately only 50% of Primary Care physicians accept performance of ABPM by pharmacists for several reasons, while the vast majority of Primary Care physicians admit having no relationship with pharmacists in their neighborhood. Besides, the present study counts on empowered patients who are determined and autonomous enough to connect physicians with pharmacists in their own interest. Therefore, the success of this protocol will depend on the convincing work of pharmacists to empower participants to understand CV risk stratification. An additional obstacle is the out-of-date role of the administration, as long as arterial stiffness is still not included as option to modify CV risk in the electronic records of patients. Finally, though recommended by ESH-Guidelines, ABPM cannot be performed in 100% of subjects, especially in normotensive individuals with normal BP in the pharmacy. A small percentage of masked HTN might escape our definition of HTN.
TRIAL STATUS
The trial is starting on February 2020.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
MTC, PC and ER were responsible for study conceptualization and writing (review and editing), all the other authors listed in the COPHARTEN-Study Group supervised and agreed to the manuscript.
FUNDING
No financial support for the conduct of the research and/or preparation of the article was provided.
ACKNOWLEDGMENT
On behalf of the COPHARTEN-Study Group, supported by the Sociedad Española de Farmacia Familiar y Comunitaria (SEFAC), Iberian Network on Arterial Structure, Central Hemodynamics and Neurocognition.
ABBREVIATIONS
- ABPM,
ambulatory blood pressure measurement;
- ABI,
ankle-brachial index;
- AS,
arterial stiffness;
- BMI,
body mass index;
- BO,
brachial oscillometry;
- BP,
blood pressure;
- COF,
Colegio Oficial de Farmacéuticos;
- CV,
cardiovascular;
- ESC,
European Society of Cardiology;
- ESH,
European Society of Hypertension;
- HMOD,
hypertension mediated organ damage;
- HTN,
hypertension;
- IMT,
intima-media thickness;
- NHS,
National Health Service;
- PWV,
pulse wave velocity;
- SCORE
Systematic COronary Risk Evaluation;
- SEFAC,
Sociedad Española de Farmacia Familiar y Comunitaria.
APPENDICES
Appendix 1. List of collaborating community pharmacists
COPHARTEN-Study Group
ADELL ALEGRE, MANUEL; AGUSTIN ALVAREZ, EDUARDO; ALCAZAR FRANCO, SALVADOR; ALONSO NUÑEZ, MARISA; ANDRACA ITURBE, LEIRE; ANDRACA ITURBE, IRUNE; APARICIO CERCÓS, CRISTINA; BAIXAULI FERNANDEZ, VICENTE JAVIER; BALTANAS LATASA, ARTURO; BALTANAS LATASA, FELIX; BELLVER MONZÓ, OTON; CANO CONGOST, MARIETA; CASTILLO GARCÍA, MARÍA LIDON; CENTELLES FORNER, SANTIAGO; CLIMENT CATALÁ, MARÍA TERESA; COLOMER MOLINA, VICENTE; CORCOLES FERRÁNDIZ, EDELMIRA; DE ANDRES DIRUBE, ANTONIETA; DELGADO CORREA, FRANCISCO; DÍAZ DE RADA, MARÍA LUISA; DOLS ALONSO, DANIEL; FERRER ESTRELA, FERNANDO; FUENTES DE FRUTOS, JOSE ENRIQUE; GALINDO JUVERIAS, LAURA; GARCIA BARTOLOME, SONIA; GARCÍA SEVILLANO, LUIS; GARCÍA ZARAGOZA, EUGENIA; GONZALEZ MARTÍNEZ, CONSUELO; GRANEL IVORRA PEDRO; HERNÁNDEZ MARRERO, ROSARIO; HERNÁNDEZ TOMAS, LUIS; HERRERO MASCARÓS, ANTONIO; HUESO FIBLA, ENRIQUE; JARAIZ MAGARIÑOS, IRENE; JORDA REQUENA; JORDA REQUENA, ADELIA; RAFAEL; LLOPIS MIRÓ, MARÍA TERESA; LLORIS CARSI, JESUS MARIANO; LOPEZ MONCHO, MARÍA ELODIA; LUQUE DEL MORAL, RAUL; MARTIN OLIVEROS, ADELA; MARTINEZ MARI, SARA; MARTINEZ OLMEDO, RAFAEL; MENDEZ VILLAMIL-MATA, EDUARDO; MONLLOR CORCOLES, BLANCA; MORA PEREZ, FERNANDO; MUD CASTELLÓ, FERNANDO; NAVARRO CLERIGUES, ANDRÉS; ORTEGA MEDER-DÍEZ, JAIME; PERERA GRAU, MARIA; PERSEGUER TORREGROSA, ZENEIDA; PERÉZ BENAJAS, AMPARO; POYATO PADILLO, MARÍA DOLORES; PRATS MAS, ROSA; REIG LÓPEZ, JAVIER; RODRIGO SORIANO, MARÍA JOSE; ROSINACH BONET, JORDI; RUÍZ GONZÁLEZ, DESIRE; RUÍZ LOZANO, FANY; SALA CLIMENT, MARTA; SALAR IBAÑEZ, LUIS; SANCHIS BORONAT, MARÍA JOSEP; TOUS TREPAT, SALVADOR; URCULLU DONAT, BEGOÑA; VIDAL CANTOS, LINA.
Appendix 2. Questionnaire
- 1.
Is your visit to the pharmacy related to blood pressure?
□ Yes □ No - 2.
Do you suffer hypertension?
□ Yes □ No - 3.
Have you been prescribed antihypertensive medication?
□ Yes □ No - 4.
Are you taking antihypertensive medication?
□ Yes □ No - 5.
Have you been prescribed lipid-lowering medication?
□ Yes □ No - 6.
Are you diabetic or have you been prescribed antidiabetic medication?
□ Yes □ No - 7.
Are you smoker (at least one cigarette/week)?
□ Yes □ No - 8.
If you are ex-smoker, did you stop at least 5 years earlier?
□ Yes □ No - 9.
Have you ever suffered a heart attack or angina pectoris?
□ Yes □ No - 10.
Have you ever suffered a stroke (hemorrhagic or thrombotic)?
□ Yes □ No
Appendix 3. Reference values for brachial oscillometry [44]
| Normotensives (n = 1064) | |
|---|---|
| Age (years) | PWV (m/s), Median (10–90 Percentile) |
| <30 | 4.9 (4.4–5.3) |
| 30–39 | 5.5 (4.9–6.0) |
| 40–49 | 6.4 (5.8–6.9) |
| 50–59 | 7.5 (6.9–8.2) |
| 60–69 | 8.9 (8.2–9.7) |
| 70–79 | 10.6 (9.8–11.5) |
| >79 | 12.7 (11.6–13.3) |
Footnotes
See Appendix 1: List of collaborating Community Pharmacists
REFERENCES
Cite this article
TY - JOUR AU - Enrique Rodilla AU - Rosa Prats AU - Otón Bellver AU - Javier Reig AU - Pedro Cunha AU - María Teresa Climent PY - 2019 DA - 2019/12/05 TI - Assessment of Arterial Stiffness by Brachial Oscillometry in Community Pharmacies for Managing Hypertension (COPHARTEN)☆ JO - Artery Research SP - 121 EP - 130 VL - 25 IS - 3-4 SN - 1876-4401 UR - https://doi.org/10.2991/artres.k.191124.001 DO - 10.2991/artres.k.191124.001 ID - Rodilla2019 ER -
