Novel Aspects of Differences in Arterial Stiffness Parameters during Short Abstinent Period in Smokers vs. Non-smokers
 , Annamária Pakai1,
, Annamária Pakai1,  , Attila Cziráki2, Zsófia Verzár1, 2,
, Attila Cziráki2, Zsófia Verzár1, 2, 
- DOI
- 10.2991/artres.k.200725.001How to use a DOI?
- Keywords
- Tobacco smoking; arterial stiffness; augmentation index; pulse wave velocity; 24-h long examination
- Abstract
Although the effects of smoking on hemodynamics and arterial stiffness has already been evaluated from many aspects, self-controlled and 24-h data have remained a missing area. Ten healthy light smokers were examined in a cross-sectional observational study for 48 h [smoking was prohibited during the first 24 h (non-smoking day) and allowed during the second 24 h (smoking day)] with an oscillometric device. Control group consisted of ten healthy non-smokers. Peripheral blood pressures were significantly higher on the smoking day (134.11 ± 11.02 and 77.11 ± 10.64) than on the non-smoking day (127.23 ± 8.41, p = 0.017 and 71.25 ± 10.47, p = 0.02) or among non-smokers (120.80 ± 5.77, p = 0.005 and 68.37 ± 4.87, p = 0.04). Heart rate was significantly lower on the non-smoking day (64.89 ± 9.03) than among non-smokers (74.30 ± 8.22, p = 0.03) and on the smoking day (76.09 ± 10.53, p = 0.001). Pulse Wave Velocity (PWV) was significantly higher on the smoking day (7.48 ± 1.17) than on the non-smoking day (7.00 ± 1.28, p = 0.03). Peripheral blood pressure results confirmed that smoking leads to both acute and subchronic elevation. Lower heart rate of smokers on the non-smoking day than non-smokers can be the consequence of improper heart rate adaptation to everyday activities. PWV values improved during the one-day long abstinent period suggesting that it is the most sensitive stiffness value to smoking cessation.
- HIGHLIGHTS
- •
Systolic and diastolic blood pressure values were the highest on the smoking day.
- •
Heart rate of smokers was lower on the non-smoking day than that of non-smokers.
- •
PWV of smokers was higher on the smoking day than on the non-smoking day.
- •
There was no difference between AIX values on the non-smoking and smoking days.
- •
- Copyright
- © 2020 Association for Research into Arterial Structure and Physiology. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
It has long been recognized that tobacco smoking has great impact on morbidity and mortality. Despite declines, tobacco smoking remained the leading risk factor for disease burden in North America and Western Europe [1]. Approximately 30–40% of smoking-related deaths are due to cardiovascular diseases [2].
The hemodynamic effects of tobacco smoking include increased blood pressure, heart rate and myocardial contractility resulting in an increase in cardiac output and myocardial work [3]. This increased myocardial work is associated with an increased coronary blood flow by up to 40% in healthy individuals [4]. Nevertheless, due to endothelial injury and dysfunction [4,5], impaired vasodilatory reserve, prothrombic state, increased neutrophil and monocyte adhesion to blood vessels and promotion of inflammation [5], the increase in coronary blood flow is less than expected based on the level of myocardial work in the absence of nicotine. Moreover, in the presence of coronary artery disease smoking increases coronary vascular resistance [6] and decreases coronary blood flow [7]. Cigarette smoking during coronary angiography has been observed to acutely trigger coronary vasospasm [8].
Several studies have confirmed that arterial stiffness increases acutely after cigarette smoking as measured by Augmentation Index (AIx), Carotid-femoral Pulse Wave Velocity (cfPWV), Brachial-radial PWV (brPWV) or Carotid-radial PWV (crPWV) [9,10]. Kim et al. [11] reported that at baseline, the Brachial-ankle PWV (baPWV) was not significantly different between smokers and non-smokers but was significantly higher in chronic smokers 5 min after cigarette smoking and remained higher for 30 min [11]. According to a systematic review on 39 relevant studies [12] more studies reported significantly higher aortic or brachial PWV as well as AIx in chronic smokers than non-smokers. However, three different studies found no significant correlation between smoking status and cfPWV [12].
The importance of parameters describing arterial stiffness including PWV, aortic AIx and central Systolic Blood Pressure (SBPao) has been confirmed on patients with coronary artery disease [13] and hypertension [14,15] as well as on apparently healthy population [16] and young sportsmen [17]. Thus, the evaluation of arterial stiffness was included in the 2007 and 2013 European Society of Cardiology/European Society of Hypertension guidelines for the management of arterial hypertension, both in evaluating organ damage and in cardiovascular risk calculation [18,19].
The acute and chronic effects of smoking on blood pressure and heart rate are well described by previous studies [20–22]. Nevertheless, its effect on arterial stiffness has only been partially evaluated, in a systematic literature review paper [12]. Although several studies discuss the effects of smoking cessation on arterial stiffness, they are analysing only the chronic effects of smoking cessation (60 weeks, 6 months). Also the previous studies use single measurements of stiffness values and they were not self-controlled. Previous studies have shown that smoking elicit constriction of resistance arteries and lead to increases in systemic blood pressure [23]. Thus we hypothesized that arterial stiffness values change significantly in the first 24 h after smoking cessation due to the lack of vasoconstrictor effect of smoking [23]. Thus, our aim was to determine the effects of short-term smoking cessation on arterial stiffness via a continuous measurement method with the exclusion of individual variables.
2. MATERIALS AND METHODS
In the first phase of our study, 10 healthy light smoker (smoking a maximum of 10 cigarettes/day) volunteers were examined for 48 h with a non-invasive ambulatory oscillometric device (Arteriograph 24 distributed by Tensiomed Kft, Budapest, Hungary) between 1st April 2015 and 31st December 2015. The volunteers were ordered to abstain from cigarette smoking during the first 24 h and were allowed to smoke during the second 24 h. Inclusion criterion was smoking of at least 10 cigarettes during the second day. Day and night periods were adjusted individually; brachial systolic and Diastolic Blood Pressure (DBP), pulse and arterial pulse pressure waveform were measured, aortic SBP, aortic AIx, brachial AIx and aortic PWV were derived, whereas pulse pressure and mean arterial pressure were calculated in every 20 min during waking and in every 40 min during sleeping hours. As demonstrated in Figure 1, AIx was calculated as a difference of the reflected (second, backward, P2) and ejected (first, forward, P1) wave of the central pulse pressure waveform expressed as a percentage of pulse pressure. PWV was calculated as the jugulum-symphysis distance divided by the half of the return time. In the second phase of the study, 10 healthy, non-smoker, age-matched and BMI-matched volunteers were examined for 24 h with the same method between 1st July 2017 and 31st December 2017. Informed consent was obtained from all volunteers prior to the examinations.
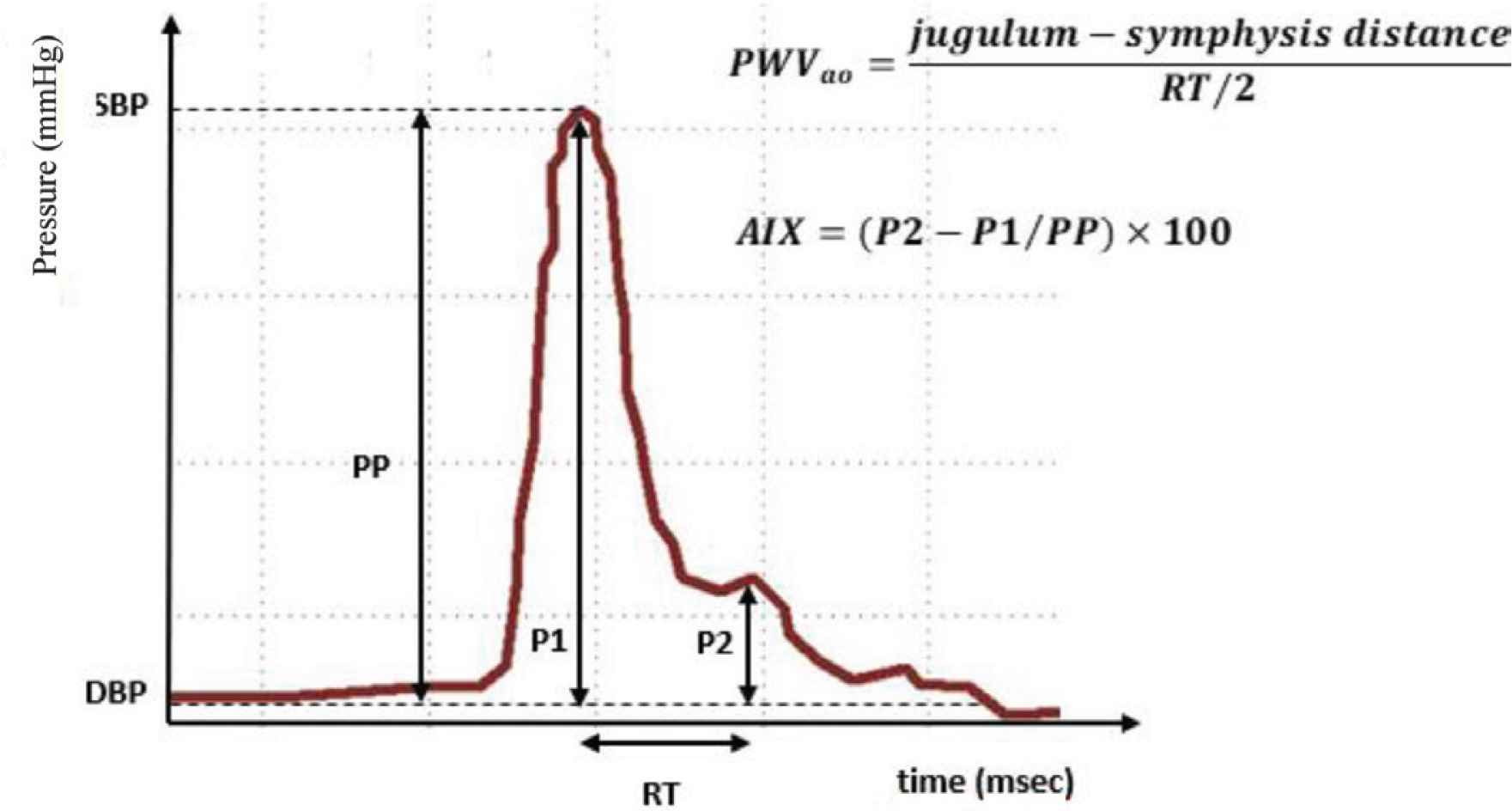
Calculation methods of pulse wave value and augmentation index from the pulse pressure waveform. P1, Amplitude of the forward pressure waveform minus diastolic blood pressure value; P2, Amplitude of the backward pressure waveform minus diastolic blood pressure value; RT, Return time; PP, pulse pressure.
All participant abstained from alcohol-containing beverages and physical exertion outside usual daily activities. Exclusion criteria included any kind of chronic disease that may affect cardiovascular function (e.g. chronic kidney disease, congenital heart defect or hypertension) and regular alcohol or drug consumption.
Each dataset was individually controlled and invalid data were eliminated resulting in an average of 46 remaining values per day per parameter. Regarding missing data, only missing completely at random type occurred during the study, these data were omitted from further statistical analysis. Socio-demographic and statistical analysis was performed with IBM SPSS Statistics v22.0 (IBM Corporation, Armonk, NY, USA). The sample was tested for normality using the one-sample Kolmogorov–Smirnov test. The results obtained from the light smoker group during the smoking and non-smoking days, expressed as means ± standard deviations were compared to each other using the paired-sample T-test. The results of the control group and the light smoker group were compared to each other with the independent samples T-test.
3. RESULTS
Mean age was 29.00 ± 8.78 years in the test group and 28.90 ± 10.72 years in the control group. Mean BMI was 22.89 ± 3.42 in the test group and 22.14 ± 2.33 in the control group. Neither in age (p = 0.98) nor in Body Mass Index (BMI, p = 0.57) was statistical difference found among the two groups. The test group consisted of seven men and three women, while the control group consisted of four men and six women.
Figures 2–4 demonstrate a representative pulse pressure waveform of a negative control, a smoking person on the non-smoking day and a smoking person on the smoking day, respectively.
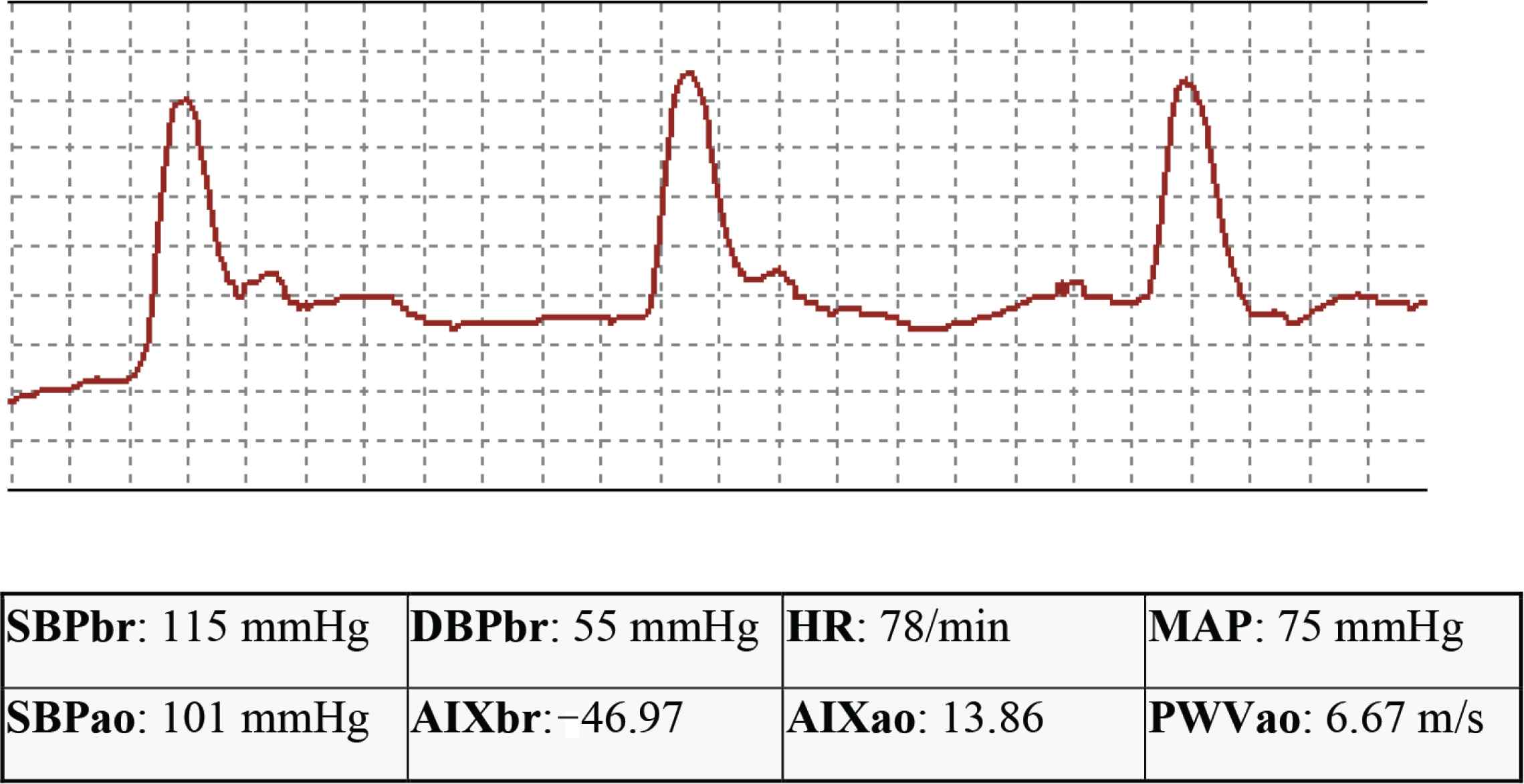
Original pulse pressure waveform of a negative control. SBPbr, brachial systolic blood pressure; DBPbr, brachial diastolic blood pressure; HR, heart rate; MAP, mean arterial pressure; PP, pulse pressure; SBPao, central systolic blood pressure; AIxao, central augmentation index; AIxbr, brachial augmentation index; PWV, pulse wave velocity.
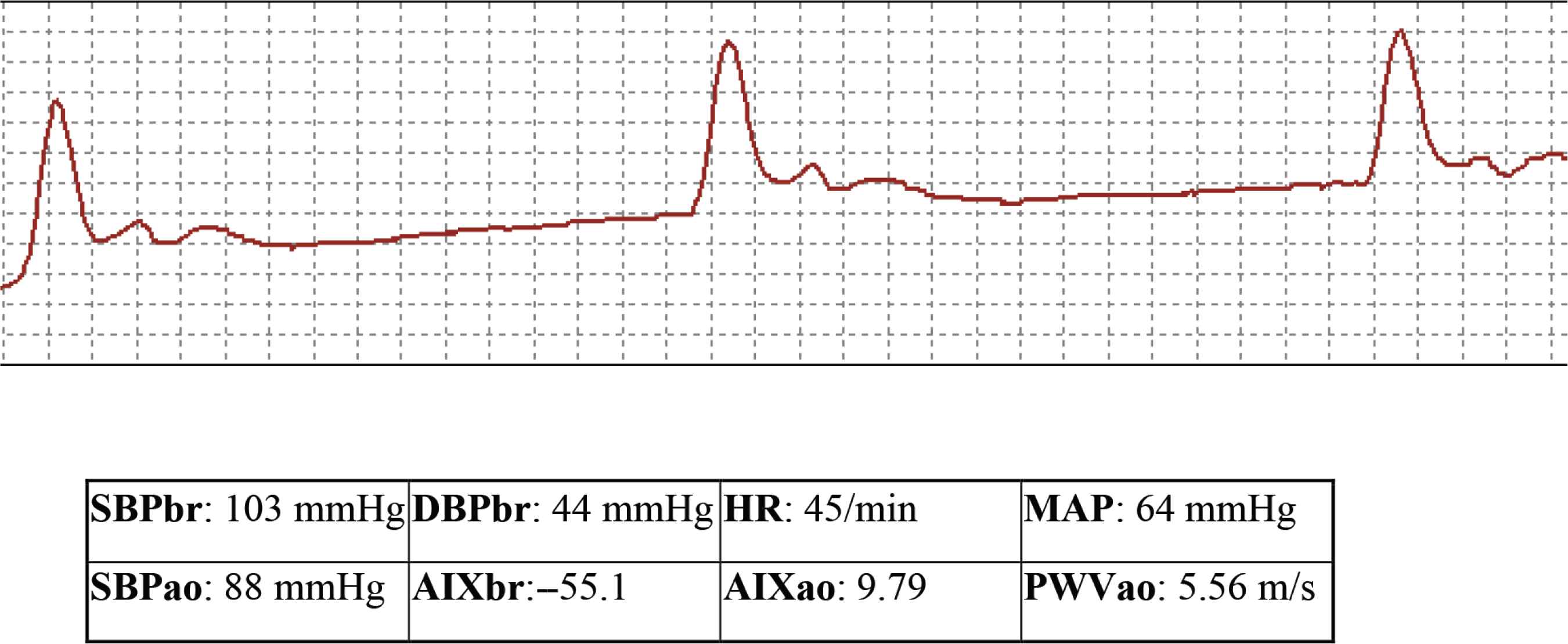
Original pulse pressure waveform of a smoker on the non-smoking day: There are no remarkable differences compared to the waveform of the control person. SBPbr, brachial systolic blood pressure; DBPbr, brachial diastolic blood pressure; HR, heart rate; MAP, mean arterial pressure; PP, pulse pressure; SBPao, central systolic blood pressure; AIxao, central augmentation index; AIxbr, brachial augmentation index; PWV, pulse wave velocity.
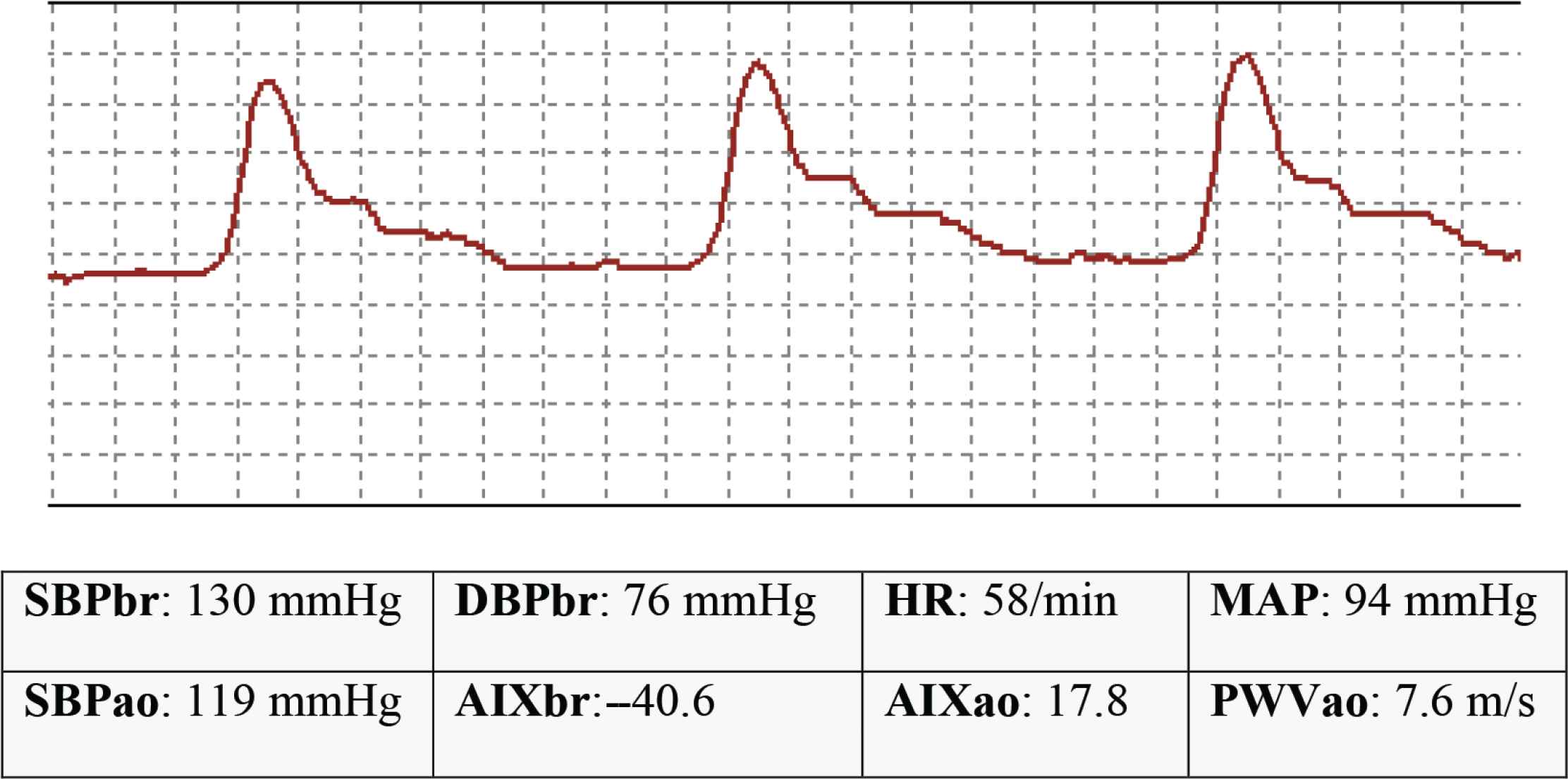
Original pulse pressure waveform of a smoker on the smoking day: The waveform is remarkably distorted due to the shortening of return time (and consequently, the increase of pulse wave velocity), however, no considerable change can be observed in augmentation index values. SBPbr, brachial systolic blood pressure; DBPbr, brachial diastolic blood pressure; HR, heart rate; MAP, mean arterial pressure; PP, pulse pressure; SBPao, central systolic blood pressure; AIxao, central augmentation index; AIxbr, brachial augmentation index; PWV, pulse wave velocity.
Table 1 summarizes the mean Brachial SBP (SBPbr), Brachial DBP (DBPbr), heart rate, Mean Arterial Pressure (MAP), pulse pressure, SBPao, Central AIx (AIxao) and Brachial AIx (AIxbr) and PWV values in the non-smoking group and in the smoking group on both non-smoking and smoking days.
| Smokers | Non-smokers | ||
|---|---|---|---|
| Non-smoking day | Smoking day | ||
| SBPbr (mmHg) | |||
| Daytime | 127.23 ± 8.41* | 134.11 ± 11.02*,# | 120.80 ± 5.77# |
| Night-time | 118.64 ± 7.79□ | 116.30 ± 9.63# | 106.16 ± 9.10#□ |
| All-day | 125.15 ± 7.51□ | 129.61 ± 9.87# | 117.83 ± 6.23#,□ |
| DBPbr (mmHg) | |||
| Daytime | 71.25 ± 10.47* | 77.11 ± 10.64*,# | 68.37 ± 4.87# |
| Night-time | 64.40 ± 9.89 | 62.79 ± 8.84 | 57.59 ± 5.96 |
| All-day | 69.49 ± 9.57* | 73.43 ± 9.75* | 66.31 ± 4.39 |
| HR (1/min) | |||
| Daytime | 64.89 ± 9.03*,□ | 76.09 ± 10.53* | 74.30 ± 8.22□ |
| Night-time | 55.86 ± 7.50 | 59.24 ± 8.54 | 62.08 ± 9.61 |
| All-day | 62.89 ± 8.22*,□ | 71.63 ± 9.63* | 72.21 ± 8.50□ |
| MAP (mmHg) | |||
| Daytime | 89.91 ± 9.30* | 96.11 ± 10.42*,# | 85.85 ± 4.53# |
| Night-time | 82.48 ± 8.75□ | 80.63 ± 8.69 | 73.78 ± 6.68□ |
| All-day | 86.04 ± 8.42* | 92.15 ± 9.44*,# | 83.48 ± 4.39# |
| PP (mmHg) | |||
| Daytime | 55.98 ± 6.78 | 57.00 ± 5.80 | 52.43 ± 5.36 |
| Night-time | 54.24 ± 6.30□ | 53.50 ± 5.81 | 48.57 ± 5.47□ |
| All-day | 55.66 ± 6.39 | 56.18 ± 5.53 | 51.52 ± 5.27 |
| SBPao (mmHg) | |||
| Daytime | 112.82 ± 10.31 | 117.59 ± 14.95 | 111.52 ± 7.39 |
| Night-time | 112.06 ± 11.31 | 105.04 ± 14.12 | 100.88 ± 11.70 |
| All-day | 112.33 ± 9.92 | 114.09 ± 14.53 | 109.20 ± 8.31 |
| AIXao | |||
| Daytime | 15.26 ± 8.45 | 12.15 ± 9.43 | 17.79 ± 7.55 |
| Night-time | 23.12 ± 10.49 | 16.22 ± 8.36 | 22.78 ± 9.39 |
| All-day | 17.05 ± 8.47 | 13.41 ± 8.99 | 18.63 ± 7.87 |
| AIXbr | |||
| Daytime | −44.20 ± 16.69 | −50.34 ± 18.62 | −39.20 ± 14.02 |
| Night-time | −28.68 ± 20.72 | −42.30 ± 16.51 | −29.35 ± 18.55 |
| All-day | −40.67 ± 16.73 | −47.85 ± 17.76 | −37.54 ± 15.54 |
| PWV (m/s) | |||
| Daytime | 7.00 ± 1.28* | 7.48 ± 1.17* | 7.36 ± 1.11 |
| Night-time | 6.61 ± 1.19 | 6.73 ± 0.90 | 6.84 ± 0.84 |
| All-day | 6.86 ± 1.24* | 7.20 ± 1.01* | 7.26 ± 1.08 |
Significant difference between smokers on the smoking day and the non-smoking day.
Significant difference between smokers on the smoking day and non-smokers.
Significant difference between smokers on the non-smoking day and non-smokers.
SBPbr, brachial systolic blood pressure, DBPbr, brachial diastolic blood pressure, HR, heart rate, MAP, mean arterial pressure, PP, pulse pressure, SBPao, central systolic blood pressure, AIXao, central augmentation index, AIXbr, brachial augmentation index, PWV, pulse wave velocity.
Summary of mean brachial systolic blood pressure, brachial diastolic blood pressure, heart rate, mean arterial pressure, pulse pressure, central systolic blood pressure, central and brachial augmentation index and pulse wave velocity values in the non-smoking group and in the smoking group on both non-smoking and smoking days.
3.1. Systolic Blood Pressure
The SBP during daytime was significantly higher among smokers on the smoking day than either among smokers on the non-smoking day (6.88 ± 5.33 mmHg, p = 0.02) or non-smokers (13.31 ± 8.46 mmHg, p = 0.005). No statistical difference was identified between smokers on the non-smoking day and non-smokers (6.43 ± 6.84 mmHg, p = 0.06). Figure 5 represents the daytime SBPbr mean values and 95% confidence intervals in the different groups.
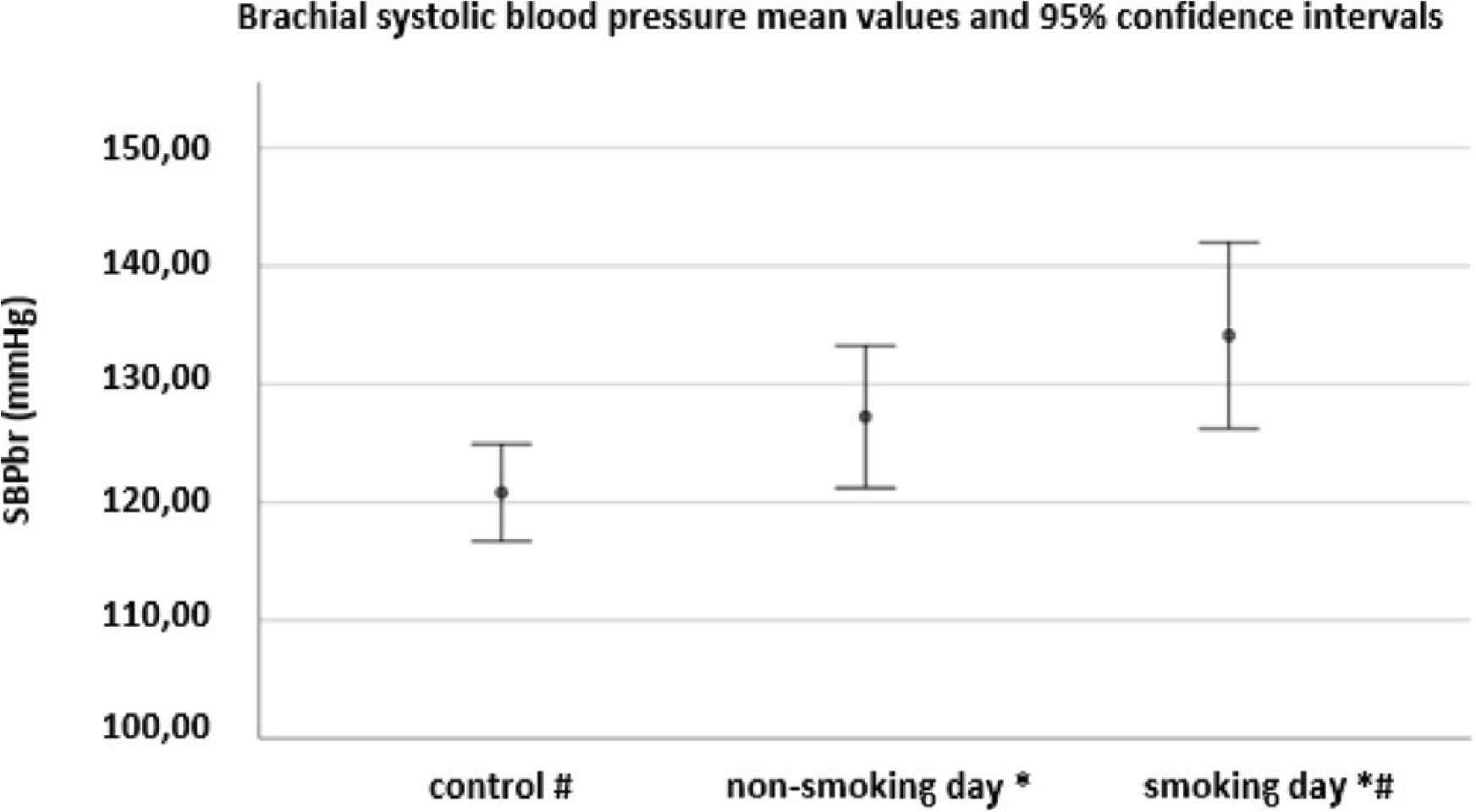
Brachial systolic blood pressure mean values and 95% confidence intervals among non-smokers, among smokers on the non-smoking day and among smokers on the smoking day. *Significant difference between smokers on the smoking day and on the non-smoking day (p = 0.02). #Significant difference between smokers on the smoking day and non-smokers (p = 0.005). SBPbr: brachial systolic blood pressure.
The SBP during night-time was significantly higher among smokers on both non-smoking (12.48 ± 7.96 mmHg, p = 0.004) and smoking days (10.14 ± 8.80, p = 0.03) than among non-smokers; however no statistical difference was detected between smokers on the smoking and non-smoking days (p = 0.38).
The daily SBP was significantly higher among smokers on both non-smoking (7.32 ± 6.48 mmHg, p = 0.03) and smoking days (11.78 ± 7.85 mmHg, p = 0.006) than among non-smokers; the difference among smokers between the non-smoking and smoking day was insignificant (4.46 ± 4.51 mmHg, p = 0.05).
3.2. Diastolic Blood Pressure
The DBP during daytime was significantly higher among smokers on the smoking day than among both smokers on the non-smoking day (5.87 ± 4.51 mmHg, p = 0.02) and non-smokers (8.74 ± 8.02 mmHg, p = 0.04); no statistical difference was identified between smokers on the non-smoking day and non-smokers (p = 0.44).
No statistical difference was revealed in DBP during night-time.
The daily DBP was significantly higher among smokers on the smoking day than on the non-smoking day (3.94 ± 3.39 mmHg, p = 0.03); however, no statistical difference was found between smokers on the non-smoking day and non-smokers (7.12 ± 7.32 mmHg, p = 0.36) or smokers on the smoking day and non-smokers (p = 0.06).
3.3. Heart Rate
The heart rate during day-time was significantly lower among smokers on the non-smoking day than among both non-smokers (9.41 ± 8.11 bpm, p = 0.03) and smokers on the smoking day (11.12 ± 5.26 bpm, p = 0.001); however, no statistical difference was noticed between smokers on the smoking day and non-smokers (p = 0.68).
No statistical difference was identified between the different groups in the case of heart rate during night-time.
The daily heart rate among smokers during the non-smoking day was significantly lower than on both smoking days (8.74 ± 4.26 bpm, p = 0.001) and among non-smokers (9.32 ± 7.85 bpm, p = 0.02). No difference was found between smokers on the smoking day and non-smokers (p = 0.89).
3.4. Mean Arterial Pressure
The MAP was significantly higher during daytime among smokers on the smoking day than among both smokers on the non-smoking day (6.20 ± 4.68 mmHg, p = 0.02) and non-smokers (10.26 ± 7.81 mmHg, p = 0.01); however, no statistical difference was detected between smokers on the non-smoking day and non-smokers (p = 0.24).
The MAP was significantly higher during night-time among smokers on the non-smoking day than among non-smokers (8.70 ± 7.32 mmHg, p = 0.02). Further differences were not proven to be statistically significant.
The daily MAP was significantly higher among smokers on the smoking day than among both smokers on the non-smoking day (4.11 ± 3.68 mmHg, p = 0.03) and non-smokers (8.67 ± 7.13 mmHg, p = 0.02); however, no statistical difference was detected between smokers on the non-smoking day and non-smokers (p = 0.15).
3.5. Pulse Pressure
No statistical difference was revealed between day-time and daily pulse pressure values of different groups.
The pulse pressure during night-time was significantly lower among non-smokers than among smokers on the non-smoking day (5.67 ± 5.54 mmHg, p = 0.046); however, further differences were not proven to be statistically significant.
3.6. Aortic Systolic Blood Pressure
No statistically significant differences were revealed between the groups during any time of the day.
3.7. Aortic and Brachial Augmentation Index
No statistically significant differences were detected between the groups in any time of the day.
3.8. Pulse Wave Velocity
Pulse wave velocity was significantly higher during day-time among smokers on the smoking day than on the non-smoking day (0.48 ± 0.41, p = 0.03). Figure 6 represents the day-time PWV mean values and 95% confidence intervals in the different groups. Similarly, the daily PWV was significantly higher among smokers on the smoking day than on the non-smoking day (p = 0.04). No other statistically significant differences were identified between the other groups in any time of the day.
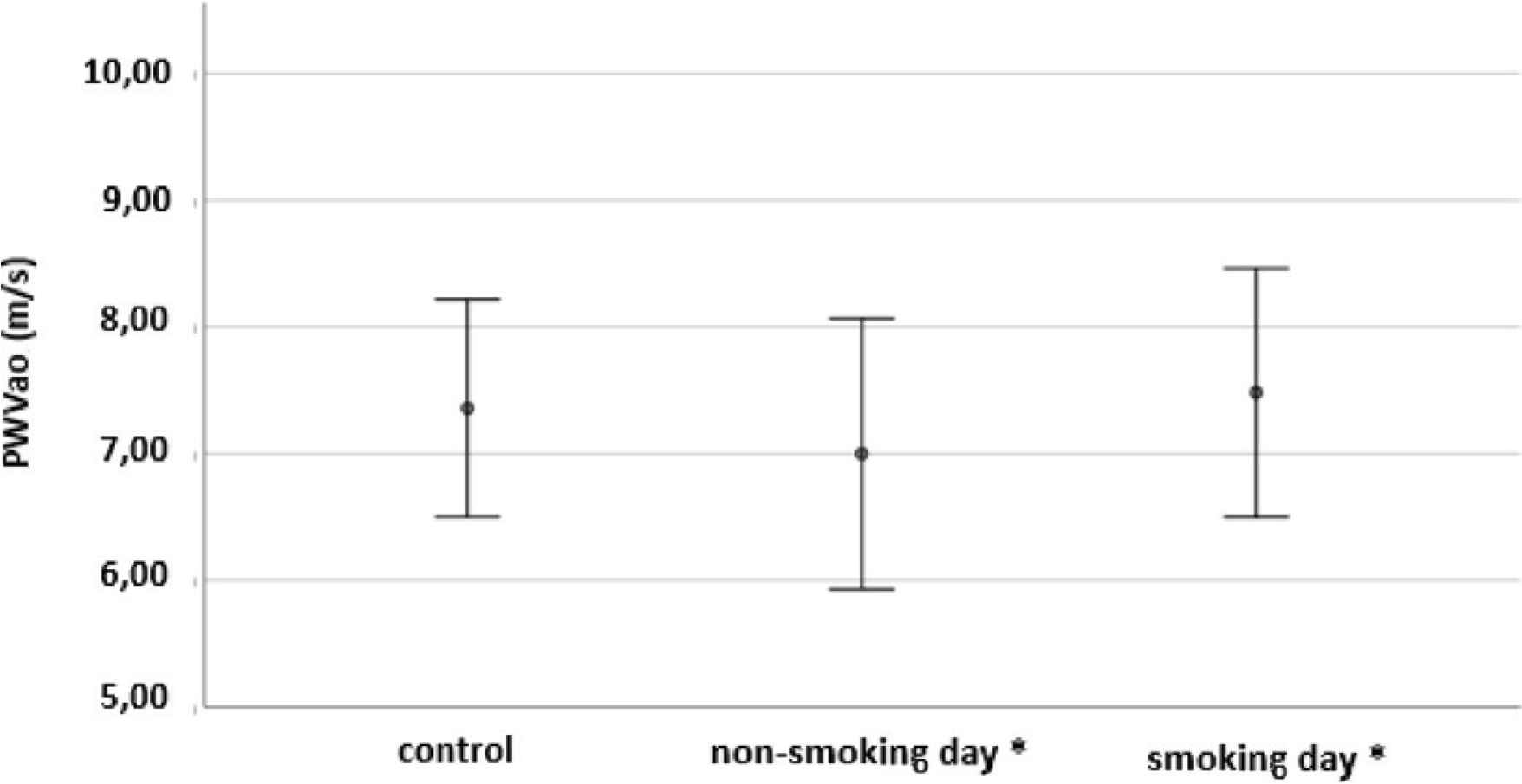
Pulse wave velocity mean values and 95% confidence intervals among non-smokers, among smokers on the non-smoking day and among smokers on the smoking day. *Significant difference between smokers on the smoking day and on the non-smoking day (p = 0.03). PWVao: central pulse wave velocity.
4. DISCUSSION
To the best of our knowledge, no data on 24-h or self-controlled stiffness parameters in smokers has been published to date. Our results confirm former observations in general, nevertheless add important novel aspects to those at several points.
The effect of smoking on peripheral blood pressure values remained a disputed issue, blood pressure values are expected to be higher in smokers due to sympathetic stimulation, which is confirmed by numerous studies [20]. However, others – using a single measurement method – did not find difference [9,21], whereas inverse relationship (i.e. lower systolic and DBP results in smokers) was also published [22]. In our research, the highest SBP values were measured during day-time in smokers on the smoking day (134.11 ± 11.02 mmHg). This value improved (with 6.88 ± 5.33 mmHg) in smokers on the non-smoking day to a similar value to the SBP of non-smokers. The same claim is proven to be true for daily SBP results. The analysis of night-time SBP results revealed that smokers had higher values on both smoking and non-smoking days than non-smokers; however, no significant improvement could be observed among smokers between the non-smoking and smoking days supporting the potent subchronic effect of smoking on DBP.
The DBP values during daytime were significantly higher in smokers on the smoking day than on the non-smoking day or in non-smokers. No difference was found between the results of smokers on the non-smoking day and non-smokers, though, suggesting that the subchronic effect of smoking on DBP is less substantial than on SBP. The latter is partially confirmed by the fact that no significant differences were found between the different groups during night-time.
Tobacco smoking is considered to cause an acutely and chronically accelerated heart rate due to sympathetic stimulation confirmed by numerous research data [21,22]. A study in 2013 found that smokers had higher resting heart rate, however, they showed lower heart rate increase during exercise [24]. Thus, the heart rate analysis in our study provided partially surprising findings. Evaluation of the results of smokers alone revealed that these were consistent with previous data, i.e. the heart rate of smokers on the smoking day was 11.20 ± 5.18 bpm higher than on the non-smoking day. Interestingly, the comparison with the results of non-smokers revealed that there was no difference between the values of non-smokers and smokers on the smoking day, but the value of smokers on the non-smoking day was proven to be 9.41 ± 8.10 bpm lower than that of non-smokers. A similarly designed study published in 2014 examining adolescents before and after smoking cessation and negative controls found that although resting heart rate results were in accordance with expectations, the heart rate of smoking subjects was significantly lower than the heart rate of healthy controls [25]. The authors explained this result with the different activity of participants, what is – based on the same orders given to participants – highly unlikely in our study. As all participants were involved in normal daily activities these results should rather be considered as a consequence of improper heart rate adaptation during exercise similarly to subjects in the study of Papathanasiou et al. [24].
Mean arterial pressure values during day-time and all-day were significantly higher among smokers on the smoking day than both smokers on the non-smoking day and non-smokers, and similarly to SBP and DBP no difference was found between smokers on the non-smoking day and non-smokers. The values during night-time appeared to be lower in non-smokers than in smokers on the non-smoking day, which is likely to reflect the effect of non-significant night-time difference in DBP between these groups.
Although significant differences were observed in both day-time and daily SBP and DBPs, the analysis of peripheral pulse pressure revealed no statistically significant differences in daytime or daily pulse pressure values suggesting that SBP and DBP values incremented proportionally as a result of smoking. During night-time the pulse pressure among non-smokers was lower than among smokers on the non-smoking day reflecting the greater increment in SBP than DBP (differences in SBP and DBP were 12.48 ± 7.96 and 10.14 ± 8.80 mmHg, respectively).
As more invasive and non-invasive studies demonstrated increased AIx is associated with an increased risk for coronary artery disease [13,26]. AIx was proven to be significantly lower after 1 year of cessation period [21] and appeared to be higher in chronic smokers compared to non-smokers with single measurement [9]. In our study, no statistically significant differences were found between the tested groups. Therefore, 1 day of abstinence seems to have no effect on AIxbr and aortic AIx.
According to the Strong Heart Study PWV as a direct representative of vascular stiffness has been related to cardiovascular risk in several patient populations [27]. PWV was found to be decreasing after 1-year of smoking cessation [21] and immediately after cigarette smoking as well [9]. The assessment of our PWV results revealed that – as expected based on the sympathetic stimulation caused by tobacco smoking – PWV during day-time and all-day was higher among smokers on the smoking day than on the non-smoking day. PWV is considered to reflect the actual state of vessels. Our results confirm this claim as PWV values were higher among smokers on the smoking day than on the non-smoking day. Nevertheless, the fact that PWV values improved to those of non-smokers during the 1-day long non-smoking period suggests that the analysed vascular changes are reversible in this young population.
5. LIMITATIONS
The main limitations of the study included the difficulty in recruiting this type of volunteer – i.e. the majority of potential “light smoker” participants declined participation due to the prolonged 24-h non-smoking period – resulting in consequent problems during statistical analysis and the evaluation of results. Further examinations are required to reveal further differences in a greater population. The relative great number of invalid measurements resulting from the sensitivity of the equipment to move has led to further difficulties during analysis and evaluation.
6. CONCLUSION
Although the relationship of smoking and cardiovascular risk factors has long been investigated, contradictory data was published (e.g. the effect of smoking on blood pressure) and open points have remained. Only a few self-controlled data exist in the field, mainly with limited measurement spectrum and/or focusing on the differences after a longer period (1 week, 1 year). Our study demonstrates a database capable of comparing various parameters between smokers during smoking day, smokers during non-smoking day and non-smokers. The changes in SBP and DBP, pulse pressure and MAP values followed the expectations. The unexpected changes in heart rate are likely to demonstrate an improper heart rate adaptation to everyday activities. Nevertheless, no difference was found in AIxbr and AIxao and SBPao values, whereas PWV values significantly improved during the 1-day long non-smoking period suggesting that PWV is the most sensitive parameter to smoking among the tested parameters.
CONFLICTS OF INTEREST
The authors whose names are listed immediately below certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patentlicensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
AUTHORS’ CONTRIBUTION
ZMB literature search, data collection, manuscript writing. AP contributed data or analysis tools, performed the analysis. AC substantial contribution to the conception and design of the study, critical revision of the manuscript, project supervision. ZV substantial contribution to the conception and design of the study, critical revision and editing of the manuscript, project administration. All authors have approved the final article.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ABBREVIATIONS
- AIx,
augmentation index;
- cfPWV,
carotid-femoral pulse wave velocity;
- brPWV,
brachial-radial pulse wave velocity;
- crPWV,
carotid-radial pulse wave velocity;
- baPWV,
brachial-ankle pulse wave velocity;
- ESC,
European Society of Cardiology;
- ESH,
European Society of Hypertension;
- BMI,
body mass index.
Footnotes
Peer review under responsibility of the Association for Research into Arterial Structure and Physiology
Data availability statement: The data that support the findings of this study are openly available in Mendeley Database at https://data.mendeley.com/datasets/ttjr6g88rx/1, reference number 10.17632/ttjr6g88rx.1 (DOI).
REFERENCES
Cite this article
TY - JOUR AU - Zsófia Mrekváné Burián AU - Annamária Pakai AU - Attila Cziráki AU - Zsófia Verzár PY - 2020 DA - 2020/08/07 TI - Novel Aspects of Differences in Arterial Stiffness Parameters during Short Abstinent Period in Smokers vs. Non-smokers JO - Artery Research SP - 212 EP - 218 VL - 26 IS - 4 SN - 1876-4401 UR - https://doi.org/10.2991/artres.k.200725.001 DO - 10.2991/artres.k.200725.001 ID - Burián2020 ER -
