Hemodynamic Data Analysis and Site of Measurement in Children and Adolescents
 , Nataša Marčun Varda
, Nataša Marčun Varda- DOI
- 10.2991/artres.k.201102.001How to use a DOI?
- Keywords
- Pulse wave velocity; pulse wave analysis; site of measurement; children
- Abstract
Pulse wave velocity is a method of functional vascular evaluation. The gold standard is the carotid-femoral pulse wave velocity measurement. However, the software allows measurement among radial, carotid and femoral artery. The goal of our prospective pilot study was to compare pulse wave velocity measurement among different arteries, not only carotid-femoral, in children and adolescents to find out, if the measurement can be performed in a simplified version with comparable results which would be especially important in younger children. Pulse wave velocity was measured in three different ways: carotid-femoral pulse wave velocity in lying position, carotid-radial pulse wave velocity in lying position and carotid-radial pulse wave velocity in sitting position. Additionally, central hemodynamic data were collected. There was statistically significant difference between: carotid-femoral pulse wave velocity and carotid-radial pulse wave velocity in lying position and carotid-femoral pulse wave velocity and carotid-radial pulse wave velocity in sitting position (p < 0.0001 for both). There was no significant difference between carotid-radial pulse wave velocity in lying or sitting position (p = 0.158). Analysis of central hemodynamic data showed statistically significant differences between subendocardial viability ratio (p = 0.001), end systolic pressure (p = 0.001) and central diastolic pressure (p = 0.001) when central hemodynamic data of carotid-radial measurements lying and sitting were compared, but there were no differences when the same parameters were compared between hemodynamic data of both lying positions, except for subendocardial viability ratio. The site of measurement significantly affects pulse wave velocity and can not be interchangeable. On the contrary, the position of the child does not affect pulse wave velocity, but could be important in hemodynamic data analysis.
- Copyright
- © 2020 Association for Research into Arterial Structure and Physiology. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Pulse palpation has been an integral part of physical examination through history. To quote Frederic Akbar Mohamed, pioneer in essential hypertension description: “Since the information which the pulse affords is of so great importance, and so often consulted, surely it must be to our advantage to appreciate fully all it tells us, and to draw from it every detail that it is capable of imparting’” [1,2]. Since then, much has been done in the field of pulse wave physiology, pulse wave analysis and pulse wave velocity measurement. Pulse wave is a propagation through arterial tree created by beating heart with blood pressure and flow pulsations. As waves are spread and reflected at transitions in arterial geometry and elasticity, they carry information about the matter in which they propagate [3].
One of the techniques of “pulse palpation” is applanation tonometry which allows us pulse wave analysis and pulse wave velocity measurement. Its use is increasing in both adults and children and much has been published in last 20 years. It has become obvious that it is reasonable to evaluate vascular elasticity with pulse wave analysis and pulse wave velocity assessment and to provide information beyond standard cardiovascular disease risk factors in the prediction of future cardiovascular disease events [4].
The advantages of applanation tonometry are the non-invasiveness, particularly important in children, repeatability, cost and portability of the device [5]. It is not recognized as a novel method anymore, but its use is still not applied in clinical routine. The most obvious disadvantage of the method is its inaccuracy, which firstly arises from an indirect assessment of the arterial path. Even with accurate measurements of the arterial path by magnetic resonance imaging, true pulse wave velocity is questionable, since we cannot guarantee that the velocities in all parts of the arterial path are the same (segments of the carotid, iliac, and femoral arteries differ in their elastic properties, which is even more pronounced in age). Additionally, measurements do not include the proximal aorta, which actually changes the most with age. Consequently, in adults and children carotid-femoral pulse wave velocity has been proposed as gold standard to ensure comparable results [4]. Peripheral pulse wave can sometimes be difficult to obtain, especially in subjects with low blood pressure, obesity or in children [5,6].
One of the devices, used in our department, is SphygmoCor Cardiovascular Management Suite® (AtCor Medical, Australia) that allows us measurement among different arteries – radial, carotid and femoral. Though carotid-femoral pulse wave velocity is preferred, in children, especially obese, another approach might be easier to perform regarding the fact that differences in vascular elasticity might not be as pronounced as in adults due to young age [7]. The limitations of pulse wave velocity measurement in children have been determined in many studies, specially ensuring that the patient is still and comfortable [8]. Therefore, the goal of our prospective pilot study was to verify if an alternative to carotid-femoral pulse wave velocity measurement could be established. We propose measuring pulse wave velocity between radial and carotid artery in the same position or preferably while the subject is sitting. Regardless the fact, that arteries differ in their elastic properties throughout the body as stated above, the following hypothesis of the study was that the pulse wave velocity, measured carotid-femoral in lying position could be the same as pulse wave velocity, measured carotid-radial in lying or sitting position due to different elastic properties in children and should be researched in the prusuit for a more appropriate way of measurement in our youngest patients.
2. MATERIALS AND METHODS
Fifty eight children and adolescents were analyzed using Sphygmo-Cor Cardiovascular Management Suite®. Only patients with known cardiovascular risk factors, e.g. hypertension and obesity, were invited in whom pulse wave velocity would be measured as a part of regular assessment because increased arterial stiffness has already been proven in these patients [9,10]. Pulse wave velocity was measured in three different ways: carotid-femoral pulse wave velocity in lying position, carotid-radial pulse wave velocity in lying position and carotid-radial pulse wave velocity in sitting position, which would be the most simplified method in our opinion. The measurement took place in the same order in all patients. Additionally, central hemodynamic data have been collected and analyzed.
Applanation tonometry is the most commonly used method for non-invasive pulse wave velocity measurement [6]. A micromanometer is placed on the skin, which allows the tonometric sensors to accurately detect the movement of the vessel and with it the travelling pulse wave, thereby detecting and obtaining a measurement of the shape of the pulse wave. The electrocardiographic signal is simultaneously recorded, which enables timing detection. Arterial path length is also measured and from the relationship between both, path and time, the device can estimate pulse wave velocity [11,12].
SphygmoCor devices have an integrated pulse waveform analysis based on the concept that the hemodynamic characteristics of the patient can be inferred from the pulse waveform. One of the main features of the device is the ability to generate a central aortic pulse wave from the pulse waves measured in the periphery from which central hemodynamic parameters can be obtained. From the obtained peripheral signal, a transfer function is used to calculate the aortic pulse wave. The software calculates more than 20 different aortic pulse wave related parameters. The most important are the aortic augmentation index, another marker of vascular elasticity, and the sub-endocardial viability ratio, a non-invasive indicator of myocardial load, oxygen delivery, and myocardial perfusion [5,11,13].
In our study we compared central hemodynamic data, namely augmentation index at heart rate of 75/min, sub-endocardial viability ratio, end systolic pressure, central systolic and diastolic pressure between different methods of measurement.
SPSS Statistics (IBM Version 22.0, IBM Corporation, Armonk, NY, USA) has been used for statistical analyses. Descriptive statistics and paired t-test were used for comparison of the results. Statistical analysis has been presented as Bland and Altman plot for pulse wave velocity measurements. Multivariate analysis was also performed. A value of p < 0.05 was considered statistically significant.
3. RESULTS
Thirty six male and 22 female patients were analyzed. In six patients carotid-femoral pulse wave velocity could not be obtained, in comparison to carotid-radial pulse wave velocity that was obtained in all cases, in both positions. Descriptive statistics of the researched group is presented in Table 1 with pulse wave velocity in all three positions. Next, we compared those results with paired t-test: there is statistically significant difference between both carotid-femoral pulse wave velocity and carotid-radial pulse wave velocity lying (p < 0.001) and sitting (p < 0.001), meanwhile there is no statistically significant difference between carotid-radial pulse wave velocity lying and sitting (p = 0.158). Statistical analysis has also been presented as the Bland and Altman plot presented with Figures 1–3 as the ratio between the difference and the average of the measurement for each case, with an average of −0.7891 ± 0.90895 in the first, an average of −0.9704 ± 0.97654 for second, and an average of −0.1603 ± 0.85285 for the last case. The statistical bias is present for Figures 1 and 2, but not in Figure 3, where the average is closest to zero, which confirms our results – in the last case, comparing carotid-radial pulse wave velocity sitting and lying, the results are comparable, otherwise not. A multiple regression analysis has been made to determine the effect of different factors (namely age, sex, height, weight, body mass index, systolic and diastolic pressure) on pulse wave velocity in each case. In case of carotid-femoral pulse wave velocity the adjusted R-square is 0.04 with significance of p = 0.285 and none of the factors is recognized as significant. In the second case, the carotid-radial pulse wave velocity in lying position the adjusted R-square is 0.146 with significance of p = 0.034 and with none of the factors, recognized as significant. In the last case, the carotid-radial pulse wave velocity, the adjusted R-square is 0.151 with significance of p = 0.031 and diastolic blood pressure recognized as important factor but with a p-value of only 0.049.
| Parameter | Mean ± SD |
|---|---|
| Age | 13.24 ± 3.9 (5, 21) |
| Height (cm) | 160 ± 16.5 (119, 190) |
| Weight (kg) | 66.8 ± 23.4 (22, 128) |
| BMI (kg/m2) | 25.2 ± 6.4 (15.5, 41.3) |
| Systolic pressure (mmHg) | 130 ± 15 (104, 161) |
| Diastolic pressure (mmHg) | 78 ± 11 (56, 101) |
| cfPWV (m/s) | 4.9 ± 0.6 (4.0, 6.0) |
| crPWV lying (m/s) | 5.7 ± 1 (4.1, 8.5) |
| crPWV sitting (m/s) | 5.8 ± 1 (4.1, 9.0) |
SD, standard deviation; BMI, body mass index; PWV, pulse wave velocity; cf, carotid-femoral; cr, carotid-radial.
Descriptive statistics and mean PWV
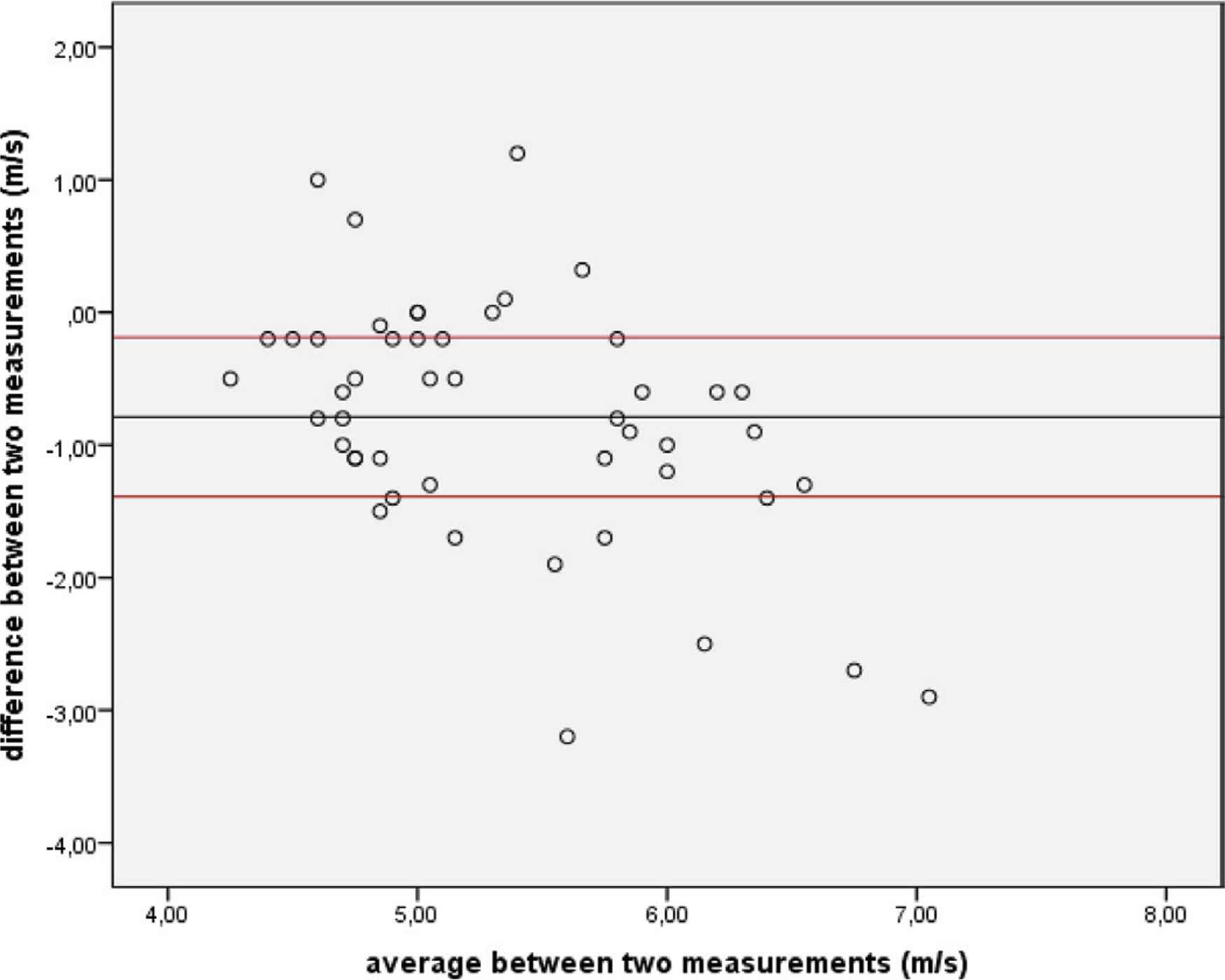
Bland and Altman plot for pulse wave velocity measurement performed carotid-femoral lying and carotid-radial lying.
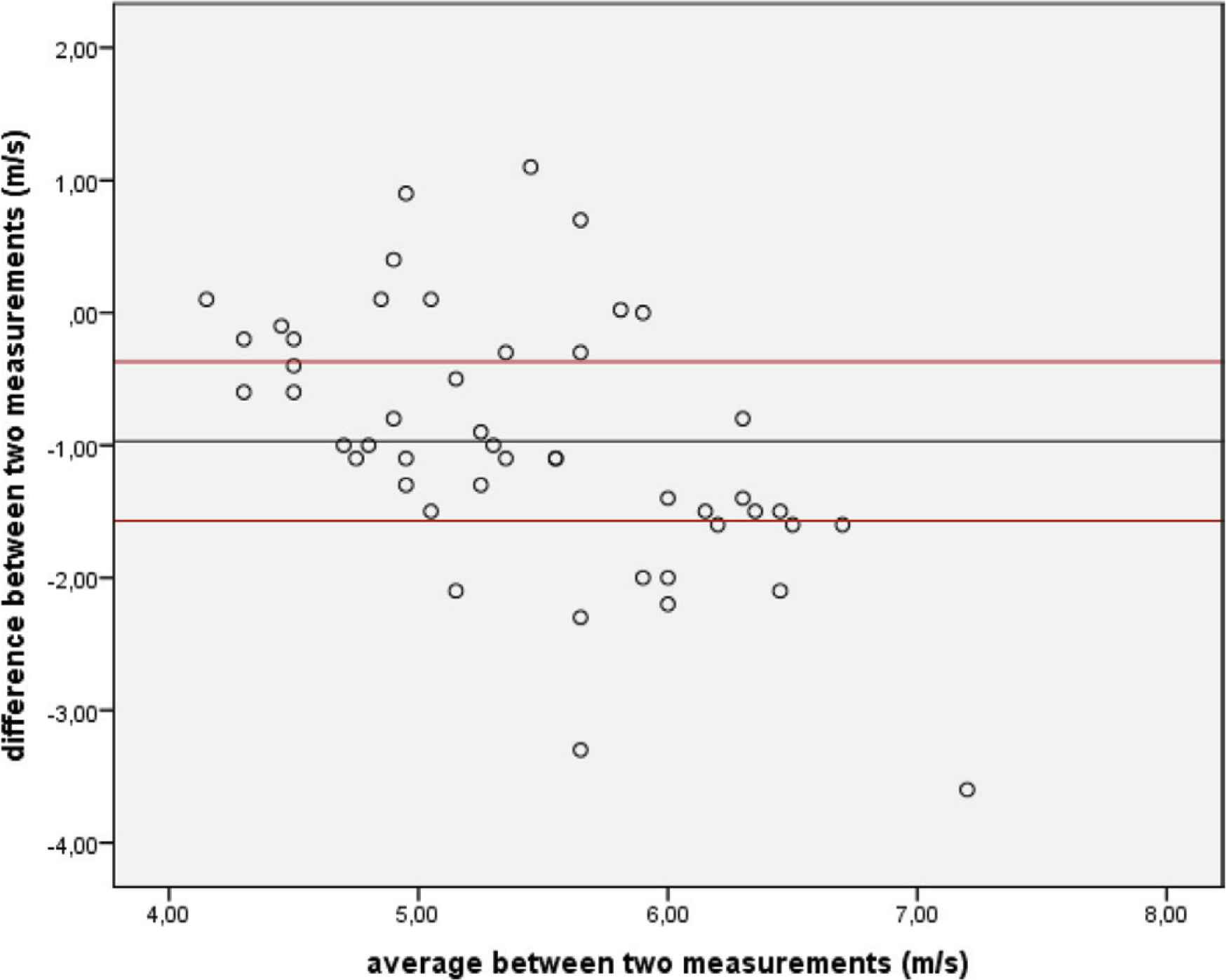
Bland and Altman plot for pulse wave velocity measurement performed carotid-femoral lying and carotid-radial sitting.
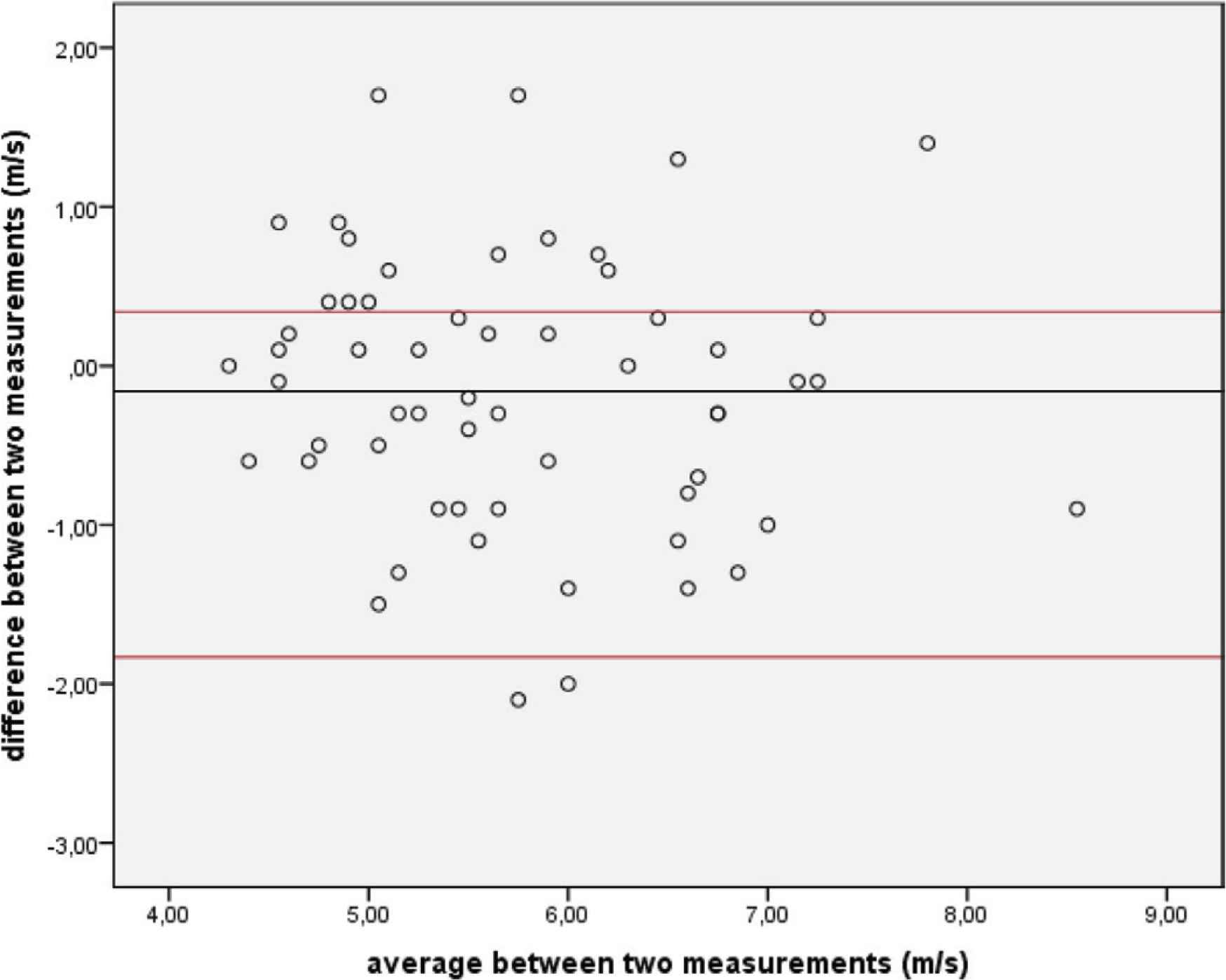
Bland and Altman plot for pulse wave velocity measurement performed carotid-radial lying and carotid-radial sitting.
Next, central hemodynamic data were analyzed with mean values, presented in Table 2. Analysis of central hemodynamic data showed statistically significant differences between subendocardial viability ratio (p = 0.001), end systolic pressure (p = 0.001) and central diastolic pressure (p = 0.001) when central hemodynamic data of carotid-radial measurements lying and sitting were compared, but there were no differences when the same parameters were compared between hemodynamic data of both lying positions, except for subendocardial viability ratio, where there was a statistical difference with p = 0.029. Other comparisons were statistically insignificant (Table 3).
| Parameter | Mean ± SD | Parameter | Mean ± SD |
|---|---|---|---|
| AIx75 cf | −21 ± 19 | ESP cr sitting (mmHg) | 103 ± 13 |
| AIx75 cr lying | −21 ± 17 | CSP cf (mmHg) | 114 ± 20 |
| AIx75 cr sitting | −17 ± 17 | CSP cr lying (mmHg) | 112 ± 12 |
| SEVR cf | 138 ± 27 | CSP cr sitting (mmHg) | 114 ± 16 |
| SEVR cr lying | 137 ± 28 | CDP cf (mmHg) | 91 ± 12 |
| SEVR cr sitting | 142 ± 26 | CDP cr lying (mmHg) | 89 ± 11 |
| ESP cf (mmHg) | 101 ± 14 | CDP cr sitting (mmHg) | 91 ± 11 |
| ESP cr lying (mmHg) | 99 ± 13 |
SD, standard deviation; Aix, augmentation index; SEVR, subendocardial viability ratio; ESP, end systolic pressure; CSP, central systolic pressure; CDP, central diastolic pressure; cf, carotid-femoral; cr, carotid-radial.
Mean values of central hemodynamic data obtained from different position measurements
| Pair | p-value | Pair | p-value |
|---|---|---|---|
| AIx75 cf and AIx75 cr lying | 0.541 | ESP cr lying and ESP cr sitting | 0.001 |
| AIx75 cf and AIx75 cr sitting | 0.460 | CSP cf and CSP cr lying | 0.869 |
| AIx75 cr lying and AIx75 cr sitting | 0.069 | CSP cf and CSP cr sitting | 0.411 |
| SEVR cf and SEVR cr lying | 0.477 | CSP cr lying and CSP cr sitting | 0.244 |
| SEVR cf and SEVR cr sitting | 0.029 | CDP cf and CDP cr lying | 0.305 |
| SEVR cr lying and SEVR cr sitting | 0.001 | CDP cf and CDP cr sitting | 0.090 |
| ESP cf and ESP cr lying | 0.110 | CDP cr lying and CDP cr sitting | 0.001 |
| ESP cf and ESP cr sitting | 0.179 |
Aix, augmentation index; SEVR, subendocardial viability ratio; ESP, end systolic pressure; CSP, central systolic pressure; CDP, central diastolic pressure; cf, carotid-femoral; cr, carotid-radial.
t-Paired test for central hemodynamic data
4. DISCUSSION
It is generally recommended that for children only pulse wave velocity measuring devices validated on pediatric population are used. Research conducted in the adult population cannot be generalized to pediatric studies [4]. The technique is being increasingly recognized and studied in the pediatric population. Many studies have demonstrated elevated pulse wave velocity in children with cardiovascular risk factors, such as hypertension or even only family history of hypertension, obesity, metabolic syndrome, diabetes, renal disease, congenital heart defect or heart transplant because of congenital heart disease, stress, smoking, sedentary lifestyle [14–16]. Low-birth weight also proved to be a risk factor, but was confirmed only when brachial-ankle pulse wave velocity was measured, not with the gold standard, carotid-femoral pulse wave velocity [4].
In the pediatric population, fundamental factors such as blood pressure and heart rhythm vary with age, making it difficult to interpret the results. In general, pulse wave velocity also increases with age in healthy children [17], with increasing blood pressure and lower heart rate. In addition, there are only few studies with a small number of patients for certain disease groups. Several authors believe that there is still a disagreement in the pediatric population regarding the technique of measuring and interpreting results, which expresses the need to standardize the method in children and to carry out research under a single protocol [4].
Carotid-femoral pulse wave velocity has long been considered the gold standard of measurement. In our study, we wanted to obtain the measurements at other sites, such as carotid-radial, which would be easier to perform in the pediatric population. This fact was also confirmed during the study, when we failed to perform carotid-femoral measurements in six subjects, while we did not have any problems with the carotid-radial pulse wave velocity regardless the position.
Measurements between carotid-femoral pulse wave velocity and carotid-radial pulse wave velocity (sitting or lying) are significantly different (p < 0.001), which leads to the conclusion that the measurement site is essential for interpretation of the results and therefore cannot be interchangeable. Also, a statistical bias in Bland and Altman plot can be observed between carotid-femoral pulse wave velocity and carotid-radial pulse wave velocity (sitting or lying). Additionally, the data shows that above an average value of 5.5 m/s, carotid-radial (lying or sitting) pulse wave velocity becomes higher then carotid-femoral pulse wave velocity. The fact could indicate that with higher pulse wave velocity (which could be interpreted as accelerated atherosclerosis) the differences between elastic properties of different arteries could be more pronounced. However, we should identify possible factors that would have an affect on the difference, such as age, sex, body mass index etc. A multivariate regression analysis has been made for our cohort, however, specific factors were not recognized.
A similar study has already been conducted in adults, where similar results were obtained – in addition to carotid-femoral and radial-femoral measurements, a femoral-posterior tibial measurement was also performed. Similar differences in measurement were found [18]. We found only one study in children comparing carotid-femoral pulse wave velocity and pulse wave velocity between the carotid and the toe. In this study, as in ours, a significant difference between the measured velocities was found [19].
We additionally wanted to check whether the position of the subject influences the measurement of pulse wave velocity, since the length of the arterial path can be minimally affected by changing the position. Using the paired t-test, no significant difference in the measurement of lying or sitting (p = 0.158) was revealed. For this part of the study, we used carotid-radial pulse wave velocity, since we do not have access to the femoral artery with the carotid-femoral pulse wave velocity in a sitting position. On the contrary, in healthy adult volunteers a similar study has been conducted and the results showed dynamic response with elevated pulse wave velocity during standing position, that lowered again when subjects were again in supine position. Authors assume, that this was the consequence of an increment in hydrostatic pressure in the abdominal aorta which with smaller radius propagates the pulse in a faster way and could play a role in the overall adaptation of the humans to gravitational stress [20].
Central hemodynamic characteristics, most importantly, systolic and diastolic blood pressures, are obtained during pulse wave analysis and are proven in adults to be more sensitive than peripheral blood pressure measurement when cardiovascular risk and pharmacological effects are evaluated [21,22]. Therefore, central hemodynamic data obtained from pulse wave velocity measurements were analyzed. Some differences in sub-endocardial viability ratio and central diastolic pressure were found between measurements lying and sitting, but not between both lying positions, which indicates a possible effect of the position on central hemodynamic data, less the site itself.
A major limitation of our study is primarily the number of subjects with a large age range. Next, the group of our subjects is diverse with different cardiovascular risk factors. To confirm our results, we should expand the study to include healthy children. They could also be divided according to age groups, since from a physiological point of view more comparable results could be obtained.
5. CONCLUSION
Several guidelines for pulse wave analysis and pulse wave velocity measurement were published for adults and children, mostly emphasizing carotid-femoral pulse wave velocity in supine position as the gold standard of measurement [4,23]. Our results confirm the importance of site and position of the measurement, though in different studies in children several approaches are used. We are encouraged that a simplified method could lead to a unified approach, but first, validation with the acquisition of reference values is essential.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
MM and NMV study conceptualization and writing the manuscript, MM data acquisition with measurements, formal analysis and writing (original draft), NMV provided patients for measurement, supervised the project, finalized the original draft.
All authors read and approved the final manuscript.
FUNDING
No financial support was provided.
ETHICAL APPROVAL
The study was approved by local ethics committee (UKC-MB-KME-25/19).
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Mirjam Močnik AU - Nataša Marčun Varda PY - 2020 DA - 2020/11/09 TI - Hemodynamic Data Analysis and Site of Measurement in Children and Adolescents JO - Artery Research SP - 20 EP - 24 VL - 27 IS - 1 SN - 1876-4401 UR - https://doi.org/10.2991/artres.k.201102.001 DO - 10.2991/artres.k.201102.001 ID - Močnik2020 ER -
