Liver Abscess in a Term Baby: A Case Report and Review of Literature
Peer review under responsibility of the Dr. Sulaiman Al Habib Medical Services Group Company
- DOI
- 10.2991/dsahmj.k.190521.001How to use a DOI?
- Keywords
- Diagnosis; liver abscess; management; newborn
- Abstract
Neonatal sepsis is common; particularly in preterm babies. However, it is uncommon for neonatal sepsis to present as localized liver abscess. Since 1930, less than 150 cases of liver abscess have been reported in the literature. The majority of initially reported cases were in term babies; while over the past two decades an increasing incidence in preterm babies has been reported. This is most likely due to increasing survival of preterm babies and associated increased use of invasive procedures (umbilical venous catheterization, and central venous lines) and the use of total parenteral nutrition. Apart from high index of clinical suspicion, an ultrasound (US) scan and computed tomography (CT) of the abdomen are required to confirm the diagnosis of liver abscess in a sick newborn baby.
- Copyright
- © 2019 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Liver abscess in the neonatal period is a rare disorder with potentially serious morbidity. The disorder can occur both in term and preterm babies. Newborn babies with lower gestational age, lower birth weight, invasive procedures (umbilical lines or central venous lines), immunodeficiency, and those on parenteral nutrition remain at higher risk [1]. The recent widespread and efficient use of bedside ultrasound (US) scans in the Neonatal Intensive Care Unit (NICU) have made it easy to rule in or rule out liver abscess in a baby with clinical features of sepsis and hepatomegaly. We report a case of liver abscess secondary to sepsis in a term neonate. The baby required surgical drainage with complete resolution. The relevant literature is also reviewed.
2. CASE REPORT
A 16-day-old term, male baby, birth weight 3.1 kg, was transferred to our NICU with sepsis. The Blood Culture and Sensitivity (C/S) was persistently positive for coagulase-negative staphylococci. He was born in the referring hospital by spontaneous vaginal delivery and admitted to their NICU due to meconium aspiration syndrome. He required ventilation for 1 week and an Umbilical Venous Catheter (UVC) was placed in the portal vein at birth. The UVC remained in this position for 6 days with Total Parenteral Nutrition (TPN) running through it. A chest drain was required for right pneumothorax. On admission to our hospital, he had hepatomegaly with raised C-Reactive Protein (CRP). Abdominal X-ray showed enlarged liver with high right-side diaphragm and a small 1 × 1 cm2 air bubble in the liver Figure 1. Abdominal US showed a heterogeneous multiloculated collection in the right liver lobe indenting the right hemidiaphragm, suggestive of liver abscess. Abdominal computed tomography (CT) showed a large multiloculated hepatic abscess with its main bulk in the right hepatic lobe with upper subcapsular extension causing right diaphragmatic elevation and showing multiple air loculi inside suggesting anerobic infection Figure 2A and 2B. The abscess was drained by an emergency laparotomy and an indwelling drain was placed. The C/S from pus was negative, while biopsy from the abscess wall showed nonspecific acute and chronic inflammation with granulation tissue. CRP gradually normalized, the drain was removed, and the baby recovered very well.
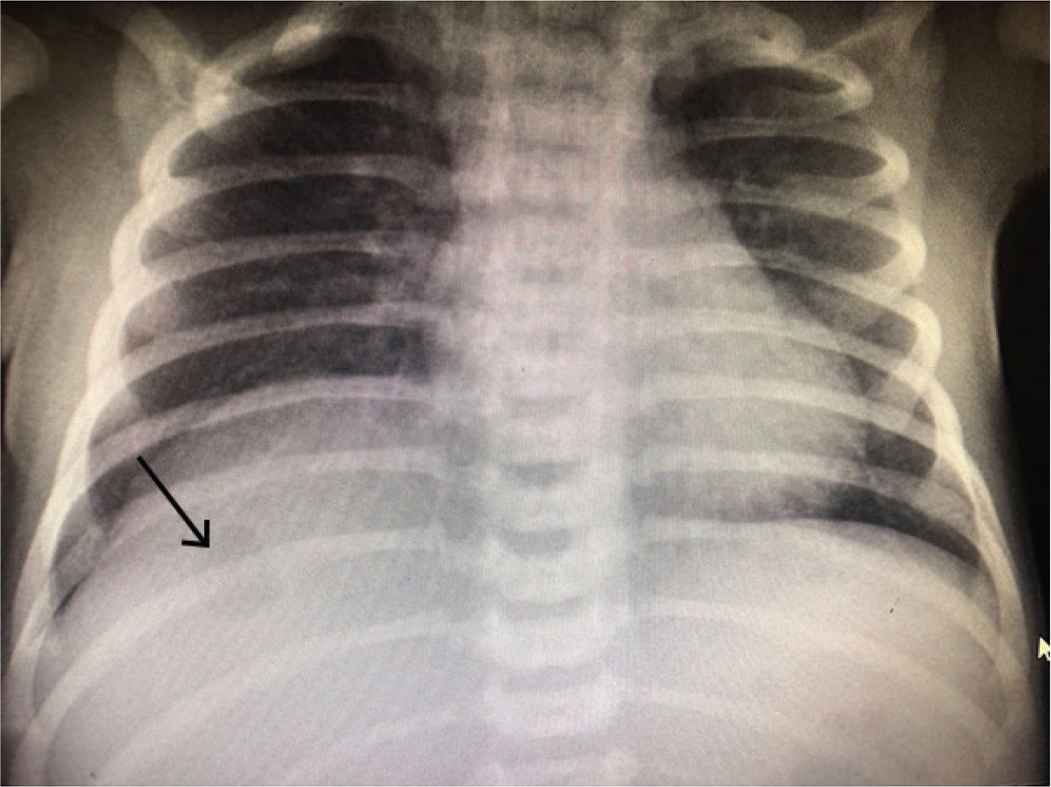
Thoracic and abdominal X-rays showing gas bubble in the liver.
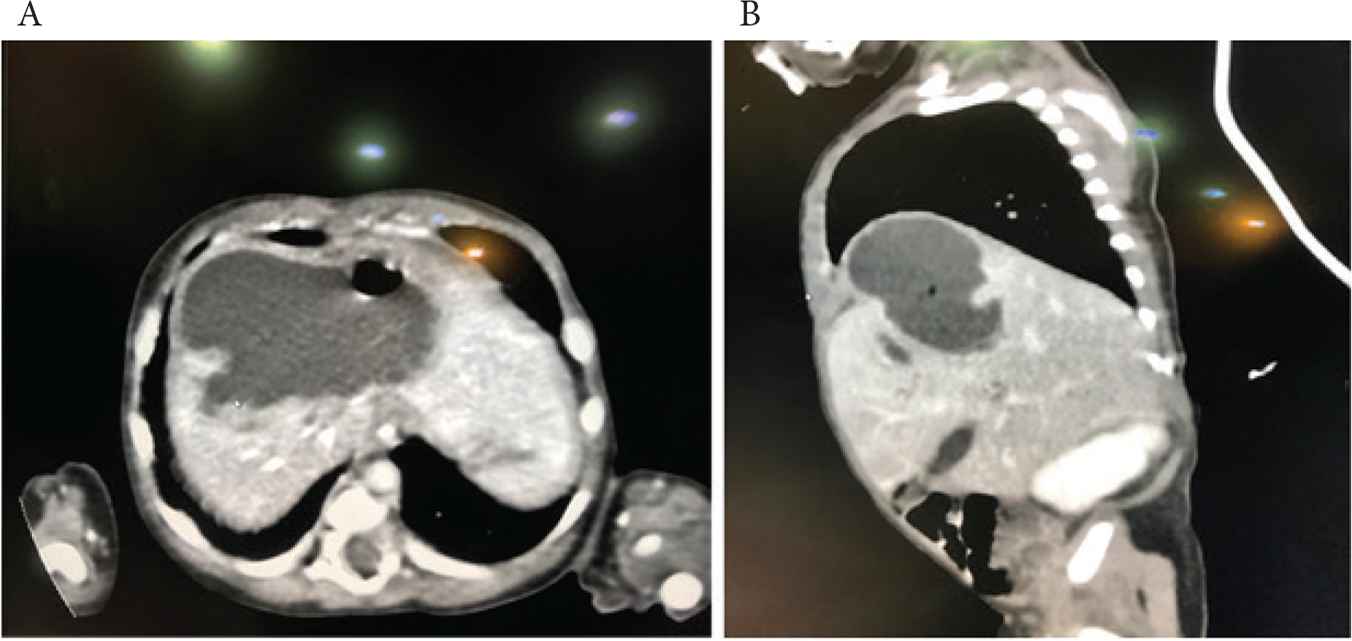
(A) Abdominal CT (horizontal view) showing large multiloculated hepatic abscess. (B) Abdominal CT (vertical view) showing large multiloculated hepatic abscess. CT, computed tomography.
3. DISCUSSION AND REVIEW OF THE LITERATURE
Neonatal liver abscess is a rare but serious disorder associated with high mortality and morbidity [1–5]. Tan et al. [4] reported six cases of neonatal liver abscess in 2005 and reviewed the incidence since 1930. They discovered fewer than 100 reported cases in the English-language literature between 1930 and 2005 [4]. Most of these cases were term babies. Between 2005 and 2013, 27 more cases were reported [3]; the majority of which were preterm babies [2,3]. This increase in incidence could have been due to increasing survival of preterm and low birth weight babies who have had UVCs, central lines, and TPN. The poor body defense mechanisms (immunodeficiency and neutrophil dysfunction) due to prematurity itself may also be a contributory factor. Other predisposing factors include central catheters used for TPN, necrotizing enterocolitis, umbilical sepsis, and gallbladder or liver surgery [4,5]. Chorioamnionitis and abruptio placentae are possible maternal risk factors [6]. The increasing use of portable US in the NICU and improved US skills of staff may have been instrumental in diagnosing these cases, which was not possible in the pre-US era.
The clinical presentation and laboratory findings of neonatal liver abscess are usually nonspecific; similar to those of generalized sepsis. Hepatomegaly and raised diaphragm on X-rays point towards a possible space-occupying mass in the liver. A high index of suspicion should always be raised in a baby with potential risk factors. Abdominal US is usually the first investigation that can detect, locate, and define a liver abscess [7]. US has a sensitivity of 80–90% in screening and diagnosis of neonatal liver abscess. US can also help in screening associated abscesses in other organs, such as spleen, kidney, and lungs. Being a low cost, noninvasive, mobile, and easily available instrument, US is useful for diagnosis and monitoring of response to treatment; both surgical and medical. Serial US done at frequent intervals during the course of the disease gives useful information on the progress of the healing process. US can also be used to guide percutaneous drainage of neonatal liver abscess. US findings of neonatal liver abscess may be similar to those of hepatoblastoma, infantile hemangioendothelioma, and hepatic hamartoma. Serum α-fetoprotein levels may be helpful in differentiating these malignant and benign hepatic masses from liver abscesses [2]. Abdominal CT (with and without contrast) gives a firm diagnosis and also defines the extent, structure (single or multiloculated), and any connections with the UVC or central lines. Typical CT appearance is that of a well-circumscribed, low-attenuation mass with a contrast-enhancing rim. Together, abdominal US and CT scan constitute the most sensitive diagnostic tests in the detection of neonatal liver abscess [8]. A raised diaphragm is the only useful sign on plain thoracic and abdominal X-rays. Our case was unusual because the clinical suspicion was raised after seeing a large gas bubble in the liver substance Figure 1. This could have been caused by a gas-producing organism, although pus culture was negative. This was not a surprise because, prior to surgery, our baby had received antibiotics for several days.
Neonatal liver abscess can be caused by a variety of organisms. Polymicrobial infection is found in up to 50% of abscesses [3]. The most common bacteria cultured from neonatal liver abscess are Staphylococcus aureus, Streptococcus pyogenes, Escherichia coli, Klebsiella spp., and Pseudomonas spp. [3,4]. Case reports of neonatal liver abscess caused by Corynebacterium acnes, anaerobic bacteria, and Candida spp. have also been published [5]. The microorganisms may enter the liver and produce an abscess by four possible mechanisms: (1) an ascending infection via the umbilical and portal veins; (2) hematogenous spread; (3) ascending infection via the biliary tract; and (4) by direct contiguous spread from neighboring organs [2–6]. TPN extravasation through a UVC tip sited in the liver substance can also cause necrosis and abscess formation. Our case had a UVC with TPN running through it for the first 6 days of life. He had persistent Staphylococcus epidermidis sepsis at the time of transfer to our hospital on day 16 of life. Although the liver abscess was sterile, we believe it originated from hematogenous spread. DeFranco et al. [9] described a similar case of a full-term neonate with a history of umbilical venous catheterization followed by coagulase-negative staphylococcal sepsis. The infant developed a solitary hepatic abscess with saprophytic organisms. Singh et al. [1] reported a similar case in a term baby at 1 month of age who had a pus culture positive for S. aureus. The blood culture in their case was negative; most probably due to previous antibiotic treatment.
Neonatal liver abscess may be a solitary abscess or multiple abscesses either confined to the liver or involving other organs (e.g., spleen, brain, and lungs). The incidence of multiple liver abscesses is higher than the incidence of a solitary liver abscess. These multiorgan abscesses are small, not drainable, not associated with umbilical infection, and have a fulminant course. A solitary liver abscess is usually large, either uni or multiloculated, well localized, and easily drainable. The solitary liver abscesses have been associated with TPN administration via UVC and usually run a subacute course [2].
Portal vein thrombosis, portal cavernoma formation, and portal hypertension are known complications of neonatal liver abscess [10–12]. Doppler US and CT with intravenous contrast usually confirm the diagnosis of these complications. Babies who develop portal vein thrombosis, should be followed up during the first 5 years of life with US and Doppler studies to look for development of portal cavernoma and portal hypertension. Neonatal portal vein thrombosis can be managed conservatively with intravenous low molecular weight heparin (enoxaparin) 1.5 mg/kg subcutaneously every 12 h. Singh et al. [11] reported successful conservative management of portal vein thrombosis in their case with enoxaparin with complete resolution and no long-term complications. Their case had multiple small liver abscesses that also resolved completely with conservative management with antibiotics.
The treatment of neonatal liver abscess consists of drainage by aspiration (closed or open) plus intravenous antibiotics as directed by the microbiology results. The recovery is usually full without any long-term morbidity.
Management of neonatal liver abscess needs a multidisciplinary approach. The predisposing factors (e.g., umbilical catheter/central line and immunodeficiency) should be removed. A single large abscess or multiple large abscesses will require either percutaneous drainage of the abscess (with or without US guidance), or open drainage of the abscess affecting multiple lobes of the liver and/or single large abscess [13]. Lee et al. [14] showed good long-term outcome of their neonatal hepatic abscess cases following imaging-guided aspiration or drainage. The main stay of conservative management is appropriate antibiotic therapy that should be directed against the causative agent in culture-positive cases. In culture-negative cases, broad-spectrum antibiotics covering Gram-positive, Gram-negative, and anaerobic organisms must be started. The treatment may require 3–6 weeks of intravenous antibiotics. However, the progress and success of treatment should be monitored by serial US scans and serial hematological investigations, including complete blood count, inflammatory markers (CRP and procalcitonin) and liver function tests.
Concomitant nutritional management is important. Most of the babies can be managed on full enteral nutrition. With prompt diagnosis and appropriate treatment, the outcome seems to be better. Unfortunately, the mortality rate still can be as high as 50% in spite of appropriate care and treatment [11].
In conclusion, neonatal liver abscess is rare. Invasive procedures and other risk factors in preterm babies have resulted in increasing numbers of reported cases in recent years. A high index of suspicion should be raised in a high-risk baby with resistant sepsis. Bedside US is usually enough for diagnosis. CT scan (with or without contrast) and Doppler studies can elaborate the extent of disease and possible complications. Surgical/US-guided drainage with appropriate antibiotics are curative in most cases, with good, complication free long-term outcome.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
Cite this article
TY - JOUR AU - Sajjad Ur Rahman AU - Abid Ghalib AU - Muhammad Hasan Abdulghani AU - Abdullah Jan PY - 2019 DA - 2019/06/30 TI - Liver Abscess in a Term Baby: A Case Report and Review of Literature JO - Dr. Sulaiman Al Habib Medical Journal SP - 27 EP - 29 VL - 1 IS - 1-2 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.190521.001 DO - 10.2991/dsahmj.k.190521.001 ID - UrRahman2019 ER -
