Intensive Care Unit Patients’ Perception of Sleep Quality and Factors of Sleep Disruption: Cross-sectional Study
Peer review under responsibility of the Dr. Sulaiman Al Habib Medical Services Group Company
- DOI
- 10.2991/dsahmj.k.190530.001How to use a DOI?
- Keywords
- ICU; noise; pain; sleep deprivation; sleep disturbance; sleep quality
- Abstract
This study aimed to identify the etiologies of sleep deprivation among patients in the Intensive Care Unit (ICU). Sleep deprivation is a common problem that patients face while they are in the ICU. Poor sleep quality has several consequences such as weakening the immune system, irregular sleep cycle, and delirium. A cross-sectional study using self-administered questionnaire was performed in three medical–surgical ICU of tertiary teaching private hospitals. A modified version of sleep quality questionnaire developed by Freedman and colleagues was used to collect data from ICU patients. The questionnaire required patients to rate their overall sleep quality on a 10-point scale. A total of 30 patients participated in the study, and results showed that they perceived their overall sleep quality at home and the ICU at almost the same level. Findings also showed no differences in patients’ sleep quality during daytime and nighttime as well as during their 1st night, middle of their stay, and toward the end of ICU stay. Heart monitor alarms were perceived by the patients as the most disrupting noise in the ICU. Statistically significant differences were detected between gender and overall sleep quality (p = 0.001), daily activities (p = 0.003), and noises (p = 0.0005). Patients who had been in the ICU for 4–7 days were found to have a statistically significant poorer sleep quality compared with other patients. Multifactorial causes, including environmental and nonenvironmental factors, can result in sleep disruption among ICU patients. Interventions and strategies should be developed to minimize sleep disruption and improve the quality of care provided to ICU patients.
- Copyright
- © 2019 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
There are several causes of sleep deprivation, which is a common problem among patients in the Intensive Care Unit (ICU) [1]. Cicek et al. [2] conducted a study in Coronary Intensive Care Units (CICU) on 100 patients using Freedman et al.’s sleep quality questionnaire. The results showed that lighting, nurses’ intervention, and drawing of blood samples are the most disruptive activities in the CICU. Naik et al. [3] conducted a cross-sectional study using Richards–Campbell sleep questionnaire, and results showed poor sleep quality in 15 of the 32 patients included in the study. They also showed that age, patient’s physiology, and chronic health were related to sleep quality. Meanwhile, Zhang et al. [4] conducted a cross-sectional study using the Pittsburgh sleep quality index on 152 thoracic surgery patients in the ICU; they reported that around 46.1% of the patients reported poor sleep quality.
Richardson et al. [5] conducted a study among ICU patients. The patients were divided into two groups: the intervention and the nonintervention groups; the intervention group had to wear earplugs and eye masks while sleeping. Patients in both groups reported noise as a major source of disturbance while sleeping in the ICU. They also noted that environmental and intrinsic factors were the major reasons for sleep deprivation [1]. Critically ill patients experienced difficulty in going into deep sleep because of pain and medications [1]. New studies have found that sleep deprivation had an impact on circadian rhythms along with reduction in sleep quality and depth [6]. Ding et al. [7] conducted a study investigating the factors of sleep disturbance. The participants were 24 medical staff and 14 patients. The results showed that sleeping more than one night in the ICU would negatively impact sleep quality. Bihari et al. [8] conducted a study on 100 patients using a modified version of Freedman et al.’s sleep quality questionnaire. The results showed that sleeping in the ICU was affected by many factors, and the etiology of disturbance is multifactorial; however, noise was the most common reason reported by patients.
Freedman et al. [9] conducted a study on 203 patients confined in the ICU. The self-report questionnaire was developed to assess the etiology of sleep deprivation among ICU patients. Results showed that vital signs test was significantly the major cause of disturbance [9]. There are several methods used to measure sleep deprivation such as polysomnography, actigraphy, and other subjective methods [10]. However, several studies have concluded that the deep sleep stage is absent while patients were in the ICU, which had a negative effect on neurocognition, hormone changes, and immune system [10]. The factors of sleep deprivation are unspecific, and previous studies have shown several causes of poor sleep quality in the ICU [11]. Previous studies showed that only 14% of procedures in the ICU were completed without rousing sleeping patients [12]. A study was conducted on 293 ICU patients who were divided into two groups to determine if nurses’ interventions affected the patients’ sleep. Results showed that patients who did not receive any intervention had a better sleep quality [13]. Additionally, pain, illness, anxiety, and fear were cited as factors of sleep deprivation in the ICU [14,15].
The total number of healthy sleep hours in adults was 7–8 h [6]. The prevalence of sleep disturbance among ICU patients was high, and 55.63% of the total sleep time happened at night [3]. Moreover, approximately 24–90% of patients in the ICU reported experiencing sleep problems [4]. Meanwhile, the prevalence of delirium among ICU patients ranged between 11% and 80% [16]. Furthermore, sleep deprivation had a negative impact on vasoconstriction; it could raise the diastolic blood pressure [1]. Weakening of wound healing and the immune system are some of the physiological consequences of sleep deprivation [2]. It can also negatively affect memory, attention, and response time [10]. Approximately 67% of 329 patients who were interviewed after discharge from the ICU reported high alteration in sleep [17]. This study aimed to find the etiology of sleep deprivation among patients in the ICU.
2. DESIGN
A cross-sectional study using a self-administered questionnaire was used on conscious patients admitted to three ICUs at Dr Sulaiman Al Habib hospitals (Dr Sulaiman Al Habib Medical Group is the largest healthcare services provider in the Middle East). The ICUs are tertiary adult medical and surgical ICUs. The hospitals are teaching hospitals, and their ICUs have a bed capacity of 35, 23, and 21 beds. There are more than 3628 medical and surgical admissions per year in the three ICUs. Each patient in the ICU is provided with a private room, and the nurse/patient ratio is 1:1. All patients admitted in the ICUs are remotely monitored by an expert critical care team in a tele-ICU command center. Only adult conscious patients who were admitted in the ICU for more than two nights were eligible for inclusion in the study. This was intended to allow time for the patients to experience the ICU environment. Patients also had to be oriented to the place and time during the data collection period.
2.1. Questionnaire
This study aims to find the etiology of sleep deprivation among patients in the ICU using a modified version of Freedman et al.’s [9] sleep quality questionnaire. Modifications have been made by Bihari et al. [8] to add pain to the factors of sleep deprivation Table 1. The modified version of the sleep quality questionnaire was translated into Arabic and then translated back into English for comparison; next, it was tested on a group of adults to ensure understanding of the questions and clarity of the scale points. The demographic details of the tool included age, gender, diagnosis, and Length of Stay (LOS). The developed questionnaire required patients to rate their overall sleep quality on a 10-point scale (ranging from 1 to 10). Patients were asked to rate their sleep quality at home, overall quality of sleep in the ICU, and overall quality of sleep on specific days (where 1 = poor and 10 = excellent). In addition, patients were asked to rate the overall quality of sleep during daytime and on specific days during their stay (1 = unable to stay awake, 10 = fully alert and awake). Finally, patients were asked to rate environmental factors in the ICU during their stay (1 = no disturbance, 10 = significant disturbance).
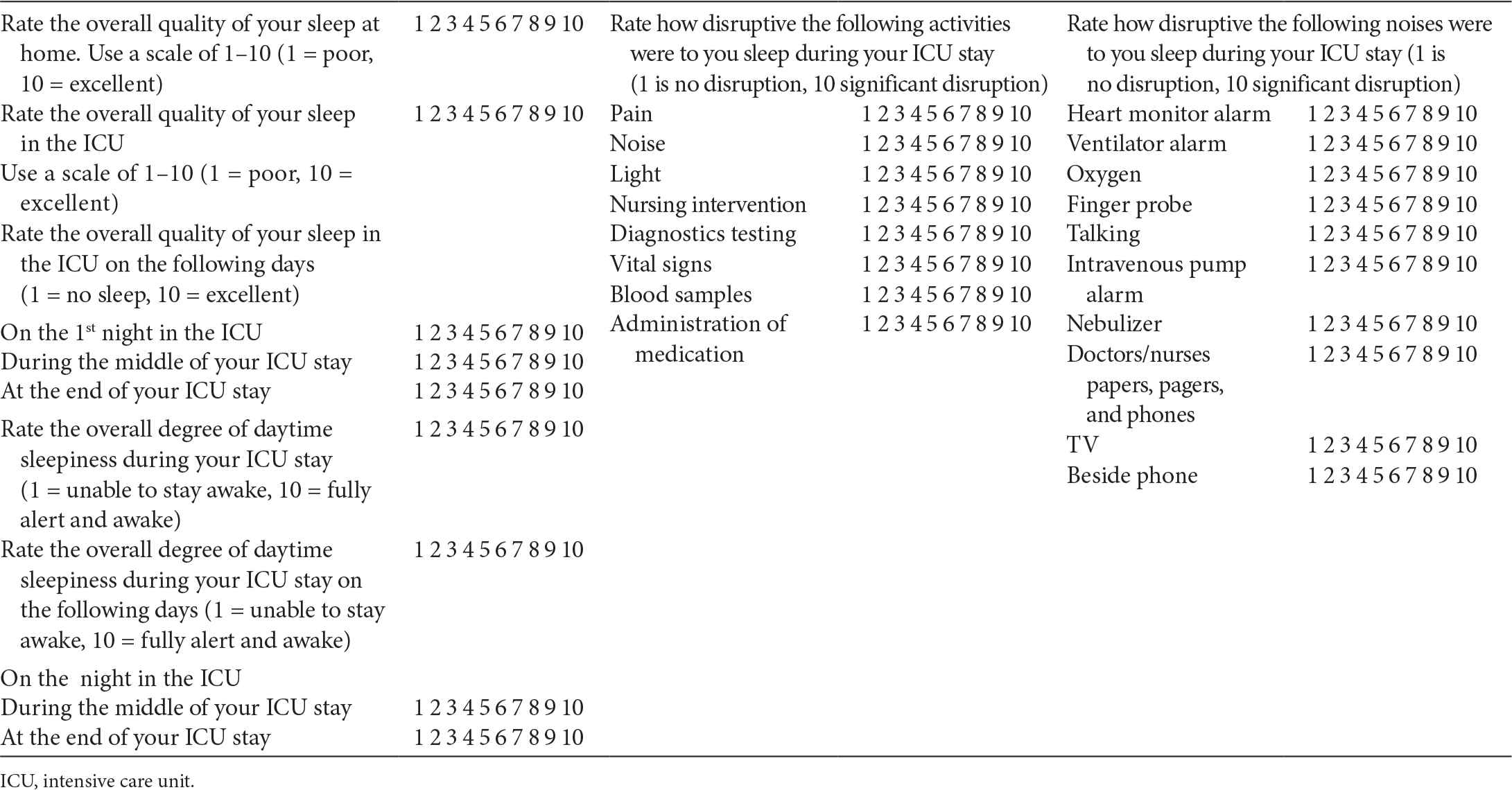
Modified version of Freedman’s sleep quality questionnaire
2.2. Ethical Consideration
The study was conducted after obtaining approval from the Dr Sulaiman Al Habib Medical Group Institutional Review Board (RC18.11.22). The anonymity and confidentiality of participants were ensured in this study. No name or personal identifying information was written on the questionnaire or in the demographic sheet. Participation in the study was voluntary, and consent was implied by participation. All participants had the right to voluntarily participate in the study without adverse consequences and were provided with a full description of the nature of the study. Participants were assured that they had the right to withdraw from the study at any time without any questioning.
2.3. Data Analysis
The data was first entered into an Excel spreadsheet and then exported to an SPSS spreadsheet. A random check for the variables was used to detect any mistakes during the data entry process. Both descriptive and inferential statistics were conducted using IBM SPSS Statistics for Windows, (Version 24.0. Armonk, NY: IBM Corp; 2016). The demographic data were summarized using descriptive statistics. Tables of frequencies, percentages, and bar charts were produced using the Frequencies command. Inferential statistics were used to build judgments of the probability that an observed difference between groups had a high probability of recurrence in the population that the sample represented and that it did not happen by chance.
3. RESULTS
A total of 30 patients completed the questionnaire Table 2. The patients’ mean age was 37.15 ± 17.34 years; the youngest among was 16 years old and the oldest was 76 years old. Duration of stay in the ICU ranged between 3 and 7 days. Of all patients, 17 (56.7%) were male and 13 (43%) female. As indicated in Figure 1, patients perceived their overall sleep quality at home and the ICU as almost the same (6.4 and 6.8, respectively).
| Characteristics | Categories | Frequency (%) |
|---|---|---|
| Age | Mean (SD) | 37.15 ± 17.34 |
| Min | 16 years | |
| Max | 76 years | |
| Gender | Male | 17 (56.7%) |
| Female | 13 (43%) | |
| Length of stay in ICU | 1–3 days | 15 (50%) |
| 4–7 days | 12 (40%) | |
| >7 days | 3 (10%) |
ICU, intensive care unit; SD, standard deviation.
Sociodemographic of study population (n = 30)
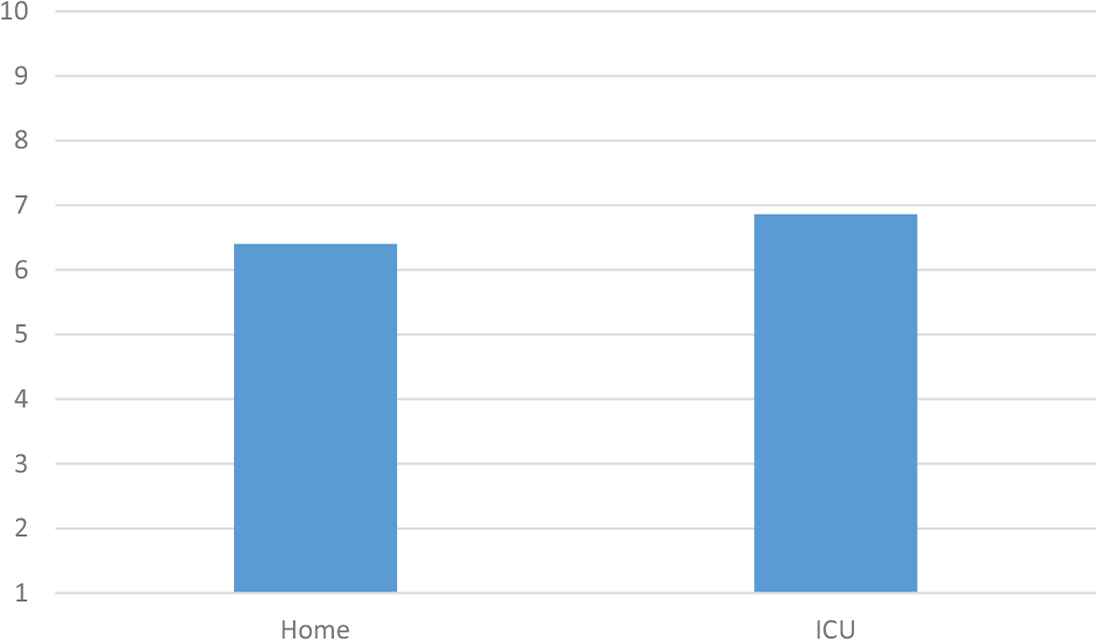
Patients’ perceived sleep quality. ICU, intensive care unit.
The patients’ self-reported sleep quality during their stay in the ICU showed no differences. As illustrated in Figure 2, patients perceived sleep quality as almost similar during their 1st night, middle of their stay, and toward the end of ICU stay. The same applies to the patients’ sleep quality during daytime in the ICU (see Figure 3). Activities including noise, light, nursing interventions, diagnostic testing, vital signs measurement, blood samples, and administration of medications were rated slightly similar as the etiology of sleep disruption over the course of their stay in the ICU Figure 4. Among the noises cited, heart monitor alarms were perceived by the patients as the nosiest cause of sleep disruption Figure 5.
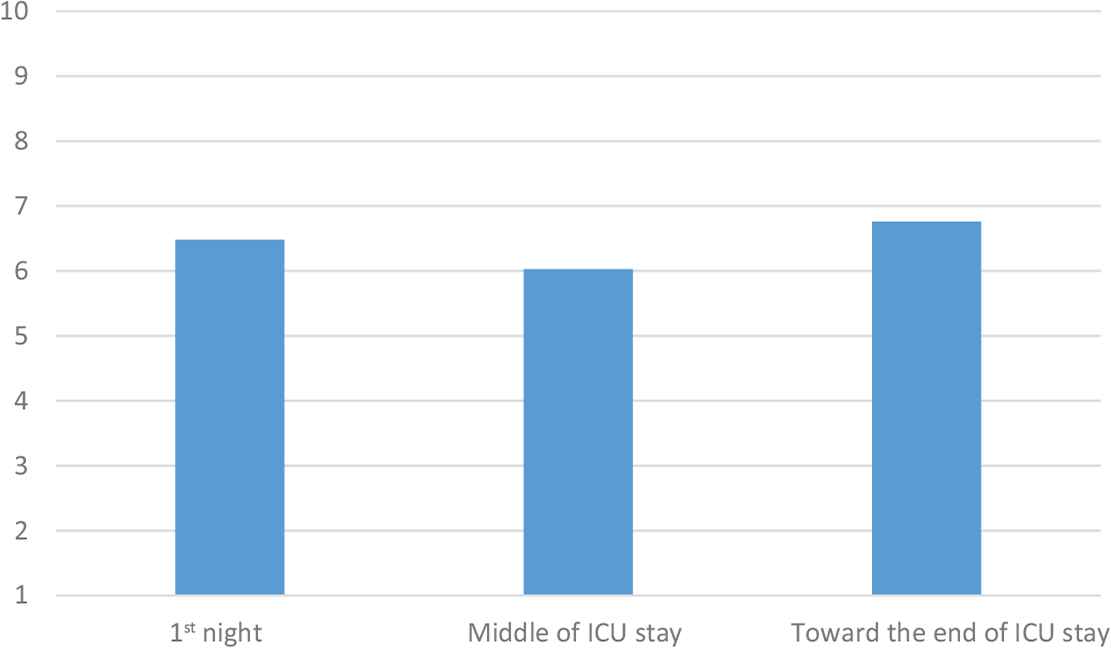
Sleep quality in intensive care unit (ICU).

Daytime sleep in intensive care unit (ICU).

Disruption in sleep.
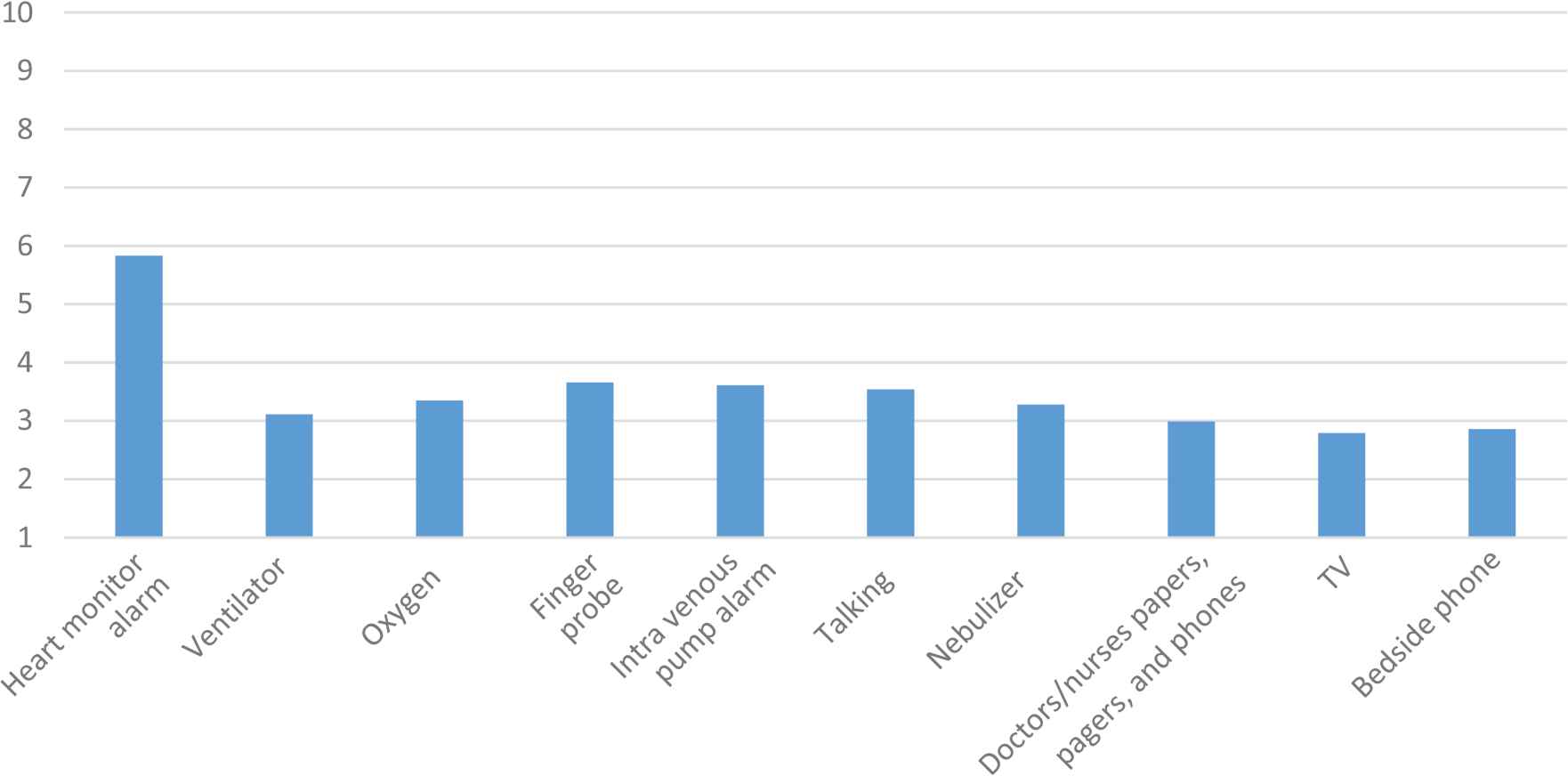
Disruption in sleep: noises.
There was a significant difference between individual gender (p = 0.001) in terms of sleep quality in the ICU. Male patients recorded more sleep disruptions than their female counterparts. In Figure 6, the bar graph highlights the perceived sleep disruption activities by gender. There was a statistically significant difference between gender and overall disruptive activities. Male patients perceived the activities as more disruptive compared with female patients. In Figure 7, the bar graph highlights the perceived sleep disruption noises by gender (p = 0.003). There was a statistically significant difference between gender and disruptive noises. Male patients regarded these noises as sleep disruptive more than female patients did.

Perceived sleep quality by gender. ICU, intensive care unit.

Perceived sleep disruption activities by gender.
In Figure 8, the bar graph highlights the perceived sleep disruption noises by gender. There was a statistically significant difference between gender and disruptive noises (p = 0.0005). Male patients regarded noises as sleep disruptive more than female patients did. Meanwhile, Figure 9 shows sleep quality in the ICU in terms of the patients’ LOS. A statistically significant difference was found in patients who had been in the ICU for 4–7 days. Patients in this group were found to have poorer sleep quality in comparison with other groups.
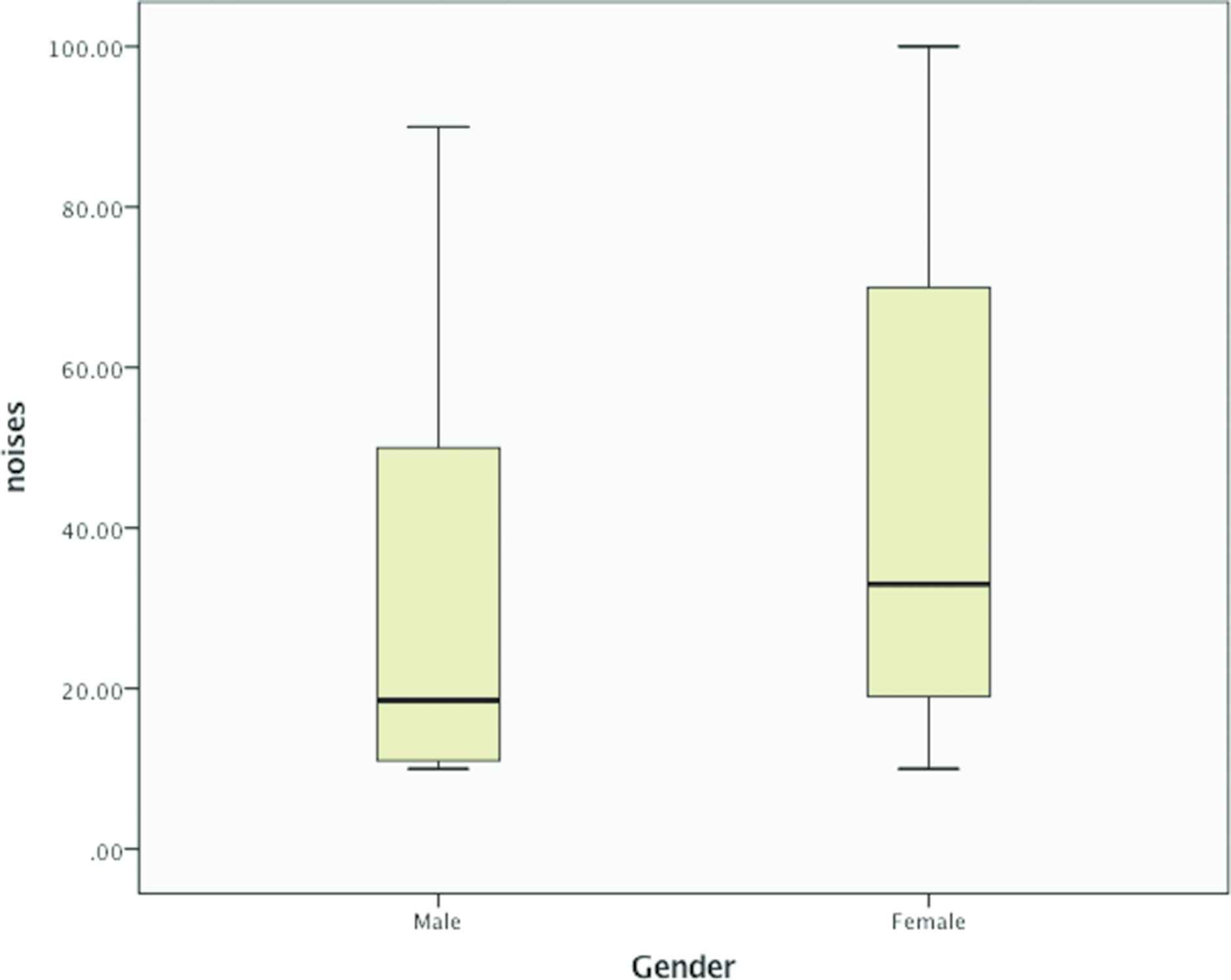
Perceived sleep disruption noises by gender.

Perceived sleep quality by patients’ length of stay. ICU, intensive care unit.
4. DISCUSSION
This study aimed to identify the sleep disturbance etiology among ICU patients using a self-administered questionnaire. This study, which was conducted in three ICUs of tertiary private hospitals in Saudi Arabia, found no difference between sleep quality at home and ICU. These findings support the assertion that there is no difference in sleep quality at home and in the ICU as perceived by patients. Many reasons may explain why the current findings did not find any difference in sleep quality between home and the ICU. All patients in the participating ICUs were admitted in private rooms, which may have provided a quiet environment and a better sleep quality. There were also other methodological factors, such as the fact that this phenomenon was measured subjectively in a small sample size in contrast to other studies which found that patients admitted in the ICU experienced poorer sleep quality compared to sleeping at home [8].
Existing literature indicated that there were no significant differences between daytime and nighttime sleep in the ICU, as per the study conducted by Freedman et al. [17] on 24 ICU patients using polysomnography. Moreover, our results also found no discrepancies between daytime and nighttime sleep. An average of more than 6 points was scored by the patients in the survey, indicating more than moderate sleep quality on both daytime and nighttime sleep quality scale. An explanation for the current result is that all participants were conscious and fully oriented patients, which did not allow the detection of specific difference between daytime and nighttime sleepiness among ICU patients. In the work of Freedman et al. [9], factor analysis showed that daytime sleepiness was significantly different in ventilated and nonventilated patients. In that study, ventilated patients were found to experience more daytime sleepiness compared with nonventilated patients.
There is a high level of agreement among patients that pain was the single biggest factor that disrupted their sleep in the ICU followed by noise. Other activities, which also received less than 5 points, included light, nursing interventions, diagnostic testing, vital signs, blood samples, and administration of medications. By contrast, in the study conducted by Elliott et al. [18], pain received a low score (less than 2/10). Moreover, patients in their study ranked noise and light as the most sleep disruptive factors in the ICU. Pain and noise negatively influenced the patients’ perceptions, disrupted their physiological and psychological balance, and consequently disrupted their sleeping patterns [18]. Pain, if not managed, negatively affects the cardiovascular stimulation, suppresses the body’s response to infection, and destroys the quiet and pleasant environment [18].
Among the noises identified in the survey, heart monitor alarms were ranked as the highest disrupting noise in the ICU. The alarms associated with audio and visual technological advances used to trace the circulatory and respiratory functions of ICU patients caused sleep disturbance. Erol and Enc [21] reported that 30% of the environmental noises in the ICU are caused by alarms. Patients’ sleep can be affected by environmental noises [20]. In previous studies, noise was reported as the most disturbing factor among ICU patients [21]. In these studies, patients’ sleep was disrupted mainly because of the noise produced by alarms in the equipment attached to monitor the patients. However, it should be noted that the patients in the current study were remotely monitored through tele-ICU command center, which decreased the disruption. Tele-ICU allows the staff to perform multiple tasks in the tele-ICU environment with less noise and without distracting the ICU patient’s sleep [22].
Patient age in this study was not related to sleep quality and sleep disruptive activities and noises (p > 0.05). These findings are not consistent with previously reported findings, where older patients were more likely to complain of disruptions compared with younger individuals [9]. By contrast, Bihari et al. [8] found that older patients had better sleep quality in the ICU than younger patients. Yet, the mean age of the study sample was 37.15 ± 17.34 years, with a small convenience sample, which did not include a sufficient number of younger patients to show a significant association between ICU patients’ age, sleep quality, and sleep disrupting factors.
When participants were analyzed according to gender, the results showed that male patients had poorer sleep quality in the ICU compared with female patients (p = 0.001) Figure 6. Males also perceived various activities as more disruptive than their female counterparts (p = 0.003). Moreover, male patients were more likely to consider noises as disturbing than female patients did (p = 0.0005). This might be related to the diagnosis of male patients even though it was not recorded in the current study. Another anticipated explanation was pain; male patients had less tolerance to pain compared with female patients. Pain, as reported in a number of previous and present studies, was rated by ICU patients as one of the most disturbing factors during their stay.
Findings of the current study should be interpreted by taking full account of its limitations. The study subjectively assessed sleep quality among ICU patients using Freedman et al.’s [9] sleep quality survey. Another limitation is the recruitment and selection bias of the study sample. Only patients who were in the ICU for at least three nights and were fully conscious were invited to participate in the study. As a result, it was difficult to recruit a larger sample, and only 30 participants were recruited. It should also be considered that the small convenience sample size is another limitation of the present study. Additionally, Freedman et al.’s [9] sleep quality questionnaire has not been fully validated to identify the ICU patients’ true sleep disruption caused by various factors.
5. CONCLUSION
Sleep disruption is very common among patients admitted in the ICU. It is multifactorial and can be attributed to environmental and nonenvironmental factors. Knowledge about the etiology of sleep disturbance among ICU patients helps as we strive to design interventions and strategies to minimize these disruptions, and can improve the quality of care provided to patients during their stay in the ICU. Further studies are required to examine whether sleep disruption among ICU patients is associated with increased mortality and other adverse outcomes and complications.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
Cite this article
TY - JOUR AU - Abbas Al Mutair AU - Abbas Shamsan AU - Adel AlFaqiri AU - Awad Al-Omari PY - 2019 DA - 2019/06/06 TI - Intensive Care Unit Patients’ Perception of Sleep Quality and Factors of Sleep Disruption: Cross-sectional Study JO - Dr. Sulaiman Al Habib Medical Journal SP - 30 EP - 35 VL - 1 IS - 1-2 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.190530.001 DO - 10.2991/dsahmj.k.190530.001 ID - AlMutair2019 ER -
