Can pervasive sensing address current challenges in global healthcare?
- DOI
- 10.1016/j.jegh.2011.11.005How to use a DOI?
- Keywords
- Global healthcare; Technology; Pervasive sensing; Ageing; Chronic disease
- Abstract
Important challenges facing global healthcare include the increase in the number of people affected by escalating healthcare costs, chronic and infectious diseases, the need for better and more affordable elderly care and expanding urbanisation combined with air and water pollution. Recent advances in pervasive sensing technologies have led to miniaturised sensor networks that can be worn or integrated within the living environment without affecting a person’s daily patterns. These sensors promise to change healthcare from snapshot measurements of physiological parameters to continuous monitoring enabling clinicians to provide guidance on a daily basis. This article surveys several of the solutions provided by these sensor platforms from elderly care to neonatal monitoring and environmental mapping. Some of the opportunities available and the challenges facing the adoption of such technologies in large-scale epidemiological studies are also discussed.
- Copyright
- © 2012 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/)
1. Introduction
Several trends are influencing global healthcare leading to rapid changes in both the development and adoption of new technology. These trends need to be studied carefully whenever new health policies are introduced, especially for developing markets in both developed and developing countries. Escalating costs of healthcare highlight the importance of managing resources with a better focus on system performance and patient well-being. Urbanisation closely linked to industrialisation means the dramatic rise of city populations worldwide, especially in developing countries, leading to higher rates of many blood-born, infectious and pollution-related diseases [1]. The access to better treatments for patients in urban areas, on the other hand, leads to a drop in several other areas. Coupled with this, in almost every country in the world, the proportion of people aged over 60 is growing faster than all other age groups. Although this can be seen as a success of modern healthcare, it challenges the society to adapt quickly in order to improve life-long health and well-being and overall health of the elderly, enabling them to lead an independent and active life.
Consumer-driven healthcare plans in the developed world, combined with wireless/mobile solutions and a growing use of web-based platforms have enabled better access to healthcare data for both patients and clinicians. However, these solutions highlight their own problems of scalability, security and privacy. Despite significant advances in medical devices, current monitoring tools are only able to provide a snapshot of a person’s physical parameters rather than offering a continuous view of his/her wellbeing. In most cases, detailed monitoring only takes place during a person’s stay in a hospital or clinic. Recent advances in sensors and embedded computing technologies have led to miniaturised sensor networks that can be worn or integrated within the home environment without affecting the person’s lifestyle or daily activities. Fig. 1 shows examples of the evolution of computers from large to miniaturised wearable and implantable devices. Integrated micro-sensors with on-board processing and wireless data transfer are the basic components of such networks already in existence. Extensive research has been directed to bio-sensor design, interfacing and bio-compatibility, wireless communication, ultra-low power processing, power scavenging, autonomic sensing, and integrated wireless sensor micro-systems leading to pervasive systems. Using the body as the media and a source of inspiration, energy to provide long-term continuous sensing and monitoring is the main driving force behind the current development of body sensor networks (BSN) [2]. These sensors have provided new means of addressing the following challenges tackling some of the global health challenges:
- •
Remote and continuous monitoring of the progress of chronic and infectious diseases.
- •
Observing post-operative patients at home allowing earlier release from hospital, reducing costs and providing efficient 24-hour monitoring.
- •
Understanding ageing and providing novel techniques for elderly care management.
- •
Large-scale monitoring of environmental changes and the impact of urbanisation.
- •
Providing innovative techniques for maternal and neonatal care after birth.
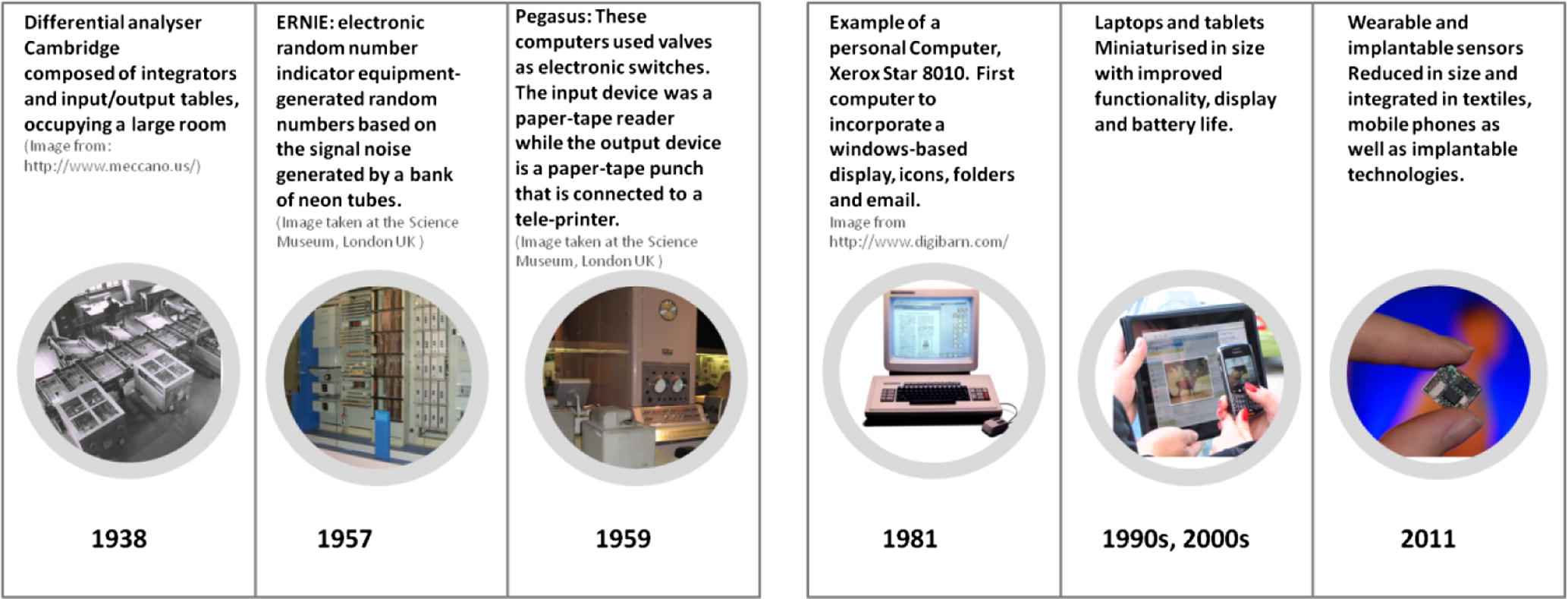
Examples of the evolution of computers over time from large computers to wearable and implantable devices.
This article will highlight several challenges facing global healthcare, then focus on pervasive technologies that can address some of the challenges posed. Finally, some of the issues that may arise when new technologies are adopted that influence patient health and well-being will be discussed, as well as opportunities for the application of pervasive sensing within epidemiological studies. Table 1 summarises some of the challenges discussed, their requirements and the sensing solutions proposed.
| Global health challenge | Requirements | Current systems | Pervasive healthcare |
|---|---|---|---|
| Chronic diseases Post-operative recovery Activity measurement |
Physiological parameters Activity measurement/feedback Sleep assessment |
Snapshot measurement Surveys/observations Personal feedback/surveys |
Continuous monitoring Activity/energy expenditure Pervasive sensors for sleep quality Intelligent data mining over time |
| Falls and elderly care | Fall detection/fall risk assessment | Pendants with push-buttons Clinic visits/surveys Clinical observations |
Automatic fall detection Wearable sensors for balance/stability |
| Rehabilitation | Encouraging activity Measuring performance |
Attending rehab clinics Clinical observation |
Remote rehabilitation monitoring Sensors for quantifying performance |
| Maternal and neonatal care | 24-Hour monitoring of neonates | Clunky uncomfortable sensors | Miniaturised sensors embedded in clothes/surroundings Minimal disruption to neonates |
| Environmental monitoring | Long-term monitoring Detecting changes |
Satellite/radar systems Automatic image analysis |
Miniaturised environmental sensors Intelligent event detection |
Several challenges facing global healthcare, requirements and solutions that can be provided by pervasive sensing.
2. Global challenges in healthcare
2.1. Chronic and infectious diseases
Chronic diseases, including heart disease, cancer, respiratory diseases and diabetes are the leading cause of death worldwide. The major risk factors associated with these diseases include smoking, alcohol, physical inactivity, obesity and a poor diet. By eliminating major risks, it is expected that around 75% of heart disease, stroke and type 2 diabetes and 40% of cancer would be prevented.1 In addition to chronic diseases, infectious diseases are also a significant burden on global economies and public health. Emerging infectious disease events have risen significantly and many events are dominated by zoonosis, and are influenced by socio-economic, environmental and ecological factors. A study by Jones et al. [3] concluded that global resources to counter disease emergence are poorly allocated, with the majority of the scientific and surveillance effort focused on countries from where the next important emerging infectious disease is least likely to originate. This highlights the need for coordinated global approaches to preventing and controlling complex infectious disease problems.
2.2. Ageing populations
The demographic shift associated with the ageing population is another major healthcare challenge. The United Nations world population report highlights the current rates of population ageing which are unprecedented in human history. This is mainly caused by declining fertility and mortality rates. The young/old balance is shifting throughout the world. Although the proportion of octogenarians is higher in more developed regions, most countries share an increase in old-age dependency ratio where the elderly are supported by a relatively smaller number of potential contributors. Labour-force participation among the older population has been declining worldwide, although the rates remain higher in the less developed than the more developed countries. The rapid increase in elderly rates builds a strain on most existing systems, so do diseases that are considered typical of elderly populations, including osteoarthritis, diabetes mellitus and hypertension. Elderly people are also generally susceptible to bronchitis, osteoporosis and heart disease. Common risk factors are obesity, diabetes, hypertension and various cardiovascular disorders [4].
Encouraging the elderly to continue to participate in their societies with dignity and security, despite having chronic conditions in some cases, is a challenge which is faced by healthcare systems and policy makers worldwide. Another challenge is that of falls which are the leading cause of injury and death among the elderly [5]; 4 out of 7 falls are fatal in persons over 70. Post-fall injuries can trigger a rapid decline in health and increase the risk of elderly death. Thus, fall-risk assessment before a fall occurs could be of great help in avoiding such scenarios.
2.3. Urbanisation and environmental impact
Most of the world’s population now lives in cities. In theory, living closer to health providers in cities should lead to better access to medications and treatments. However, this is not always the case in many countries around the world. The link between urbanisation and health problems is perhaps more evident in developing countries like India, China and Brazil where changes are occurring at an unprecedented pace. Cities are becoming hubs for infectious disease transmission, mainly because of high population densities as evidenced by recent disease pandemics [6]. Rapid urbanisation also increases mortality rates from diseases linked to lifestyle changes, such as cancer and cardiovascular diseases [7].
Many environmental changes are also linked to urbanisation. The WHO report on sanitation and drinking water2 shows that 137 million city dwellers worldwide have no access to safe drinking water and more than 600 million do not have adequate sanitation. These factors are prime contributors to the spread of infectious diseases, such as intestinal parasites leading to diarrheal infections and might cause cholera endemicity [6]. Air pollution has an impact on mortality with an association with cardiopulmonary and lung cancer [8] and an effect on the body’s respiratory and cardiovascular system. Health effects of air pollution also include breathing difficulties and worsening of existing chronic conditions such as asthma leading to increased medication use, hospital admissions and premature mortality.
2.4. Rising costs of healthcare
Rising healthcare cost is now a worldwide phenomenon to which many factors have contributed thus far. The most important being the prevalence of chronic and infectious diseases as mentioned above, in addition to providing long-term care for patients [9]. Another is the availability of novel technologies and the demand for them, especially in emerging economies. Rising hospital costs combined with increased patient demands are also driving factors. Obesity, especially in developed countries [10], has an impact on medical spending, with an estimated increase of 12% owing to obesity alone in some countries. Longevity brings the challenge of providing healthcare for a larger number of people with changing demographics. Rising labour, medication and energy costs over time are also contributing factors.
2.5. Prevention
Several debilitating and costly diseases, such as cardiovascular disease, cancer, diabetes and respiratory diseases are linked by several risk factors. Hypertension, smoking, cholesterol, malnutrition and poor diets, obesity, alcohol and physical inactivity are highlighted as the leading causes for preventable deaths worldwide [11]. The WHO indicates that most health-care systems are based on responding to acute problems and urgent needs of patients rather than preventative care. Although a shift toward preventative measures is seen in some countries, risk-reducing behaviours should be encouraged, especially for vulnerable groups.
3. How can pervasive sensing address these challenges?
Pervasive sensing is increasingly becoming a part of everyday healthcare owing to advances in sensor technology, its increasing availability, continuing miniaturisation and cost reduction [12,13]. Illustrated below is how pervasive sensing technologies can provide potential solutions to some of the aforementioned global challenges.
3.1. Pervasive sensing for infectious and chronic diseases
Early detection of pathogens is crucial in the treatment and prevention of infectious disease. Nanoscale materials with unique optical and magnetic properties have been efficiently used for the detection of pathogens as summarised in the survey by Tallury et al. [14]. Nanodiagonistics use nano-technology in clinical diagnosis of several infectious pathogens, including Escherichia coli, Salmonella and Influenza. Although these methods are now miniaturised, they are still non-pervasive as they normally require expert analysis and equipment. Further, to correct and to provide rapid-diagnosis, pervasive sensing can be used to observe patients recovering from a certain infectious disease, in terms of both their physiological parameters and behaviour patterns.
Research into chronic disease management, on the other hand, has shown several promising sensing systems for monitoring different parameters over time. Recent projects that are investigating or have investigated the use of sensors for chronic disease management include the European projects Chronious,3 WASP,4 HeartCycle,5 MyHeart6 and SAAL.7 Table 2, based on information presented in Body Sensor Networks [2] summarises some of the sensors for the observation of parameters relating to some of the most common chronic diseases. Even simple sensing paradigms where patients can use devices to remotely record and send sensor measurements to their clinicians, using a telecare device such as the Health Buddy,8 for example, have proven to be efficient for observing diseases such as asthma [15], diabetes and heart failure. One of the main challenges now is to make these sensors pervasive enough and embed them in the patient’s surroundings without affecting daily patterns and routines.
| Disease | Physiological parameters | Possible sensors |
|---|---|---|
| COPD | Respiration, heart rate Oxygen saturation and activity levels |
Wearable heart rate/respiration sensors Accelerometers |
| Parkinson's disease | Gait, muscle tone, activity | Accelerometers, optical/vision sensors Gyroscopes |
| Hypertension | Blood pressure/activity | Wearable blood pressure sensor Accelerometers |
| Cancer | Weight loss, activity, behaviour patterns | Accelerometers, gyroscopes Weight sensors |
| Arthritis | Gait patterns, temperature, stiffness | Accelerometers, optical/vision sensors Gyroscopes |
| Diabetes | Gait patterns, visual and sensory impairment | Accelerometers, vision, glucose monitors Gyroscopes |
| Cardiac arrhythmia | Heart rate, ECG | ECG sensors |
| Heart failure | Blood pressure | Heart rate and blood pressure sensors |
Some chronic diseases, physiological parameters that are of clinical importance and possible sensors that can be used to observe them.
For COPD (Chronic obstructive pulmonary disease), for example, a positive association exists between training intensity during rehabilitation and maximal oxygen consumption and muscle strength [16]. Thus, several of the previous works on COPD have been on activity detection and its correlation with recovery. This also applies to cardiac rehabilitation and post-operative monitoring.
3.2. Understanding ageing and research on elderly care
Ageing, being one of the most important challenges faced by both developing countries and the developed world, has led to several research directions focussing on how pervasive sensing can help researchers understand the ageing process itself, as well as dealing with some of the aspects of ageing. The following sections summarise these research directions.
3.2.1. Beyond telecare and enabling independent living
The review conducted by Barlow et al. [17] investigated the use of telecare for frail, elderly people and those with chronic conditions, summarising the results of 8666 studies. Based on the study, the most effective telecare interventions appeared to be automated vital signs monitoring (for reducing health service use) and telephone follow-up by nurses. The cost-effectiveness of these interventions was less certain.
The aim of telecare is to provide the elderly with means of conducting their daily activities with minimal or no intervention. Combining telecare systems with wearable and ambient systems can enable continuous care as well as the observation of changes in behaviour routines [18,19]. Several studies have been conducted worldwide for the combination of sensors with telecare, and many systems are summarised in “A review of approaches to mobility telemonitoring of the elderly in their living environment” [20]. The sensors used included passive infrared (PIR) sensors, magnetic sensors observing door use, bed-sensors, sound sensors, electrical-usage sensors, wearable sensors including accelerometers, gyroscopes and magnetometers or a combination of several wearable and ambient sensing modalities [18,21]. In addition to monitoring, several commercial telecare solutions include a digital alarm unit that can either be triggered by pushing a button or by a sudden change in vital signs or a fall.
3.2.2. Fall detection and management
Given that falls are the leading cause for injury among the elderly, a large amount of pervasive sensing research has focused on fall detection. One of the most dangerous side effects of a fall is the prolonged period the elderly spend on the ground and the risk factors attached thereto. Thus, early detection and rapid response by trained staff is essential in fall management. Several pendant systems for fall-reporting are available, but require that the elderly press a button after a fall. This might not be possible in case they suffer from a loss of consciousness. Automatic methods for fall detection using sensing include the use of image-based sensing [22], arrays of acoustic detectors [23], gyroscopes [24], accelerometers on their own or combined with air-pressure sensors [25].
Several strategies can be adopted for the prevention of falls, including specific exercises, education and assessing homes for extrinsic factors. Medical assessment can also identify intrinsic causes of falls and is normally based on a clinician’s observation of patient performance during a lab-based test. Recently, pervasive sensing has been used to assess the risk of falls aimed at providing a method of continuous assessment without the need for a hospital visit. Examples are the work by King et al. using an ear-worn accelerometry device [26], wearable shoe-insoles by Oberzaucher et al. [27] and waist-worn accelerometers by Gietzelt et al. [28].
3.3. Understanding the influence of environmental factors on health
Environment and climate changes have already been monitored constantly by meteorologists, geologists, environmentalists, biologists and biochemists, among others. This is mostly done through using remote sensing technologies, such as radar or satellite images, taking soil and water samples and installing air pollutant sensors in urban areas. However, owing to the extensive cost of traditional sensing technologies, such as satellite imaging, only macro measurements around large regions can be captured, and often only remedy actions can be taken in case of environmental incidents after they have occurred. In addition, the direct influence of environmental factors on human health is often very difficult to identify.
The recent advances in ultra-low power and low-cost wireless sensing technologies can significantly improve environment monitoring and enable real-time monitoring of micro-environments. Recent studies have demonstrated the feasibility and effectiveness of applying wireless sensor network (WSN) technologies to environment monitoring. These studies include: automatically monitoring soil conditions [29], the eruption of active volcanoes [30]; the impact of wind farms in coastal areas; and the behaviour of icecaps and glaciers [31]. Pervasive sensors also enable the monitoring of water supply systems [32] and air pollution monitoring [33]. With detailed environmental and health information acquired using the new wireless environmental sensors and pervasive health sensors, direct environmental impact on human health can be identified accurately. It will not only better the understanding of environmental health, but it will also help introduce precautionary measurements to minimise the effect of environmental hazards on human health.
3.4. Innovations in child and maternal health
The observation of physiological parameters, including respiration, heart rate and oxygen saturation (SO2) is crucial to the monitoring of premature or critically ill neonates. Continuous care is needed for the early detection of medical problems such as arrhythmias, convulsions and apnea. Adhesive and large, tethered sensors can cause discomfort to babies with fragile skin. The advances in wireless sensing technology have allowed the miniaturisation of the sensors used and their embedding in wearable garments, such as a jacket for neonatal ECG monitoring [34] and a biosensor belt for obtaining heart rate, breathing rate, movement and temperature [35]. A wearable wireless pulse oximetry oxygen saturation (SpO2) device using reflectance sensors was proposed in “Non-invasive blood oxygen saturation monitoring” [36] to obtain heart rate and oxygen saturation.
3.5. Applications in epidemiological studies
The previous sections presented a summary of how sensors have been integrated in different healthcare applications ranging from chronic diseases to child and maternal health. In this section, some of the current work aimed at using sensing in large-scale epidemiology studies will be surveyed.
Glucose monitoring has been one of the successful applications of pervasive remote sensing, especially with the introduction of continuous glucose monitors (CGM) that can help clinicians adjust therapy according to changes in the condition of the patient [37]. Studies have shown that a CGM identifies four times as many serious glucose excursions as Self-Monitoring of Blood Glucose (SMBG). These sensors have been used for several patient types, such as children [38] and patients with type 1 diabetes [39].
Another successful application of pervasive sensing has been that of using accelerometers for the quantification of physical activity, as a pedometer for step count, or integrated in watches and wearable devices. The study by Troiano et al. [40], for example, observed 6329 participants who provided at least 1 day of accelerometer data and from 4867 participants who provided four or more days of accelerometer data. These observations allowed the authors to compare activity between age groups, and deduce the adherence of groups to recommended amounts of physical activity. Accelerometers were also used in a longitudinal study observing 1032 participants and in deducing the role of decreased activity in childhood obesity [41].
Telemetry has been successfully used in several studies such as that of helping remotely observe the physical parameters/well-being of veterans (31,570 subjects [42]) and observing patients during their transport to hospitals in emergency medical service vehicles (494 patients) [43]. The next section will cover some of the challenges and obstacles facing the integration of pervasive sensors within such telecare systems.
4. A Common ground for innovation in pervasive healthcare
4.1. The role of communication technology and mobile networks
The rapid growth of the communication technologies and mobile networks have not only facilitated the information sharing for global health research, enhanced our understanding of diseases and influenzas, and improved the management of health services, but they have also enabled the realisation of pervasive health monitoring. With over 5 billion mobile phone connections, most of the world population has access to the mobile network which can also provide a backbone for pervasive sensing devices and enable the capturing of invaluable personalised health information. For instance, through integrating pervasive sensors, such as the BSN sensors [2], with mobile networks, detailed patient physiological and activity information can be gathered among large populations. This would help monitor the effects of infectious and chronic diseases, providing enriched information for health services in improving disease management. Even simple mobile phone programs, such as the iStethoscope,9 can potentially help with tracking the trend of chronic heart disease in the world population.
4.2. Adopting pervasive sensing technologies in healthcare and wellbeing
Fig. 2 shows several sensors that are currently used pervasively to monitor different parameters, including: (a) the Sensewear armband to monitor activity/energy expenditure10; (b) sensors embedded in a car seat to monitor heart function developed by FORD and RWTH11; (c) a sensor jacket for neonatal monitoring developed by Tu/e12; (d) the ear worn activity recognition sensor for gait and activity monitoring developed by Imperial College London [44]; (e) the Nike+ipod that allows runners to use a shoe-based sensor to monitor running performance on a mobile phone or an ipod13; and (f) integrating a BSN node [2] on the wheel of a wheelchair for observing wheelchair motion and paralympic athlete performance.14
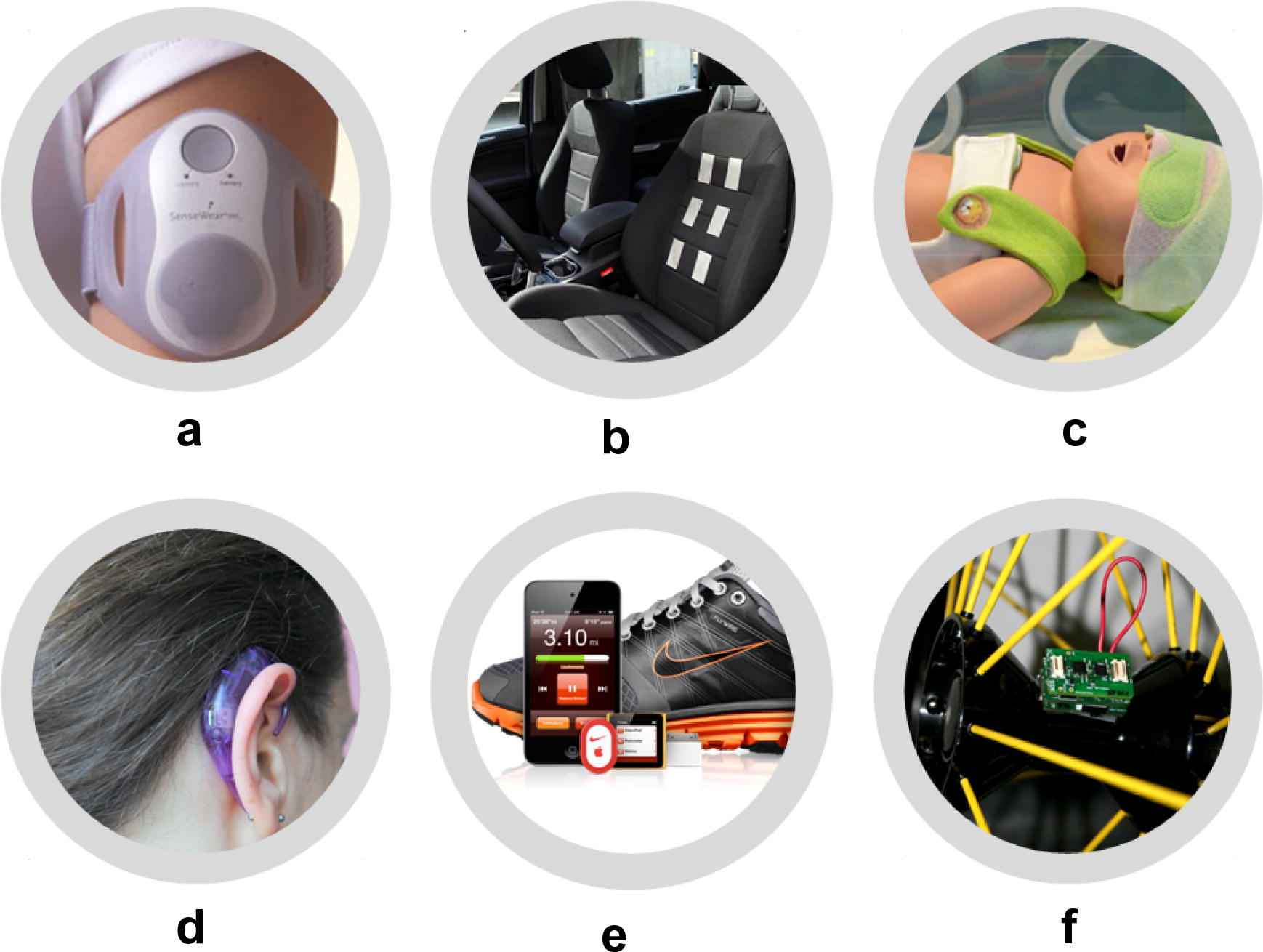
Sensors that can be embedded in everyday surroundings: (a) the Sensewear armband; (b) ECG monitoring on a car seat; (c) a sensor-jacket for neonatal monitoring; (d) an ear worn activity recognition sensor; (e) the Nike+ipod shoe-based sensor for monitoring running; and (f) a sensor to observe wheelchair motion and paralympic athlete performance.
The survey by Cook et al. [21] provides a summary of techniques deployed for providing ambient intelligence as a means of pervasive sensing within the context of smart homes and health monitoring and assistance. Ambient intelligence at home can be used to support people with mental and physical challenges, helping them to lead independent lives by recognising activity [18], detecting changes or anomalies, reminding them of tasks [45], or assessing cognitive limitations.
Fig. 3 highlights several challenges facing global healthcare and the particular solutions that could be provided by sensing systems. These solutions include sensor fusion from both ambient and wearable sensors to provide personalised context-aware sensing for monitoring an individual’s behaviour as well as the surrounding environment. An example of the use of sensing for continuous healthcare is that of post-operative surgery monitoring. Although current hospital recovery monitoring systems are effective during peri-operative and early postoperative periods, they cannot be used when the patient is at home. Following major surgery, patients are susceptible to complications such as infections, abscess formation and malnutrition which can lead to slow recovery rates. In “A pervasive body sensor network” [44], for example, an ear-worn sensor was used to observe activity levels of post-operative patients indicating changes over a few days after the operation. A wearable accelerometer was also used in “A new parameter for assessing postoperative recovery” [46] for comparing activity levels of patients undergoing laparoscopic versus open gastrectomy. An important aspect of post-operative recovery from different types of operations, especially in the orthopaedic domain, is the change in gait, and an amount of work has been dedicated to observing gait changes after surgery using pervasive sensors. Accelerometers, gyroscopes and force-sensors have both been used on different parts of the body to measure gait parameters [47]. Force-sensitive insoles were used to measure ground reaction forces and observe impaired gait in “Real-time gait event detection” [48]. Gyroscopes have also been used to observe knee-joint and hip-joint angles [49].
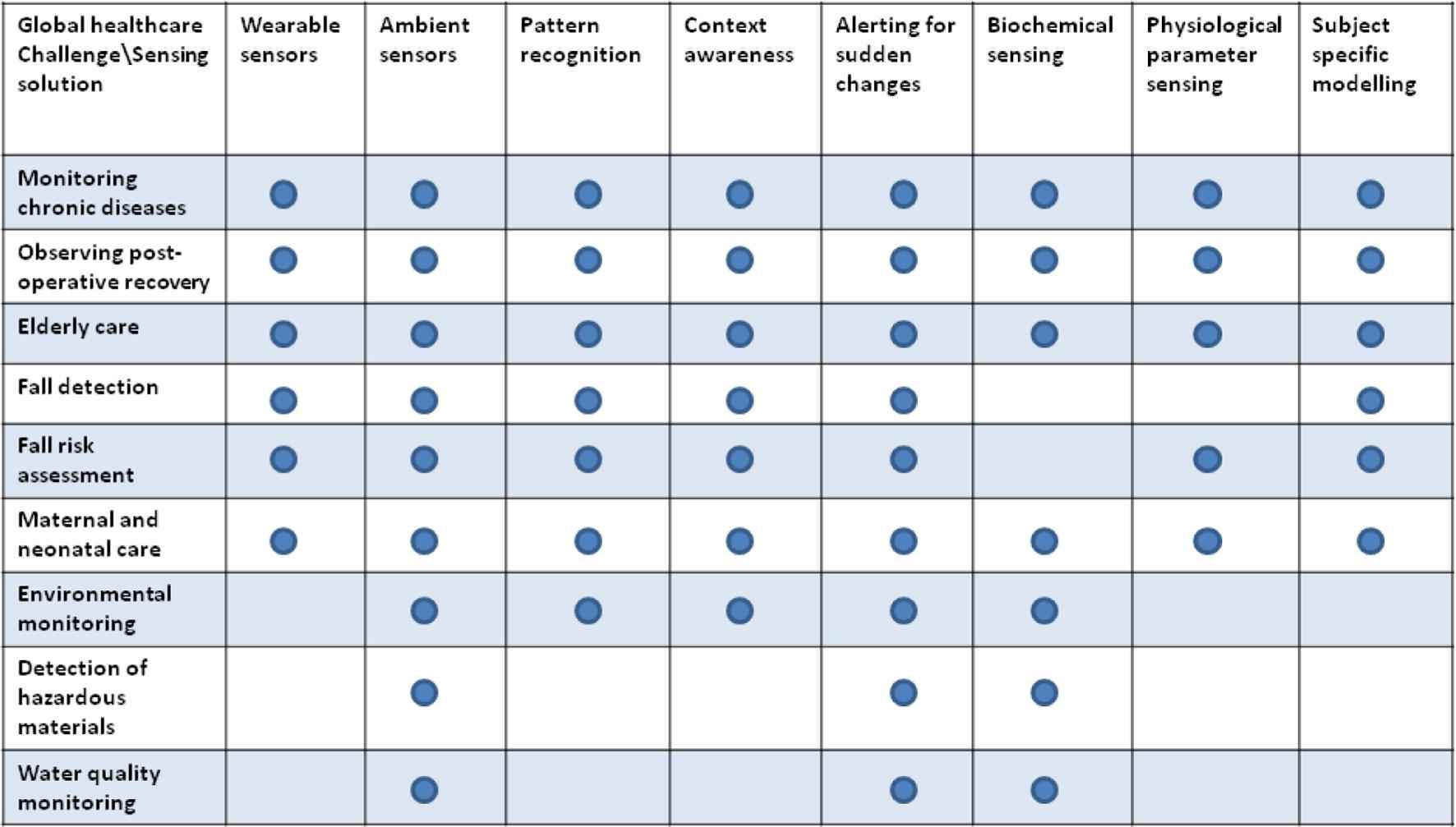
Several challenges facing global healthcare versus functionalities that could be provided by different sensing modalities.
4.3. Technical challenges to using pervasive sensors for healthcare scenarios
From a technical point of view, although sensors are now miniaturised and are equipped with efficient software, there are still challenges to be addressed before weaving them into the fabric of everyday life. Energy optimisation plays an important role in using pervasive sensing for remote monitoring. Energy consumption on sensor nodes depends on battery type, sensor types used, radio and CPU usage. In order to balance between overall energy consumption and performance, several measures can be considered. These include the use of data-compression, cache and proxy functionalities which can improve performance by reducing the traffic as well as the data-load. Appropriate data management and event handling can also help maximise performance. Efficient wake-up methods (which can be added as specific services) can save power and provide a rapid response to incoming events.
Reliability and dependability of sensor data (in terms of access and accuracy) are both vital in order to reduce false-alarm triggers, or more importantly to prevent loss of service which inhibits detection of deterioration (in the patient’s condition) or a serious event (such as a fall) [50]. Reliability involves having mechanisms for verification and correction as a guarantee of the reliable functioning of the BSN for long periods of time. The availability of several sensor types as well as sensing frameworks highlights the problem of heterogeneity in system deployment. The interoperability of these systems is of importance in making sensing solutions useable in real-life scenarios. This has opened several research directions in terms of providing service-oriented architectures for the integration of different types of sensors [51], as well as proposing multi-agent systems that manage the infrastructure of services within the environment both efficiently and securely by reasoning, task-planning, and synchronizing the data obtained from the sensors [19]. Middleware solutions that can facilitate network functionality and deal with node heterogeneity are also an area of research. The scope of the middleware used should cover sensor nodes as well as devices and connected networks. Examples include the open-source Uranus project,15 the Cougar project16 and the SCADDS project.17
Security constraints imposed by healthcare applications have several important objectives, including confidentiality, integrity, traceability and trustworthiness. To make sure these objectives are attained, several methods are used to safeguard wireless sensor networks from tampering, eavesdropping and intrusion detection. These methods include deploying secure software protocols for routing, secure data aggregation and the secure management of groups of nodes.
4.4. Challenges in market uptake of pervasive sensing solutions
Like most new technologies which are to be adopted in healthcare and the environment, pervasive sensing technologies have a life-cycle to be considered: consulting with end users, testing in safe simulation environments, then real world trials after obtaining ethical/regulatory approval.
The success of these sensors will definitely depend on their level of miniaturisation, built-in intelligent analysis and most importantly their integration with everyday objects used by people. From a wearable sensor perspective, more sensors are showing up embedded in textiles, watches, mobile phones, shoes and hearing aids. Ambient sensors, on the other hand, are all around, from temperature sensors to Passive Infra red (PIR) sensors and cameras that surround communities. It is also worth noting that several sensors can be used for more than one modality. An example is the Actiwatch,18 which includes time and activity monitoring, as well as sleep/wake patterns.
Ease of use of sensor nodes is of great importance in deploying them in everyday applications. This is facilitated by ergonomic design and integration within the surroundings, as well as wearable objects, without affecting daily patterns of behaviour. Programming sensor nodes can be a daunting task, especially for non-programmers. For this purpose, there have been several operating systems for programming nodes enabling the integration of different types of sensors and catering to scalability, reliability and security [52].
4.5. Challenges in adopting pervasive sensing solutions in large epidemiological studies
In addition to challenges relating to market uptake and technical questions posed by the use of pervasive sensors, their use on large-scale clinical trials also faces some obstacles. The first is that of regulatory approval and ethical issues relating to large medical trials. Questions relating to privacy, effect on other means of monitoring and ethical consequences need to be fully answered before a trial is given approval, which, although necessary, could lead to delays in terms of testing out new technologies. The pricing of such sensors could be a barrier for their adoption in large trials, especially if government agencies are providing funding for trials. The cost-efficiency of devices also needs to be investigated for large-scale trials with a minimisation of maintenance costs in the long run.
The large amount of ambient and wearable sensors used in large-scale patient studies definitely leads to vast amounts of data collected, especially when studies are performed over long periods of time. The main challenge has moved from being that of obtaining data to that of developing intelligent algorithms to perform pattern recognition, anomaly detection and behaviour monitoring with accurate information on compliance and surrounding context. Conventional data-mining methods might not be appropriate to deal with the distributed, subject-specific and context-varying nature of sensor data over such expansive parameters. Thus, data-mining for sensor data has evolved as a field of research posing several interesting questions that are yet unanswered. An important area of research is that of decision-making and designing knowledge-based systems using such vast amounts of data. Subject-specific models, learning from populations based on similarity and adaptive models that change according to patient variations are factors that will probably be included as such decision-making systems evolve to accommodate pervasive sensing data.
4.6. Emerging economies and changes in healthcare policies
The rapid growth of markets in countries like Brazil, China and India has lead to a change in how these nations use and produce innovative medical technologies. This growth has increased the demand for better quality healthcare, in terms of medical equipment, medications and information systems. Economic changes have signalled an era of change in living conditions, as well as daily habits, leading to more urbanisation and a general decrease in activity levels. Basic administrative systems in hospitals are being replaced by clinical information systems for patient records, accounts, and pharmacy/laboratory tests.
Investment in universities and medical research programmes in these countries will eventually lead to new world leaders in the production of new affordable technologies. Currently, developing nations are the leading markets for smaller and more affordable devices. The change in policies with respect to intellectual property protection as well as market competition will also affect how these nations produce and use novel technologies.
4.7. Opportunities in pervasive sensing
A paradigm shift from reactive to preventative healthcare is taking place worldwide with pervasive sensors playing a very important role in addressing some of the challenges posed. This article has addressed several challenges in global healthcare and has surveyed existing pervasive sensing systems that are being deployed to address these challenges. These systems offer a variety of exciting opportunities from a healthcare perspective. In this section three of these areas will be highlighted: encouraging active lifestyles, improving rehabilitation and providing better neonatal care.
Encouraging physical activity will increasingly play an important role in tackling increasing obesity worldwide. Sensors that can detect activity are currently used in sports and their integration with everyday objects, including mobile phones and watches, is ongoing. Providing feedback to people about their activity and encouraging them to be active is crucial if these sensors were to make a difference in behavioural patterns. Personalising feedback to match individual factors such as age, lifestyle and health status presents both a challenge and an opportunity for pervasive sensing.
The integration of pervasive sensors in rehabilitation programs is also an area that has started to see interesting applications. Games using sensors are widely available now and give an idea of how simple it is to make them part of everyday life. Encouraging patients to perform specific motions by using these sensors and giving them feedback on ranges of motions and forces deployed could be an important stage in rehabilitation, which can be administered remotely.
In addition to surveying applications and existing sensing systems, this article has also highlighted some of the challenges that accompany the use of sensing within large-scale epidemiological studies. These include technical challenges, such as energy optimisation, reliability, security and networking, as well as challenges from a user perspective stressing the importance of miniaturisation, ease of use and reasonable pricing. Large databases resulting from these studies pose a set of yet unsolved challenges in terms of designing decision-based systems based on distributed sensing, and developing context aware, subject specific and adaptable models.
Such large-scale studies pose a set of questions not only in terms of individual, but also in terms of group behaviour in relation to lifestyle, food-intake, genetic pre-disposition to disease and interaction with others. These sensors might help researchers understand how human behaviour is affected by these conditions as well as environmental factors. The influence of social, psychological and ethnic factors might also be better understood after observing group behaviour of large populations. The understanding of this type of data will require a combined effort between engineers, clinicians, behaviour scientists, psychologists and sociology experts.
Acknowledgement
This work was supported by the EPSRC-funded project ESPRIT (EP/H009744/1).
Footnotes
References
Cite this article
TY - JOUR AU - Louis Atallah AU - Benny Lo AU - Guang-Zhong Yang PY - 2012 DA - 2012/01/30 TI - Can pervasive sensing address current challenges in global healthcare? JO - Journal of Epidemiology and Global Health SP - 1 EP - 13 VL - 2 IS - 1 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2011.11.005 DO - 10.1016/j.jegh.2011.11.005 ID - Atallah2012 ER -
