Coverage of vitamin A supplementation and deworming during Malezi Bora in Kenya
- DOI
- 10.1016/j.jegh.2013.12.005How to use a DOI?
- Keywords
- Vitamin A; Deworming; Malezi Bora; Child health days; Kenya
- Abstract
Twice-yearly child health weeks are an effective way of reaching children with essential child survival services in developing countries. In Kenya, child health weeks, or Malezi Bora, were restructured in 2007 from an outreach-based delivery structure to a health facility-based delivery structure to reduce delivery costs and increase sustainability of the events. Administrative data from 2007 to 2011 have demonstrated a decrease in coverage of Malezi Bora services to targeted children. A post-event coverage (PEC) survey was conducted after the May 2012 Malezi Bora to validate coverage of vitamin A supplementation (VAS) and deworming and to inform program strategy. Nine hundred caregivers with children aged 6–59 months were interviewed using a randomized, 30 × 30 cluster design. For each cluster, one facility-based health worker and one community-based health worker were also interviewed. Coverage of VAS was 31.0% among children aged 6–59 months and coverage of deworming was 19.6% among children aged 12–59 months. Coverage of VAS was significantly higher for children aged 6–11 months (45.7%, n = 116) than for children aged 12–59 months (28.8%, n = 772) (p < 0.01). Eighty-five percent (51/60) of health workers reported that Malezi Bora was implemented in their area while 23.6% of primary caregivers reported that Malezi Bora occurred in their area. The results of this PEC survey indicate that the existing Malezi Bora programmatic structure needs to be reviewed and reformed to meet WHO guidelines of 80% coverage with VAS.
- Copyright
- © 2014 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Introduction
Vitamin A supplementation (VAS) is a widely recognized high-impact and cost-effective intervention for increasing child survival [1]. The World Health Organization recommends twice-yearly VAS in areas where vitamin A deficiency (VAD) is a public health concern to reduce all-cause mortality in children aged 6–59 months. Robust evidence from randomized controlled trials has shown twice-yearly VAS can reduce all-cause mortality by 24% in children 6–59 months of age [2]. Twice-yearly delivery of VAS through integrated Child Health Days (CHDs) is an effective method for reaching high and equitable coverage of child survival interventions including VAS.
Throughout sub-Saharan Africa, implementation of twice-yearly CHDs has been a common strategy to address the challenge of rising coverage rates of key child survival interventions and decreasing child mortality in a cost-effective way, particularly in areas with poor infrastructure [3]. CHDs deliver a package of high-impact child survival interventions that may include vitamin A supplementation (VAS), deworming, immunizations and insecticide-treated mosquito nets. Door-to-door distribution is effective at achieving high coverage, however, this distribution strategy can be costly in both money and human resources, and alternative strategies may be considered if funds and staff are not available [4].
In Kenya, VAS and deworming services were initially delivered through outreach-based twice-yearly child health campaigns, with VAS coverage from administrative data reaching a high of 93% in 2006 [5]. In 2007, Kenya’s child health campaigns were renamed Malezi Bora and restructured with a health facility-based delivery system rather than the previous outreach-based (door-to-door) system in an effort to reduce implementation costs. While the change in delivery structure for VAS and deworming reduced overall implementation costs, the change had an immediate impact on coverage with administrative data showing only 22% coverage of VAS in 2007 [5].
Administrative data from 2009–2012 indicate that VAS coverage from Malezi Bora has steadily increased, but coverage remains below the World Health Organization (WHO) recommended 80% to reduce child mortality [1]. During this period, the increase in coverage has been attributed to increased communication efforts surrounding Malezi Bora and targeted additional distribution through Early Child Development Centers (ECD) to reach children 3–5 years of age.
A Demographic and Health (DHS) Survey conducted in 2009 found coverage of VAS to be significantly less than that reported through administrative coverage (30.3% vs. 75.0%, respectively) [6]. The differences in reported coverage of the DHS and administrative data may be due to the longer recall period for the DHS, inaccurate targeted population numbers, and/or errors recording or tallying administrative data [7].
To validate administrative data for receipt of VAS and deworming through Malezi Bora within an acceptable recall period, a post-event coverage (PEC) survey was conducted after the May 2012 Malezi Bora. Secondary objectives of the survey were to determine factors associated with VAS and deworming receipt and evaluate caregiver and health worker knowledge of VAS to inform program strategy.
2. Materials and methods
A PEC survey was conducted in non-arid and non-semi-arid lands (non-ASAL) of Kenya following the May 2012 Malezi Bora, in which deworming capsules were distributed to children 12–59 months old and VAS was distributed to children 6–59 months old (100,000 IU for children 6–11 months old and 200,000 IU for children 12–59 months old). Non-ASAL areas comprise only 20% of Kenya’s landmass, but hold 75% of the Kenyan population and include the country’s capital city, Nairobi [8]. Data collection took place in June 2012, within six weeks of the May 2012 Malezi Bora, to ensure accurate recall of services received. Arid and semi-arid regions of Kenya were excluded due to a blanket supplementary feeding program in those areas through which VAS was distributed monthly. Applying standardized WHO Immunization Coverage Cluster Survey methodology [9], 30 clusters were randomly selected using probability proportionate to size (PPS) sampling and 2009 Kenya National Census data [10]. Because census data were only available at the sub-location level, clusters were selected at the sub-location level according to census enumeration areas and a village was selected at random in each sub-location.
In each cluster, interviews were conducted with 30 primary caregivers of children aged 6–59 months at the time of the May 2012 Malezi Bora. Households were randomly selected by identifying a central starting point in the cluster (church, mosque, communal center, etc.), spinning a pen to determine a direction, counting the number of houses from the starting point to the boundary of the cluster in the determined direction, and using a random number table to select the starting household from those households counted. Households were eligible if there was a child residing in the household who was 6–59 months of age at the time of the May 2012 Malezi Bora and their primary caregiver was present. If there were multiple eligible children in a household, one child was randomly selected by writing the names of each eligible child on separate slips of paper and selecting one at random. If a primary caregiver was not present, their location was requested and the caretaker was visited when possible. If the caretaker was not in proximity, the house was skipped due to time constraints. Informed oral consent was obtained from each caregiver interviewed.
After completing the first interview, enumerators proceeded to the next nearest house in the determined direction and so forth until 30 interviews were completed. Enumerators conducted surveys in teams of two to ensure data quality. Team leaders supervised each enumerator team at a minimum of five interviews per cluster, entering responses on a second survey form and comparing them with enumerators’ responses as an additional data assurance measure. Each team carried deworming tablets and vitamin A capsules in dosages of 50,000, 100,000 and 200,000 IU that were shown to caregivers to assist with recall of service uptake.
In each cluster, one community-based health worker (community health extension worker [CHEW] or public health technician [PHT]) and one facility-based health worker (nurse, clinical officer, or nutritionist) were interviewed using convenience sampling. Criteria for selection included working within the selected cluster in their respective field and participation in the May 2012 Malezi Bora event. Survey tools for both health workers and primary caretakers were structured to allow respondents to indicate multiple responses for relevant questions. For example, when measuring primary caretaker knowledge of vitamin A, all responses mentioned were recorded.
2.1. Statistical analysis
In total, 900 primary caregivers, 30 facility-based health workers and 30 community-based health workers were interviewed. Of the 900 caregivers interviewed, the responses of 12 caregivers were excluded because their child was later determined to be younger than six months or older than 59 months at the time of Malezi Bora. Due to the exclusion of these caregiver surveys, certain clusters were represented by fewer caregivers in the analysis. To adjust for this under-representation, a weight was derived for each cluster based on the number of eligible survey forms and these weights were used to conduct all analyses. For example, if in one cluster there were two caregivers with children who were below or above the accepted age range, the weight used for the said cluster was 30/28 or 1.07.
All data were entered using double data entry into an Epi Info database, compared for errors, and corrected as necessary by reviewing the original survey form. Areas were categorized as urban or rural according to their designation by the Kenya National Bureau of Statistics. Analysis was done using SPSS Version 20 (IBM, USA), with a p-value of <0.05 considered significant. In order to test for associations, Chi-square tests were conducted for categorical variables. A logistic regression analysis was performed with variables showing significant associations with VAS coverage to determine the extent of the relationship between each factor and VAS.
3. Results
3.1. Demographic characteristics
Demographic characteristics of the caregivers and children surveyed are listed in Table 1. The majority (81.6%) of caregivers were the selected child’s mother, with most (79.6%) residing in rural areas. Approximately half (45.5%) of caregivers interviewed with children 3–5 years of age reported that their child did not attend an Early Childhood Development (ECD) program even though they were eligible for attendance.
| Variable | n (%) |
|---|---|
| Area type | |
| Rural | 717 (79.6) |
| Non rural | 183 (20.4) |
| Sex of the child | |
| Male | 457 (50.8) |
| Female | 443 (49.2) |
| Child attends Early Childhood Development (ECD) program?* | |
| Yes | 204 (54.5) |
| No | 171 (45.5) |
| Relationship of caregiver with child | |
| Mother | 734 (81.6) |
| Grandmother | 67 (7.4) |
| Father | 46 (5.2) |
| Aunt | 23 (2.6) |
| Sibling | 7 (0.8) |
| Nanny/house help | 8 (0.9) |
| Other relative | 12 (1.3) |
| Highest level of schooling received by caregiver | |
| None | 55 (6.1) |
| Primary education | 560 (62.3) |
| Secondary education | 248 (27.5) |
| University education | 3 (0.3) |
| College education | 34 (3.8) |
Children ⩾3 years (n = 375).
Demographic characteristics of children selected as the focus of the interviews and their primary caregivers.
3.2. Vitamin A and deworming coverage during Malezi Bora
Coverage of VAS was 31.0% among children aged 6–59 months and coverage of deworming was 19.6% among children aged 12–59 months during the May 2012 Malezi Bora (Fig. 1). Coverage of VAS for children aged 6–11 months (45.6%, n = 117) was significantly higher than for children aged 12–59 months (28.8%, n = 783) (p < 0.01). Health facilities and dispensaries (45.7%) were the most frequently reported locations of VAS delivery during Malezi Bora, with VAS also received at the home (38.9%), at district hospitals (9.1%), mobile health posts (4.0%) and ECD (1.1%). The primary reasons that caregivers cited for not attending Malezi Bora were not having heard of the event (58.4%) and not having anyone available to take the child (5.3%) (Fig. 2).
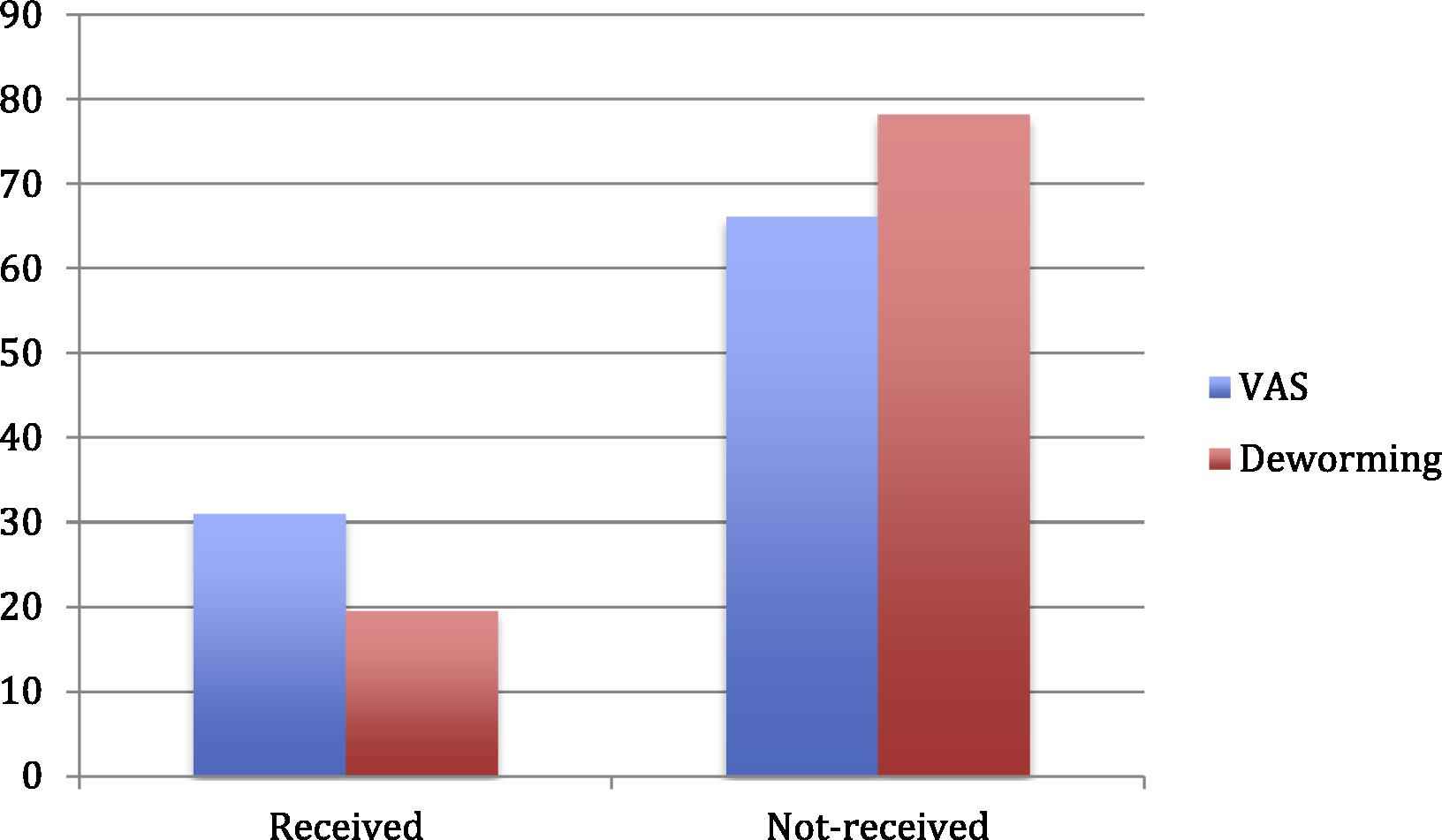
Coverage of VAS to children aged 6–59 months and deworming to children aged 12–59 months during the may 2012 Malezi Bora.
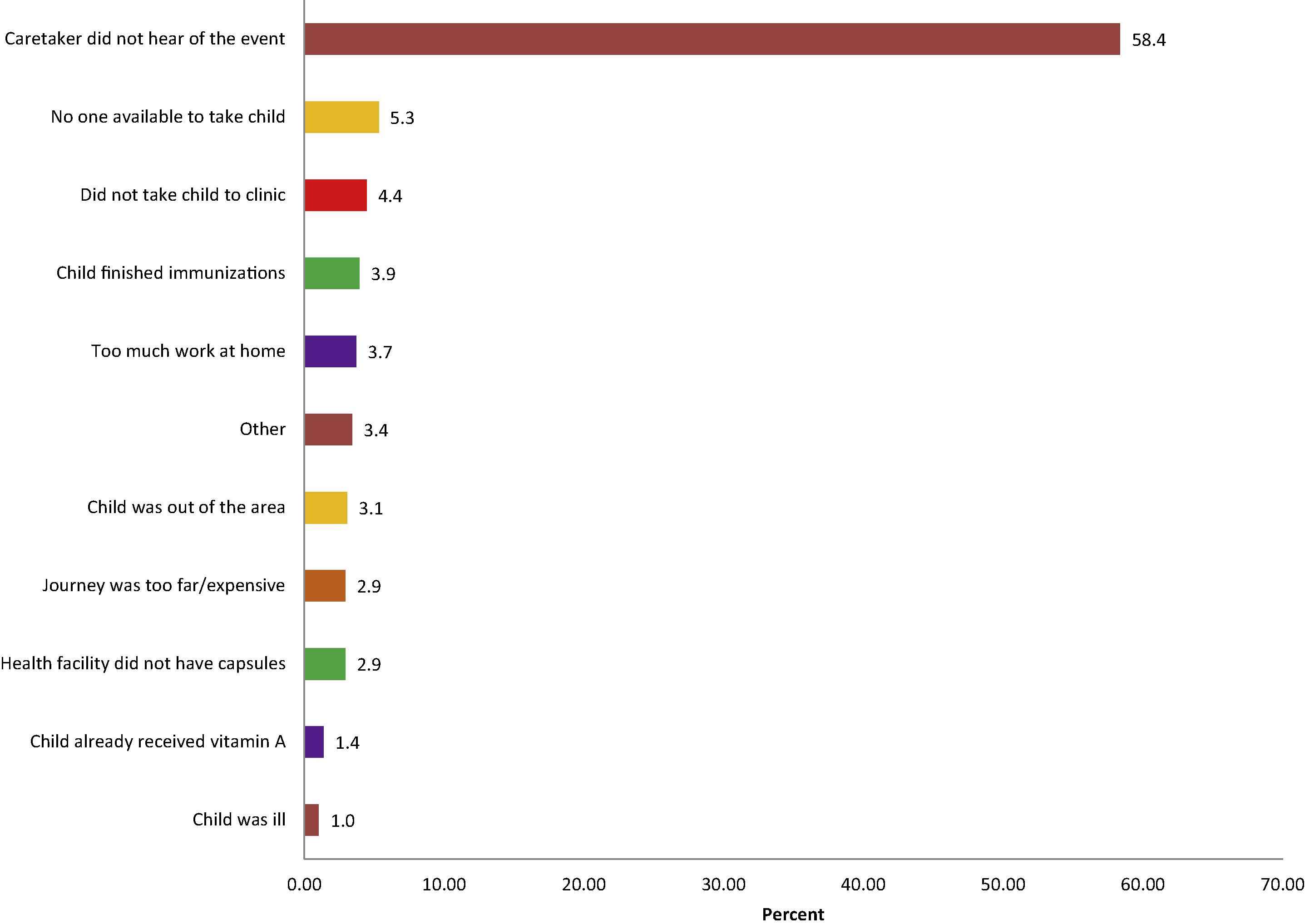
Reasons reported by caregivers why children did not attend the May 2012 Malezi Bora. Multiple responses were accepted.
3.3. Malezi Bora implementation and awareness
Ninety percent of facility-based health workers and 80.0% of community-based health workers reported that Malezi Bora was implemented in their area, while only one quarter of primary caregivers (23.6%) reported that Malezi Bora or a child health event took place in their area in the previous two months. Caregivers most frequently attributed their awareness of Malezi Bora to facility-based health workers (38.7%), radio (13.9%), community health workers (11.5%), word of mouth (9.8%) and community leaders (9.8%).
3.4. Knowledge of vitamin A
The majority of caregivers interviewed (85.8%) had heard of vitamin A. When asked about the benefits of VAS, 26.7% of caregivers responded that it protects against diseases, 20.8% said it improves child health, and one caregiver responded that it reduces mortality (Table 2). Less than a quarter of caregivers knew the correct age when VAS should first be administered (22.1%) or that children should be supplemented every six months (18.2%).
| Variable | Caregivers (n = 900) | Community-Based HWs (n = 30) | Facility-based HWs (n = 30) |
|---|---|---|---|
|
|
|||
| n (%) | n (%) | n (%) | |
| Benefits of vitamin A * | |||
| Protects against disease | 241 (26.7) | 22 (73.3) | 25 (83.3) |
| Improves child health | 188 (20.8) | 6 (20.0) | 4 (13.3) |
| Helps with growth/body building | 114 (12.7) | 14 (46.7) | 10 (33.3) |
| Increases appetite | 89 (9.9) | 3 (10.0) | 1 (3.3) |
| Increases energy | 55 (6.1) | 1 (3.3) | 0 (0.0) |
| Prevents blindness/helps vision | 52 (5.8) | 22 (73.3) | 28 (93.3) |
| Reduces risk of death | 1 (0.1) | 0 (0.0) | 2 (6.7) |
| Does not know/remember | 278 (31.0) | 0 (0.0) | 0 (0.0) |
| Other | 43 (4.7) | 4 (13.3) | 5 (16.7) |
| Age for first administration of vitamin A | |||
| At birth | 63 (7.0) | 0 (0.) | 2 (6.7) |
| 6 months | 198 (22.1) | 24 (80.0) | 26 (86.7) |
| 9 months | 38 (4.2) | 0 (0.0) | 1 (3.3) |
| Do not know | 189 (21.0) | 2 (6.7) | 0 (0.0) |
| Other | 284 (31.6) | 4 (13.3) | 1 (3.3) |
| How often children should receive vitamin A | |||
| At each Malezi Bora | 2 (0.2) | 0 (0.0) | 0 (0.0) |
| Every six months | 163 (18.2) | 24 (80.0) | 27 (90.0) |
| Does not know | 254 (28.3) | 2 (6.7) | 0 (0.0) |
| Other | 350 (38.9) | 4 (13.3) | 3 (10.0) |
| Vitamin A dosage for children 6–11 months * | |||
| One blue capsule (100,000 IU) | N/A | N/A | 27 (90.0) |
| Half of a red capsule | N/A | N/A | 8 (26.7) |
| One red capsule (200,000 IU) | N/A | N/A | 1 (3.3) |
| Do not know | N/A | N/A | 0 (0.0) |
| Other | N/A | N/A | 1 (3.3) |
| Vitamin A dosage for children 12–59 months | |||
| One blue capsule (100,000 IU) | N/A | N/A | 2 (6.7) |
| One red capsule (200,000 IU) | N/A | N/A | 27 (90.0) |
| Do not know | N/A | N/A | 0 (0.0) |
| Other | N/A | N/A | 0 (0.0) |
Multiple responses were accepted.
Caregiver, community-based and facility-based health worker knowledge of vitamin A supplementation.
Among health workers, VAS was most commonly associated with preventing disease and preventing blindness. Very few health workers (6.7%) recalled that VAS reduces mortality in children.
3.5. Health-seeking behaviors and health communications
When caregivers were asked where they seek health services most regularly and for what reasons, 90.0% of caregivers reported that they seek health services at government dispensaries, health facilities or hospitals, regardless of the age group (6–11 months vs. 12–59 months) of their child. Almost all caregivers (96.4%) stated that they seek health services when their child is sick, while 44.7% of caregivers reported that they also seek health services for routine visits and/or immunizations. When stratified by age, the results showed that a significantly higher proportion of caregivers with younger children (6–11 months old) tend to seek health services for routine visits and/or immunizations (p < 0.001).
3.6. Predictors of vas and deworming service uptake
Statistical analysis revealed that the recipient child’s age group (6–11 months and 12–59 months), the place where caregivers seek health services (district hospital versus other health institutions), and methods of getting health information (through community leaders versus other methods) are significant predictors of VAS uptake. As shown in Table 2, after controlling for the place where caregivers seek health services and methods of getting health information, children aged 6–11 months had twice the odds of receiving VAS compared with children 12–59 months of age (OR = 2.1, p < 0.01). For caregivers who regularly seek health services in a district hospital, the odds of their children receiving VAS were 0.61 times (OR = 0.61, p < 0.01) the odds of those who seek health services in other institutions, with all other factors being equal. After controlling for child’s age and place where caregivers seek health services, those caregivers getting health information from their community leaders had an estimated 1.5 times (OR = 1.5, p < 0.05) the odds of their children receiving VAS compared with those who get health information from other sources.
4. Discussion
Vitamin A and deworming coverage during the May 2012 Malezi Bora was significantly lower than WHO recommendations with coverage of 31.0% for VAS and 19.6% for deworming, which is consistent with VAS coverage measured by the 2009 DHS. According to WHO and UNICEF recommendations, twice-yearly VAS coverage of at least 80% is necessary to significantly increase child survival among children aged 6–59 months [11]. Based on a 24% reduction in child mortality with universal VAS coverage, an estimated 16,413 lives could be saved per year if universal VAS coverage is achieved in Kenya for children aged 6–59 months of age [HKI unpublished methodology].
Results from the current PEC survey suggest that low VAS and deworming coverage in Kenya is attributed to lack of caregiver’s awareness of Malezi Bora, minimal knowledge of VAS as a major child survival intervention, and low attendance of children over 12 months in health facilities for routine service delivery. Both caregiver awareness and low health facility attendance need to be addressed in subsequent Malezi Bora events to increase coverage of VAS and deworming service delivery.
Low awareness of Malezi Bora among caregivers is attributed to inadequate communication of Malezi Bora activities. Only 23.6% of caregivers recalled Malezi Bora being implemented and of caregivers whose children did not receive VAS, 58.4% stated that they had never heard that Malezi Bora had taken place. In the current Malezi Bora communication platform, interpersonal communication methods from health workers, members in the community and community leaders were the most effective in reaching caregivers and increasing their awareness. Additional social mobilization and communication activities such as radio spots, posters, and banners were rarely mentioned by caregivers as sources of information on Malezi Bora. Increasing awareness of Malezi Bora through effective communication methods such as interpersonal communication is recommended to increase awareness and demand of Malezi Bora services in subsequent rounds.
Survey results indicate increased outreach may be necessary to deliver Malezi Bora services. Nearly half of caregivers communicated that they only take their child to a health facility if their child is sick, which may explain in part why the majority of caregivers did not bring their children to the health facility to receive Malezi Bora services. To make the receipt of Malezi Bora services more convenient and to increase coverage to populations with poor access to health facilities, alternate distribution sites and methods may need to be considered.
Among the target population, children aged 6–11 months have twice the odds as children 12–59 months of age to receive VAS. This finding is consistent with the 2009 Kenya DHS, which showed that coverage of VAS was more than two times higher among children 9–11 months old compared with children 24–59 months old [6]. Higher coverage of younger children can be explained through (1) caregivers of younger children being more likely to visit health facilities because they are regularly coming for routine visits, and (2) younger children being more likely to be home and available to attend Malezi Bora compared with older children who are in school.
The current outreach strategy to distribute Malezi Bora services through ECD centers may not be the most effective method of outreach, as the current data suggest that ECD attendance is poor and that ECD distribution often does not occur due to lack of funding or poor planning. With poor attendance of children 3–5 years of age in ECD programs [12], additional outreach systems for Malezi Bora are needed to reach older children.
One potential platform to reach older children is during the second dose of measles vaccination delivered at 18 months, which is planned to be introduced into the EPI calendar. The second dose of measles would bring children below 2 years of age to the health center, but would not address low coverage of VAS among children older than 2 years of age. Vitamin A supplementation is frequently integrated with polio and measles campaigns, which achieves high coverage. Unfortunately, polio campaigns are infrequent and only occur when there is an outbreak, and measles campaigns only take place every 3–5 years. Therefore, integration into the measles and polio campaigns is not a sustainable method to deliver VAS.
Targeted delivery and communication strategies are needed to increase coverage of VAS and deworming during Malezi Bora and raise awareness of Malezi Bora among caregivers and the wider community. In addition to health facility based delivery of services, a community-based approach utilizing community health workers (CHW) may be warranted given that caregivers generally do not visit health facilities after their child turns one year aside from when their child is sick. A community outreach strategy would ideally utilize the existing system of CHWs and CHEWs to increase awareness of the community prior to Malezi Bora and to deliver VAS and deworming at the community level during Malezi Bora. In addition, it is recommended that targeted outreach of Malezi Bora services should be expanded from the existing ECD or school-based distribution to increase coverage among children 3–5 years old.
The recommendation to deliver VAS through a community outreach strategy is aligned with the WHO Reaching Every District (RED) strategy, which advocates for strengthening the linkage between communities and services via CHW and re-establishing outreach services to improve service delivery in distant communities [13]. All delivery strategies would need to be complimented by a strong and effective communication strategy to increase awareness of Malezi Bora in the community and create demand for Malezi Bora services among caregivers.
Limitations to this study include time constraints to complete the survey (one cluster per day per survey team) and reliance on caretaker recall. Population data were not available at the village level and thus a village was selected at random in each cluster to identify the first household to be visited in a cluster. This study’s strengths include data collection within six weeks of service delivery and multiple methods were applied to ensure data quality. In order to ensure data quality, experienced enumerators were selected and enumerators were required to work in pairs. During data collection, correct recording of responses was confirmed by supervisors who completed selected surveys in duplicate and double data entry was practiced.
5. Conclusion
The low coverage of VAS and deworming in Kenya during Malezi Bora indicate that the existing Malezi Bora programmatic structure needs to be examined and reformed to meet its original objectives at inception and address key challenges to service uptake demonstrated in these survey findings. Implementation of immediate changes to address poor coverage is critical to achieve necessary levels for improving child survival and decrease the incidence of child morbidity and mortality.
6. Contributions
NN, HIK and JLB conceived the study. PCC, NN, HIK, and JLB supported the implementation and trained the surveyors. GOM and MCI conducted the data analysis with support from HIK and JLB. PC drafted the manuscript and JLB and HIK revised the manuscript. All authors reviewed and approved the final manuscript.
7. Funding
This study was made possible by the generous support of the Canadian International Development Agency (CIDA). The contents are the responsibility of the authors and do not necessarily reflect the views of CIDA or the Canadian Government.
8. Conflicts of interest
None declared.
References
Cite this article
TY - JOUR AU - Paloma C. Clohossey AU - Heather I. Katcher AU - Geoffrey O. Mogonchi AU - Nancy Nyagoha AU - Marissa C. Isidro AU - Evelyn Kikechi AU - Edgar E.V. Okoth AU - Jessica L. Blankenship PY - 2014 DA - 2014/02/06 TI - Coverage of vitamin A supplementation and deworming during Malezi Bora in Kenya JO - Journal of Epidemiology and Global Health SP - 169 EP - 176 VL - 4 IS - 3 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2013.12.005 DO - 10.1016/j.jegh.2013.12.005 ID - Clohossey2014 ER -
