Prevalence and determinants of electrocardiographic abnormalities in African Americans with type 2 diabetes
- DOI
- 10.1016/j.jegh.2014.04.003How to use a DOI?
- Keywords
- Electrocardiogram; Diabetes; African Americans; Heart; Hypertension; Cardiovascular disease
- Abstract
Background: Electrocardiographic (ECG) abnormalities are independently associated with poor outcomes in the general population. Their prevalence and determinants were assessed in the understudied African American population with type 2 diabetes.
Methods: Standard 12-lead ECGs were digitally recorded in 635 unrelated African American-Diabetes Heart Study (AA-DHS) participants, automatically processed at a central lab, read, and coded using standard Minnesota ECG Classification. Age- and sex-specific prevalence rates of ECG abnormalities were calculated and logistic regression models were fitted to examine cross-sectional associations between participant characteristics and ECG abnormalities.
Results: Participants were 56% women with a mean age of 56 years; 60% had at least one minor or major ECG abnormality [23% ⩾1 major (or major plus minor), and 37% ⩾1 minor (with no major)]. Men had a higher prevalence of ⩾1 minor or major ECG abnormality (66.1% men vs. 55.6% women, p = 0.0089). In univariate analysis, age, past history of cardiovascular disease, diabetes duration, systolic blood pressure, sex and statin use were associated with the presence of any (major or minor) ECG abnormalities. In a multivariate model including variables, female sex (OR [95% CI] 0.79 [0.67, 0.93]), statin use (0.79 [0.67, 0.93]) and diabetes duration (1.03 [1.0, 1.05]) remained statistically significant.
Conclusions: Nearly three out of five African Americans with diabetes had at least one ECG abnormality. Female sex and statin use were significantly associated with lower odds of any ECG abnormality and diabetes duration was significantly associated with higher odds of any ECG abnormality in the multivariable model.
- Copyright
- © 2014 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Introduction
Associations between minor and major electrocardiographic (ECG) abnormalities and incident cardiovascular disease (CVD) are widely observed [1–6]. These associations persist after adjustment for traditional CVD risk factors suggesting they are independent. A higher prevalence of ECG abnormalities has been reported in African Americans (AAs) relative to European Americans [7,8] – a finding in accordance with higher CVD rates in the general AA population. Patients with diabetes are at a significantly increased risk of CVD events, and diabetes is widely accepted as a coronary artery disease risk equivalent [9–11].
Few studies have assessed the prevalence and determinants of ECG abnormalities in AAs with type 2 diabetes (T2D). It is currently recommended by the American Heart Association/American College of Cardiology Foundation (AHA/ACCF) guidelines to obtain ECGs for those with diabetes [12]. However, it remains unclear how best to use the results of the ECG to improve patient care. Information regarding the prevalence of ECG abnormalities in the high risk AA population with T2D could help guide efforts to develop risk stratification tools to identify those who may benefit from closer follow-up and aggressive risk factor management. There are potential subsets of patients with diabetes with high risk features that may be further elucidated by the ECG, a non-invasive and low-cost screening modality. The prevalence and associations of ECG abnormalities were examined in AAs with T2D enrolled in the African American-Diabetes Heart Study (AA-DHS), one of the most extensively phenotyped African ancestry cohorts for CVD and related risk factors in populations with diabetes.
2. Methods
2.1. Study population
The study sample included 635 consecutive unrelated, self-reported AAs with T2D recruited in the parent Diabetes Heart Study (DHS) and subsequent AA-DHS. In the DHS, siblings concordant for T2D were recruited from internal medicine clinics and community advertising [4]. One member of each AA sib-pair was included and T2D was diagnosed after the age of 34 years in the absence of historical evidence of ketoacidosis. An additional 555 unrelated AAs were subsequently enrolled in the AA-DHS using the same diagnostic criteria, except that T2D was diagnosed after the age of 30 years. Inclusion criteria in both studies allowed individuals with prior myocardial infarction, angina, congestive heart failure, transient ischemic attack, and stroke, but excluded those with previously diagnosed advanced nephropathy (estimated glomerular filtration rate <60 ml/min/1.73 m2 or end-stage renal disease). Although not excluding participants with prevalent cardiovascular disease may lead to overestimation of ECG abnormalities, it is well established that the diabetic population are at high risk of CVD and excluding those with CVD will risk the representative nature of this sample. Identical examinations were conducted in the Clinical Research Unit of the Wake Forest School of Medicine in DHS and AA-DHS, including interviews for medical history, current medications and health behaviors, measurements of body size, resting blood pressure, 12-lead ECG, fasting blood draw, and spot urine collection. These studies were approved by the Institutional Review Board at the Wake Forest University School of Medicine, and all participants provided written informed consent.
2.2. Electrocardiographic measures
A resting 12-lead ECG was obtained from all participants using a GE MAC 1200 electrocardiograph (GE, Milwaukee, Wisconsin). The digitally collected ECG tracings were transmitted via phone line to be centrally read and coded at the Epidemiological Cardiology Research Center (EPICARE), Wake Forest School of Medicine (Winston-Salem, NC). All ECGs were initially checked for quality before being automatically processed using the GE Marquette 12-SL version 2001 software (GE, Milwaukee, Wisconsin). The Minnesota coding system was used to classify ECG tracings as having a major or minor abnormality [13]. Participants with only minor ECG abnormalities were classified as having “any minor abnormalities”, and participants with major ECG abnormalities with or without coexisting minor ECG abnormalities were classified as having “any major ECG abnormalities”. Major ECG abnormalities included: major ventricular conduction defect; definite myocardial infarction (defined as the presence of major Q wave abnormalities); possible myocardial infarction (defined as the presence of minor Q/-QS wave plus major ST/-T abnormalities); major isolated-ST/-T abnormalities; left ventricular hypertrophy; major atrioventricular conduction abnormalities; major QT prolongation (QT ⩾ 116%), pacemaker, and other major arrhythmias. Minor ECG abnormalities included: minor isolated Q/-QS waves; minor isolated ST/-T abnormalities; high R waves; ST segment elevation; incomplete (left and right) bundle branch block; minor QT prolongation (QTi ⩾ 112%); short PR interval; left axis deviation; right axis deviation; frequent ventricular premature beats; and other minor arrhythmias.
2.3. Statistical analysis
Baseline characteristics were described for the total cohort, and the prevalence of ECG abnormalities (minor, major, and any minor or major) was tabulated in all participants and stratified by the presence or absence of ECG abnormalities. The prevalence rates of ECG abnormalities were compared between each baseline covariate (Table 1) and between men and women (Table 2) using chi square tests for categorical variables and the Wilcoxon two-sample test for continuous outcomes, as appropriate. Logistic regression models were run to test the association between ECG abnormalities (major, minor, and major/minor) adjusted for different sets of covariates, considered in a sequential fashion. Models were constructed as follows: univariate model, multivariable model adjusted for covariates that were statistically significant in the univariate model. Statistical significance was defined as p < 0.05. Analysis was performed using SAS version 9.1 (SAS institute, Cary, NC).
| With ECG* abnormality | Without ECG* abnormality | Combined* sample | p-Value† | |
|---|---|---|---|---|
| Number | 382 | 208 | 590 | |
| Age (years) | 56.8 (9.7) | 54.4 (9.2) | 56.0 (9.5) | <0.01 |
| Female (%) | 65.38% | 52.09% | 56.78% | <0.01 |
| Body mass index (kg/m2) | 34.5 (8.5) | 36.0(8.2) | 35.0(8.5) | 0.02 |
| Smoking (%) | 0.48 | |||
| Current | 25.13% | 23.08% | 24.72% | |
| Ever | 37.70% | 34.62% | 36.85% | |
| Never | 37.17% | 42.31% | 38.43% | |
| Age at diabetes (years) | 46.0 (10.5) | 45.4 (9.4) | 45.8 (10.0) | 0.53 |
| Diabetes duration (years) | 11.2 (9.0) | 8.8 (5.8) | 10.3 (8.1) | 0.04 |
| Hemoglobin A1C (%) | 8.3 (2.0) | 8.0 (2.0) | 8.2 (2.0) | 0.08 |
| Total cholesterol (mg/dL) | 180.7 (46.8) | 182.8 (43.6) | 181.7 (45.2) | 0.45 |
| LDL-cholesterol (mg/dL) | 107.5 (37.8) | 109.6(37.2) | 108.7(37.3) | 0.45 |
| HDL-cholesterol (mg/dL) | 47.4 (13.5) | 48.4 (13.7) | 47.7 (13.5) | 0.41 |
| Triglycerides (mg/dL) | 131.4 (140.2) | 125.9 (102.8) | 130.0 (125.0) | 0.76 |
| Dyslipidemia (%) | 89.79% | 91.83% | 90.51% | 0.47 |
| Hypertension (%) | 84.76% | 78.85% | 82.65% | 0.09 |
| Systolic blood pressure (mmHg) | 135.1 (20.2) | 131.1 (17.4) | 133.6 (19.3) | 0.03 |
| Diastolic blood pressure (mmHg) | 77.7 (11.6) | 77.5 (11.3) | 77.5 (11.4) | 0.96 |
| History of CVD (%) | 5.5% | 0.96% | 3.9% | <0.01 |
| Use of diabetes medications | ||||
| Insulin (%) | 44.24% | 32.21% | 40.00% | <0.01 |
| Oral (%) | 74.35% | 83.17% | 77.46% | 0.02 |
| Statin use (%) | 52.49% | 42.31% | 48.90% | 0.02 |
Values expressed by N (%) or mean (SD); CVD – cardiovascular disease.
p values for the presence of ECG abnormalities versus absence of ECG abnormalities.
Baseline characteristics stratified by the presence of ECG abnormalities.
| Description | Men % (N) of abnormalities |
Women % (N) of abnormalities |
Combined % (N) of abnormalities |
p-Value |
|---|---|---|---|---|
| Any major or minor ECG abnormality (%) | 66.1% | 55.6% | 60.0% | <0.01 |
| Minor ECG abnormalities | 59.90% | 50.80% | 54.8% | 0.03 |
| Minor isolated Q,QS waves | 9.8% (27) | 7.0% (25) | 8.2% (52) | 0.37 |
| Minor isolated ST,T abnormalities | 22.7% (63) | 25.4% (91) | 24.3% (154) | 0.71 |
| High R waves | 15.6% (44) | 16.8% (60) | 16.4% (104) | 0.88 |
| ST segment elevation, anterolateral site | 1.8% (5) | 1.4% (5) | 1.6% (10) | 0.85 |
| ST segment elevation, posterior site | 1.4% (4) | 0.6% (2) | 0.9% (6) | 0.51 |
| ST segment elevation, anterior site | 3.6% (10) | 2.5% (9) | 3.0% (19) | 0.71 |
| Incomplete right bundle branch block | 0.7% (2) | 1.4% (5) | 1.1% (7) | 0.86 |
| Incomplete left bundle branch block | 16.3% (45) | 5.3% (19) | 10.1% (64) | <0.01 |
| Minor QT prolongation | 2.5% (7) | 2.8% (10) | 2.7% (17) | 0.55 |
| Short PR | 0% (0) | 0.3% (1) | 0.2% (1) | 1.00 |
| Left axis deviation | 8.3% (23) | 2.8% (10) | 5.2% (33) | <0.01 |
| Right axis deviation | 0% (0) | 0% (0) | 0% (0) | 0.75 |
| Frequent ventricular premature beats | 3.3% (9) | 3.1% (11) | 3.2% (20) | 1.00 |
| Other minor abnormalities | 12.6% (35) | 10.4% (34) | 10.9% (69) | 0.25 |
| Major ECG abnormalities | 26.40% | 20.50% | 23.00% | 0.12 |
| Complete left bundle branch block | 0% (0) | 0.6% (2) | 0.3% (2) | 0.65 |
| Complete right bundle branch block | 1.4% (4) | 2.0% (7) | 1.7% (11) | 0.96 |
| Nonspecific intraventricular block | 1.4% (4) | 0.6% (2) | 1.0% (6) | 0.58 |
| Complete/intermittent RBBB w/left anterior hemiblock | 0% (0) | 0.3% (1) | 0.18% (1) | 1.00 |
| Major Q wave abnormalities [old MI] | 7.2% (20) | 3.9% (14) | 5.4% (34) | 0.16 |
| Minor Q/QS waves with ST/T abnorm. (possible old MI) | 2.5% (7) | 2.0% (7) | 2.2% (14) | 0.85 |
| Major isolated ST-T abnormalities | 12.3% (34) | 11.5% (41) | 11.8% (75) | 0.89 |
| Left ventricular hypertrophy (with strain pattern) | 4.0% (11) | 5.6% (20) | 4.9% (31) | 0.65 |
| Atrial fibrillation | 1.1% (3) | 0.3% (1) | 0.6% (4) | 0.32 |
| Major QT Prolongation | 1.1% (3) | 1.1% (4) | 1.26% (7) | 0.42 |
| Pacemaker | 0% (0) | 0.6% (2) | 0.3% (2) | 0.61 |
Prevalence of ECG abnormalities stratified by sex.
3. Results
The study sample included 635 unrelated AAs with T2D having a mean ± SD age of 56 ± 9.5 years, 56% (n = 358) were women. Characteristics of the study population are detailed in Table 1 stratified by the presence or absence of ECG abnormalities. Participants with ECG abnormalities, relative to those without, were more likely to be older, female, having lower body mass indices, longer diabetes durations, higher systolic blood pressures, history of cardiovascular disease defined as prior coronary artery bypass surgery or carotid endarterectomy, and were more often taking insulin and statin medications (Table 1).
Approximately 60% (N = 381) of participants had ⩾1 minor or major ECG abnormality. Major ECG abnormalities were present in 23% and minor ECG abnormalities (with no major abnormality) in 54.8% of participants. Table 2 presents prevalent ECG abnormalities stratified by sex. The most common finding was minor isolated ST-T abnormalities seen in 24.3% of the participants, followed by high R waves (16.4%), major isolated ST-T abnormalities (11.8%), other minor arrhythmias (10.9%), and incomplete LBBB (10.1%). Relative to women, men were more likely to have an incomplete LBBB (p ⩽ 0.0001) and a left axis deviation (p < 0.0001). In sex-stratified analysis, major ECG abnormalities had a statistically significant p-value for trend (p = 0.0069) in men for every 10 year increase in age from 30 to >70 years. In women, major or minor abnormalities had a statistically significant p for trend (p = 0.025) for 10-year incremental increase in age (Fig. 1).
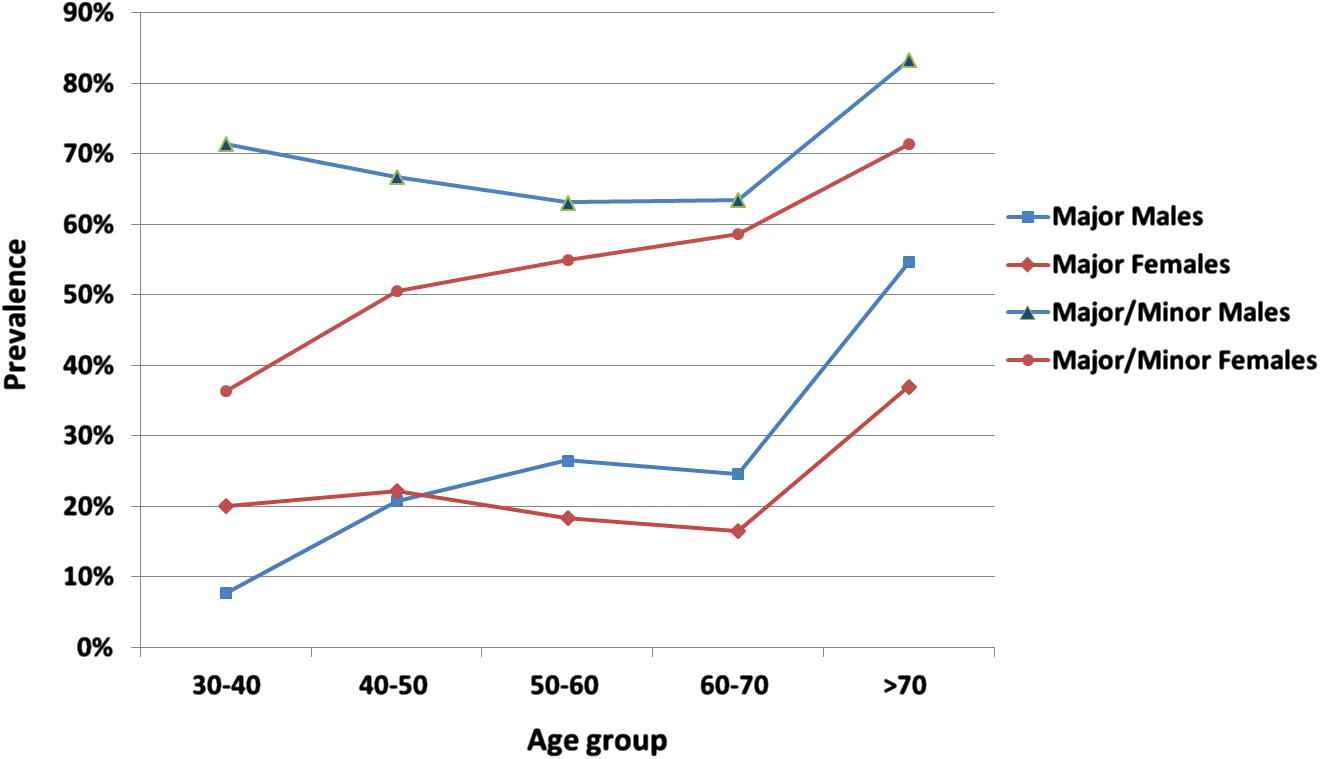
Prevalence of any major and major or minor ECG abnormalities by genders and age groups.
Results of the logistic regression analysis examining associations between ECG abnormalities, sex and other CVD risk factors are shown in Table 3. In the univariate analysis, age (odds ratio [OR] 1.02, [95% Confidence Interval] 1.01, 1.04), presence of cardiovascular disease defined as prior coronary artery bypass graft surgery or carotid endarterectomy (OR 0.59 [0.36, 0.97]), diabetes duration (OR 1.04 [1.01, 1.06]), systolic blood pressure (OR 1.01 [1.0, 1.02]), sex (OR 0.80 [0.68, 0.94]) and statin use (OR 0.79 [0.67–0.93]) were associated with major or minor ECG abnormalities. In the univariate analysis of the association with major ECG abnormalities, similar results were seen with age, presence of cardiovascular disease, systolic blood pressure and statin use; however, diabetes duration and sex were not statistically significant. In the univariate analysis of the association with minor ECG abnormalities, only diabetes duration and statin use were statistically significant (OR 1.03 and 0.78, respectively). In the multivariable analysis of any ECG abnormality, including variables that were statistically significant in each univariate analysis, diabetes duration, sex, and statin use remained statistically significant with ORs (95% CI) 1.03 (1.00, 1.05), 0.79 (0.67, 0.93), and 0.83 (0.70, 0.99), respectively. In the multivariable analysis of only minor ECG abnormalities, diabetes duration OR 1.03 (1.00, 1.05) and statin use OR 0.80 (0.67, 0.95) were statistically significant. Finally, multivariable analysis of major ECG abnormalities revealed that a history of coronary artery bypass surgery or carotid endarterectomy (OR 0.36 [0.20, 0.65]) and systolic blood pressure (OR 1.01 [1.00, 1.03]) were statistically significant.
| Any ECG abnormality | Major ECG abnormalities | Minor ECG abnormalities | ||||
|---|---|---|---|---|---|---|
| Univariate OR (95% CI) |
Multivariable* OR (95% CI) |
Univariate OR (95% CI) |
Multivariable* OR (95% CI) |
Univariate OR (95% CI) |
Multivariable* OR (95% CI) |
|
| Age (per year) | 1.02 (1.01, 1.04) | 1.01 (0.99, 1.03) | 1.03 (1.00, 1.05) | 1.01 (0.99, 1.04) | 1.01 (0.99, 1.02) | |
| Female sex | 0.80 (0.68, 0.94) | 0.79 (0.67, 0.93) | 0.84 (0.68, 1.04) | 0.89 (0.74, 1.06) | ||
| Body mass index (kg/m2) | 0.98 (0.96, 1.00) | 0.99 (0.96, 1.01) | 0.99 (0.97, 1.01) | |||
| HDL cholesterol (per 1 mg.dl) | 0.99 (0.98, 1.01) | 0.99 (0.97, 1.00) | 1.00 (0.99, 1.01) | |||
| LDL cholesterol (per 1 mg.dl) | 1.00 (0.99, 1.00) | 1.00 (0.99, 1.00) | 1.00 (0.99, 1.00) | |||
| Triglycerides (per 1 mg.dl) | 1.00 (0.99, 1.00) | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) | |||
| Total cholesterol (per 1 mg.dl) | 0.99 (0.99, 1.00) | 0.99 (0.99, 1.00) | 0.99 (0.99, 1.00) | |||
| Statin (use vs. no use) | 0.79 (0.67, 0.93) | 0.83 (0.70, 0.99) | 0.74 (0.60, 0.92) | 0.84 (0.67, 1.06) | 0.78 (0.65, 0.93) | 0.80 (0.67, 0.95) |
| Systolic BP (per 1 mmHg) | 1.01 (1.00, 1.02) | 1.01 (1.0, 1.02) | 1.02 (1.01, 1.03) | 1.01 (1.00, 1.03) | 1.00 (0.99, 1.01) | |
| Hypertension | 0.84 (0.68, 1.04) | 0.69 (0.50, 0.95) | 0.76 (0.53, 1.08) | 0.96 (0.76, 1.20) | ||
| **CV disease | 0.59 (0.36, 0.97) | 0.63 (0.36, 1.09) | 0.37 (0.22, 0.63) | 0.36 (0.20, 0.65) | 0.71 (0.40, 1.28) | |
| Hgb HbA1C | 1.06 (0.97, 1.14) | 1.06 (0.96, 1.17) | 1.05 (0.96, 1.15) | |||
| †Insulin use | 0.90 (0.65, 1.23) | 1.01 (0.52, 1.97) | 0.57 (0.28, 1.14) | |||
| Duration DM (per year) | 1.04 (1.01, 1.06) | 1.03 (1.0, 1.05) | 1.03 (1.00, 1.05) | 1.03 (1.01, 1.05) | 1.03 (1.00, 1.05) | |
| Smoking (vs. current smoker) | 0.92 (0.74, 1.14) | 0.91 (0.68, 1.23) | 0.85 (0.66, 1.09) | |||
Multivariate analysis including factors significant in the univariate model, unadjusted for multiple comparisons.
CV Disease = history of coronary artery bypass surgery or carotid endarterectomy.
Insulin = diabetes off treatment versus insulin therapy.
Associations between cardiovascular disease risk factors and ECG abnormalities.
4. Discussion
Existing reports evaluating the prevalence and significance of ECG abnormalities has predominantly been performed in middle-aged men of European ancestry. The Atherosclerosis Risk in Communities (ARIC) [8], Charleston Heart Study [6], Evans County Study [14] and Coronary Artery Risk Development in Young Adults (CARDIA) [7] studies illustrate the impact of race/ethnicity on ECG abnormalities. However, these studies included a minor subset of AAs with diabetes, and in some studies diabetes was an exclusion criterion. Therefore, the AA-DHS is uniquely situated to provide insights regarding the prevalence of ECG abnormalities in AAs with T2D. A remarkably high prevalence of ECG abnormalities was detected in the AA-DHS cohort; 23% of subjects had major abnormalities and 54.8% had minor abnormalities. In comparison, AAs in CARDIA had 10.2% major abnormalities and 17.7% minor abnormalities. In ARIC, AAs had 5.5% and 33% major and minor abnormalities, respectively.
Several results from the AA-DHS parallel existing data in AAs. In CARDIA, high R wave voltage (23.3% in AA men, 11% in AA women), followed by any minor ST-T abnormalities (15.2% and 12.7%, respectively), and incomplete LBBB (17.4% and 4.2%, respectively) were among the most common ECG abnormalities seen in AAs [7]. In ARIC, high amplitude R waves (19.1% in AA men and 11% in AA women), minor T wave abnormalities (10.7% and 8.6%, respectively) and ST segment elevation (14.6% and 0.2%, respectively) were among the most common findings. High amplitude R waves were also found to be more prevalent in the Evans County Study [14]. It appears that the relative distributions of individual ECG abnormalities from AA-DHS are in accordance with those reported in ARIC, CARDIA, and Evans County; however, their overall prevalence was far higher. The high prevalence of ECG abnormalities in AA-DHS may partially explain the reported poor CVD outcomes in AAs and in patients with diabetes.
The prevalence and distribution of ECG abnormalities in this study that included African Americans are comparable to the estimates reported from Africans living in Africa [15–19]. It is important, however, to notice that African Americans are different from Africans still living in Africa. Despite the common ancestry, the western lifestyle has changed the characteristics and disease patterns dramatically in individuals with African ancestry. Also, the methods of defining ECG abnormalities between those in this study (using Standard Minnesota code at a central ECG core lab) and these studies trigger the need to be careful in making direct comparisons. This calls for a comparative study between blacks living in different places (Africans living in Africa, African Americans, African Caribbean, African Europeans, etc.) using a similar methodology. This study was also less informed about the variations in normal ECGs between blacks and whites [19]. So, a white comparison group may have been useful for interpretation of the ECG abnormalities in this study, which was not possible in this study and is one of the limitations.
Associations between ECG abnormalities and CVD events are well established in the general and patient-based populations [1–3,5,6,20,21]. The remarkably high prevalence of ECG abnormalities in AAs with T2D will require examination of the risk of CVD-associated events with ECG abnormalities. At this stage, follow-up outcomes’ data in the AA-DHS are lacking and the association between ECG abnormalities and CVD cannot be examined. Additional study limitations inherent to the cross-sectional design include potential residual confounding in the logistic regression models. In addition, ECGs were obtained at one time point. Some ECG criteria may be dynamic in nature and could arguably be more significant if multiple ECGs were obtained at different time points. Finally, by design, AA-DHS participants with an estimated glomerular filtration rate <60 ml/min/1.73 m2 or end-stage renal disease were excluded. This may impact the generalizability of the results if applied to the spectrum of diabetics with renal disease. Therefore, a population without advanced CKD was needed and hence recruitment did not consider those with advanced CKD.
In conclusion, the prevalence and associations of ECG abnormalities in AAs with T2D enrolled in the AA-DHS were evaluated. ECG abnormalities were highly prevalent in this population; nearly 60% had at least one minor or major ECG abnormality and 23% had major ECG abnormalities. Female sex and statin use were significantly associated with lower odds of any ECG abnormality, and diabetes duration was significantly associated with higher odds of any ECG abnormality in the multivariable model. Additional studies are warranted to determine whether these ECG abnormalities are independently associated with CVD outcomes in the high risk and understudied AA population with T2D. If these ECG abnormalities aid in the identification of an exceptionally high risk subgroup of patients with diabetes, earlier use of specific cardiovascular interventions may be warranted targeting primary prevention.
Funding
This study was supported in part by the General Clinical Research Center of the Wake Forest School of Medicine grant M01 RR07122; and grants RO1 HL092301 (Donald W. Bowden) and RO1 DK071891 (Barry I. Freedman).
Conflict of interest
None.
Acknowledgements
The investigators acknowledge the cooperation of our participants and study recruiter Cassandra Bethea. The authors report no conflicts of interest.
References
Cite this article
TY - JOUR AU - Matthew B. Sellers AU - Jasmin Divers AU - Lingyi Lu AU - Jianzhao Xu AU - S. Carrie Smith AU - Donald W. Bowden AU - David Herrington AU - Barry I. Freedman AU - Elsayed Z. Soliman PY - 2014 DA - 2014/05/24 TI - Prevalence and determinants of electrocardiographic abnormalities in African Americans with type 2 diabetes JO - Journal of Epidemiology and Global Health SP - 289 EP - 296 VL - 4 IS - 4 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2014.04.003 DO - 10.1016/j.jegh.2014.04.003 ID - Sellers2014 ER -
