COVID-19 and Comorbidities: Audit of 2,000 COVID-19 Deaths in India
 , Shahul H. Ebrahim2, *,
, Shahul H. Ebrahim2, *,  , Lekha D. Bhat3, Bindhya Vijayan4,
, Lekha D. Bhat3, Bindhya Vijayan4,  , Salman Khan4, Soji D. Jose4, Zarin Pilakkadavath5, Premini Rajeev6, Jinbert L. Azariah4
, Salman Khan4, Soji D. Jose4, Zarin Pilakkadavath5, Premini Rajeev6, Jinbert L. Azariah4- DOI
- 10.2991/jegh.k.210303.001How to use a DOI?
- Keywords
- SARS-CoV; mortality; India; hypothyroidism; death audit
- Abstract
Background: On September 5, 2020, India reported the second highest COVID-19 cases globally. Given India’s unique disease burden including both infectious and chronic diseases, there is a need to study the survival patterns of COVID-19. We aimed to describe the factors associated with COVID-19 deaths in the State of Tamil Nadu that has the highest COVID-19 case burden among the Indian states, and to compare deaths among COVID patients with and without comorbidities.
Methods: We analyzed the first 1000 COVID deaths (1 March to 26 June 2020) and 1000 recent deaths at the time of analysis (1–10 August 2020). We examined data on facility (public vs private), age, gender, duration of illness prior to and/or during hospitalizations, symptoms, comorbidities and cause of death. We used R statistical program to do the analysis. We compared deaths among patients with and without comorbidities using Wilcoxon rank sum test. p < 0.05 was considered significant.
Results: First, we found a shorter time interval from onset of symptoms to death in India than that was reported in the USA and China. Second, young adults without comorbidities had shorter survival from the time of onset of symptoms irrespective of their timing of hospitalization. Third, hypothyroidism is a COVID-19 associated co-morbidity. Longitudinal studies are needed to further assess the thyroid-COVID-19 link.
Conclusion: As COVID-19 infection rates are accelerating rapidly in India, it is crucial to sensitize young adults while protecting the elderly and other vulnerable populations.
- Copyright
- © 2021 The Authors. Published by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
On August 30, 2020 India reported world’s highest single day increase in COVID-19 cases, and by September 5th, India reached the second highest tally globally, with over 2600 cases per million and a case fatality rate of 1.75% [1]. Unlike the countries affected earlier with this pandemic that have undergone the epidemiologic transition, India still faces dual burden of infectious and chronic disease challenges. This, coupled with poverty, suboptimal health care access, disease transmission enablers (such as internally displaced migrant populations; and adverse weather events that compromises mitigation, access to care, and care delivery) make the situation further complex. Such a challenging pandemic environment calls for the assessment of the natural history of COVID-19 and outcome in the Indian context. Therefore, we aimed to describe the factors associated with COVID-19 deaths in the State of Tamil Nadu (population, 78 million), that has the highest COVID-19 case burden among the Indian states [1,2]. We also specifically compared deaths among COVID patients with and without comorbidities.
2. METHODS
In this report we used public access data from 2000 COVID-19 deaths and describe factors associated with COVID-19 deaths in the State of Tamil Nadu. Tamil Nadu government releases daily bulletins related to COVID [2]. Information on COVID-19 deaths include the type of facility (public vs private), age, gender, duration of illness prior to and/or during hospitalizations, symptoms, comorbidities and cause of death. We abstracted data on the first 1000 deaths (1 March to 26 June, 2020) and 1000 recent deaths at the time of analysis (1–10 August, 2020).
We describe continuous variables such as age and time-to-events as median and interquartile range (IQR) and categorical variables like sex and age groups as proportions. We used Chi-square test to compare categorical variables and Wilcoxon rank sum test for continuous variables. p < 0.05 was considered significant. We used R statistical program to do the analysis.
3. RESULTS
Of the 2000 deaths, two-thirds of the diseased were male (73%) and treated in public facilities (72%). The median age at death was 64 years (IQR 17, range 4–97 years). Overall, median days from the onset of symptoms to death was 4.6 days, (IQR 7.1, range 0–100). Of all the 2000 patients brought to the hospital, 0.8% (15) were dead on arrival, 4% died within an hour, 20% died within 24 h, and 25% died between 1 and 3 days of hospitalization. Among the 1985 persons who died in the hospital, median days from onset of symptoms to hospitalization was four (IQR 5, range 0–30), and from hospitalization to death was 3.6 days (IQR 6.2, range 0–98.4).
Acute respiratory distress syndrome subsequent to pneumonia was the most commonly recorded immediate cause of death (54%). 624 cases had information on symptoms of whom 39% had three concurrent symptoms (dyspnea, fever, cough), and 16% had single symptoms. The leading symptoms were dyspnea (77%), followed by fever (75%) and cough (55%). Only four people had reported loss of taste and two had reported loss of smell.
Overall, 96% of the cases were recorded as having comorbidities. Among those with specific mention of the type of comorbidity, 71% had multiple comorbidities: (≥4 comorbidities, 7%; ≥3, 20%; ≥2, 29%). Most common comorbidities include diabetes (66%), hypertension (54%), coronary artery disease (18%), and chronic kidney disease (15%). Hypothyroidism was present among 4% (Figure 1). Asthma prevalence in this cohort (3%) is smaller than the 5.5% population prevalence reported for India [3]. The prevalence of comorbidity and concurrence of comorbidities increased with age; 60% of those aged 60 years or older had at least one comorbidity compared to 6% of those aged 40 years or younger (χ2 = 61.9, p < 0.0001). People without comorbidities were on an average 12.4 years younger than those with comorbidities.
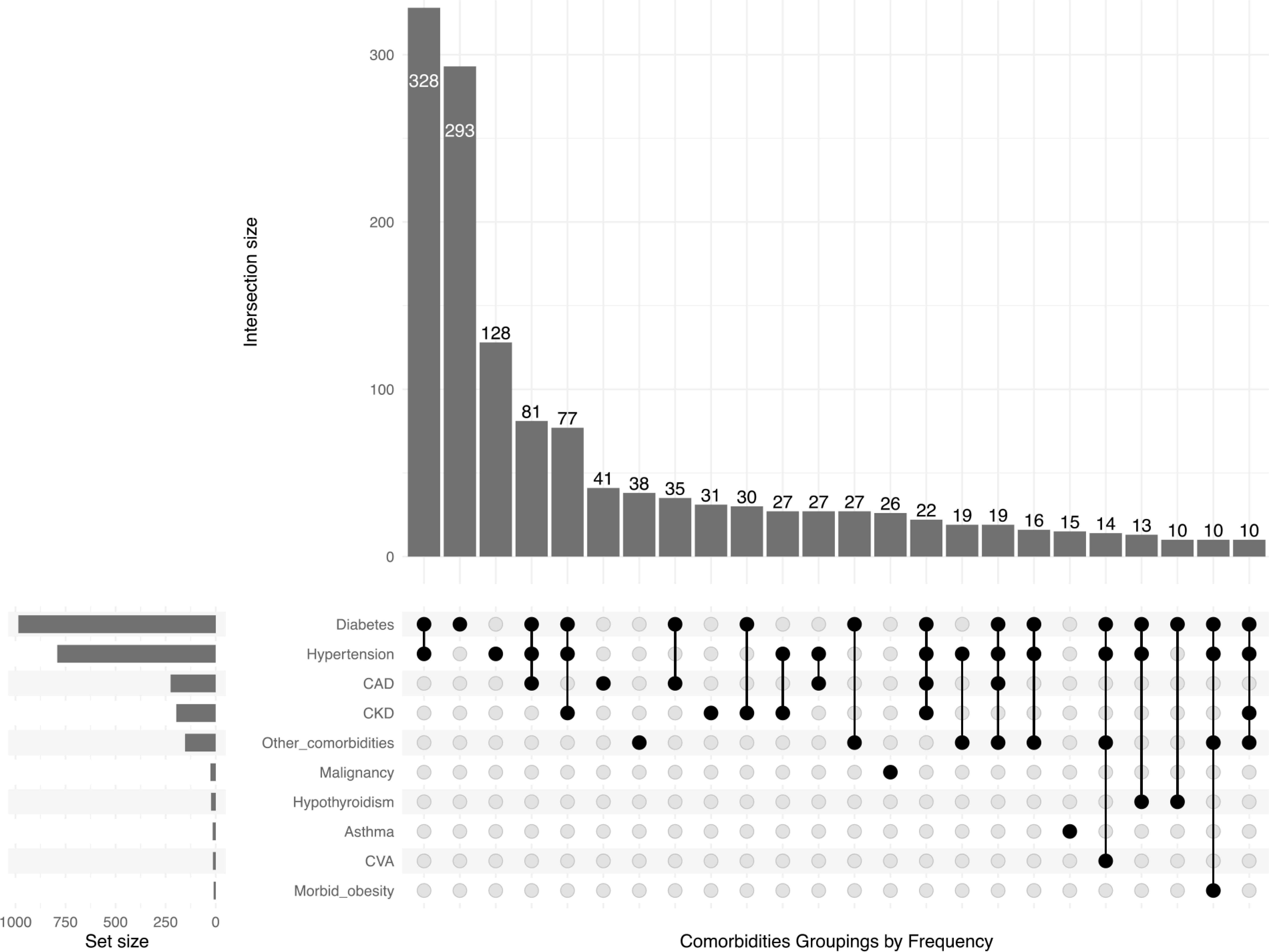
Co-occurrence of comorbidities among 2000 COVID 19 deaths, Tamil Nadu, India*. *Co-occurrences with less than 10 counts are excluded from the figure to decongest the vertical bars. CAD, coronary artery disease; CKD, chronic kidney disease; CVA, cerebrovascular accident.
Median number of days of survival of the patients (the from onset of symptoms) without comorbidities was shorter by 1.8 days than the patients with comorbidities (Table 1) even though there was no delay in hospitalization between the two groups.
| Factors | Comorbidities | No comorbidities | Significance# |
|---|---|---|---|
| Age in years [Median (IQR)] | n = 1918 | n = 82 | Test statistic = 40451 |
| 65 (17) | 53 (16.8) | p = 8.63e−14**** | |
| r = 0.16 | |||
| Time from symptom onset to hospitalization in days [Median (IQR)] | n = 506 | n = 16 | Test statistic = 4212 |
| 4 (4) | 4 (4.25) | p = 0.78 | |
| r = 0.01 | |||
| Time from symptom onset to death in days [Median (IQR)] | n = 1918 | n = 82 | Test statistic = 67507 |
| 4.7 (7.2) | 3.3 (6.4) | p = 0.0297 | |
| r = 0.05 | |||
| Time from hospitalization to death in days [Median (IQR)] | n = 1918 | n = 82 | Test statistic = 69709 |
| 3.6 (6.2) | 2.8 (5.5) | p = 0.08 | |
| r = 0.04 |
Wilcoxon rank sum test using R statistical program, p < 0.05 is considered significant, ****p < 0.0001.
Comparison of COVID-19 deaths with and without comorbidities, India
The first 1000 deaths occurred within a span of 118 days, whereas the last 1000 occurred within a span of 10 days, the period of exponential progression of the epidemic in India. We found no other significant variation in characteristics between two time periods we studied.
4. CONCLUSION
This first analysis of the largest sample of COVID-19 deaths in India revealed three distinct findings. We found a shorter time interval from onset of symptoms to death in India than that was reported in the USA (symptom onset to death, 10 days; hospitalization to death, 5 days [4]) and China [5]. Young adults without comorbidities had lesser days of survival from the time of onset of symptoms irrespective of their timing of hospitalization. While general health care access issues, individual level health care seeking behaviors, and perception among young adults regarding COVID-19 severity with old age and comorbidities may have contributed to some of these observed findings, case control studies are needed to discern if other factors play a role. The finding that hypothyroidism as a COVID-19 associated co-morbidity and the high burden of hypothyroidism in India [6] (prevalence: about one out of 10) offers opportunity to further elucidate the preliminary findings of a potential link between SARS-CoV-2 and thyroid function [7,8]. A meta-analysis has also shown the enhanced risk for severe COVID-19 among hypothyroid patients [9].
Underreporting of comorbidities, stigma- and recall bias-related inconsistencies on self-reported timing of symptoms and days of illness, variable documentation by reporting clinicians are inherent limitations of such data sources. Yet, given India’s diversity in socio-demographics and ethnicity of the population, such quick analysis of large-scale health care administrative data from different geographical regions can help highlight new research priorities, and usefully inform care and control efforts in India and in countries that face similar challenges. As COVID-19 infection rates are accelerating rapidly in India, it is crucial to sensitize young adults and their health care providers on COVID-19’s impact on young adults so that they benefit from early and adequate access to medical care. Doing so will also help prevent COVID-19 transmission to the elderly and other vulnerable populations.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
SFK and SHE identified the data source and designed the analysis. BV, SK, SDJ, ZP and PR abstracted the data; BV and JLA verified data entry; and LDB provided contextual information and SFK conducted the statistical analysis. SHE finalized the draft for publication with comments and contributions from all authors.
FUNDING
No financial support was provided.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Shaffi F. Koya AU - Shahul H. Ebrahim AU - Lekha D. Bhat AU - Bindhya Vijayan AU - Salman Khan AU - Soji D. Jose AU - Zarin Pilakkadavath AU - Premini Rajeev AU - Jinbert L. Azariah PY - 2021 DA - 2021/03/09 TI - COVID-19 and Comorbidities: Audit of 2,000 COVID-19 Deaths in India JO - Journal of Epidemiology and Global Health SP - 230 EP - 232 VL - 11 IS - 2 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.210303.001 DO - 10.2991/jegh.k.210303.001 ID - Koya2021 ER -
