Retrospective Study of Bone-TB in Oman: 2002–2019
 , Raqiya Al Mamari2, Khalfan Almazroui3, Ali Al Habsi3, Ahmed Kamona2, Huda AlHarthi3, Areej I. Al Lawati4, AlZahra H. AlHusaini5
, Raqiya Al Mamari2, Khalfan Almazroui3, Ali Al Habsi3, Ahmed Kamona2, Huda AlHarthi3, Areej I. Al Lawati4, AlZahra H. AlHusaini5- DOI
- 10.2991/jegh.k.210420.002How to use a DOI?
- Keywords
- Tuberculosis; extra-pulmonary tuberculosis; Bone-TB; Oman
- Abstract
Objective: Little information is available about the etiology, pathophysiology, risk factors, and epidemiologic features of Bone Tuberculosis (Bone-TB). In this work, we present the epidemiological data about the Bone-TB in the Sultanate of Oman.
Methods: Retrospectively, we identified and assessed those patients who were diagnosed with Bone-TB between January 2002 and December 2019 at Khoula Hospital. The following data were collected: demographics, clinical presentation, anatomical location, diagnosis, and treatment of the Bone-TB.
Results: During the study period, 115 cases of Bone-TB were diagnosed. Males were affected more than females (57.4% and 42.6%, respectively). About 30% of Bone-TB cases were primary diagnosed in other organs particularly the lungs and then after disseminated to the bone. However, the Bone-TB was detected in hip, leg, hand, shoulder, and skull bones, the most detected Bone-TB was in spine (66% of cases). After vaccination the Bacillus Calmette–Guérin (BCG) strains were identified in the bones of eight babies. Tubercle bacilli were detected by Acid-Fast Stain (AFS) in 59% of cases, and the rest of cases were confirmed using polymerase chain reaction (PCR) tests. There are two used treatment regimens, with 12.4% relapse. The gastrointestinal tract (GIT) disturbances were the most related side effects. The resistance has been detected to pyrazinamide in six cases, rifampicin in three cases, and isoniazid, streptomycin and kanamycin were detected in one case.
Conclusion: The most predominant Bone-TB cases were spine-TB that were mainly disseminated from the lungs. AFS failed to detect tubercle bacilli in 40% of cases. There is no statistical significance in relapse between the used two regimens. The death was predominant among skull-TB cases.
- Copyright
- © 2021 The Authors. Published by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Tuberculosis (TB) is a major public health issue and is one of the top 10 causes of death from a single infectious agent. According to the World Health Organization (WHO Global tuberculosis report, 2019 [1]), it infects around 10 million people worldwide. In 2018, WHO reported 1.2 million TB deaths globally with an extra 251,000 deaths among Human Immunodeficiency Virus (HIV) positive people. TB is a multisystem infectious disease; it can affect any tissue or organ, except the hair and nails [2]. TB is caused by Mycobacterium tuberculosis complex that causes chronic necrosis characterized by the formation of granulomatous lesions in the affected tissues [3]. The disease has two conditions: latent infection and active disease; active disease can be developed in approximately 10% of the infected patients [4].
Tuberculosis can infect any or all organs, however, lungs remain the most affected organ (85%) with Pulmonary TB (PTB) being the most common TB with great epidemiological significance [3–5]. Extra-PTB (EPTB) includes TB that infects organs other than the lung parenchyma, such as the pleura, lymph nodes, skin, meninges, abdomen, gastrointestinal tract (GIT), genitourinary tract, joints, and bones [2,3]. The dissemination of TB to infect other organs extra-pulmonary depends on associated diseases, ethnicity, and compromised immune system [3,6]. Although the primary mycobacterial infections remain dormant without disease development, the suppressed immune system accelerates its reactivation [7–9]. As a consequence, the risk of EPTB increases with advancing immunosuppression. For instance, EPTB can be seen in more than 50% of patients with AIDS [10]. The increased incidence of EPTB lies to some extent in the difficulty of its diagnosis, resulting in a delay in diagnosis and severe sequelae [6,10,11].
Bone and joint TB is an ancient disease, osteoarticular-TB has been identified in Egyptian mummies [12,13], Europeans’ skeletons in the Middle Ages [14], and even earlier in Iron Age remains from Asia [15]. M. tuberculosis is the most common cause of mycobacterial osteomyelitis and arthritis [16]. Nontuberculous Mycobacterial (NTM) skeletal infections are usually associated with a previous puncture, injury, or with orthopedic surgery [16]. NTM is very rare but has increased with the increase in AIDS prevalence [17]. Recently, Mycobacterium bovis skeletal infections have been observed after intravesical therapy with Bacillus Calmette–Guérin (BCG) therapy [18,19].
According to WHO, in 2018, the incidence of TB in the Sultanate of Oman was estimated as 5.9 per 100,000 population and mortality rates of 0.37 per 100,000 population. Although there are many reports describing Bone Tuberculosis (Bone-TB) infections, and their increasing prevalence in developing countries [20–24]. There were few publications on TB and its elimination in Oman [25–30], and no publications on Bone-TB until the date of writing this work. In this report, we studied retrospectively Bone-TB cases in Oman referred from the whole country to Khoula hospital, in the period of 2002–2019. We investigated the demographics of the cases, the transmission and anatomical distribution of the disease, the diagnosis, and treatment regimens.
2. MATERIALS AND METHODS
This study was conducted at Khoula Hospital, Muscat, Sultanate of Oman, a tertiary care facility that was chosen as an educational center recognized by the Royal Society of Orthopedics and Neurosurgery. It is one of the distinguished health institutions in the provision of specialized health care and high quality in many fields including orthopedics, hand surgery, spinal surgery, and neurosurgery. A retrospective study was conducted to identify and assess those patients who were diagnosed with Bone-TB between January 2002 and December 2019. After receiving approval from the Institutional Review Board, we collected the patients’ data including demographics (age, sex, and nationality), patients’ histories, diagnosis, clinical presentation, anatomical location of Bone-TB, and treatment regimens. The collected data were entered into a spreadsheet and analyzed using GraphPad Prism 8 software.
3. RESULTS
3.1. Demographic Characteristics
During the study period, 115 cases from Muscat and other regions were diagnosed as Bone-TB cases (Figure 1). Generally, males were affected more than females (57.4% with average age 41.5 years and 42.6% with average age 32.5 years, respectively) (Figure 1A). The patients were distributed according to age and sex (Figure 1C), the highest diagnosed cases were in the age range of 19–40 years. Despite that about 88% of cases were Omani (Figure 1B), the higher number of diagnosed cases were observed in years 2015–2017 especially among expatriates from India (11th on TB burden countries list according to WHO Global tuberculosis report, 2019 [1]) (Figure 1D).
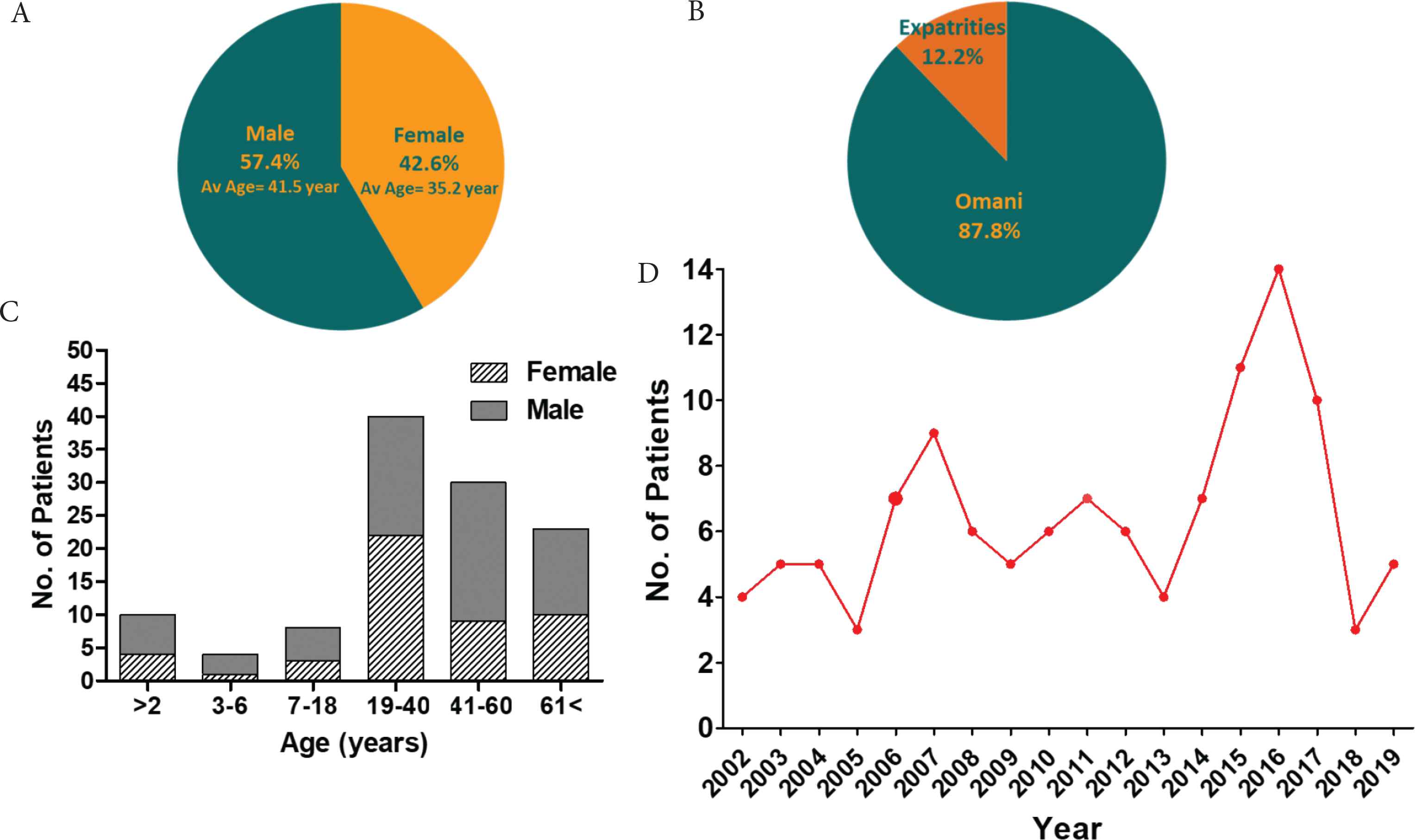
Demographic characteristics and the prevalence of Bone-TB cases. (A) The sex and average age of the cases. (B) The nationality of the cases. (C) The distribution of the cases according to age and sex. (D) The prevalence of cases in the period of 2002–2019.
3.2. Bone-TB Transmission
The transmission of Bone-TB was represented in Figure 2. By taking patients’ histories, we found that 28.7% (33 out of 115 cases) of Bone-TB cases were primarily TB-diagnosed in other organs and then disseminated to bone (Figure 2B). Consequently, about 39% of pulmonary-TB cases were disseminated to infect bone, particularly spine bones. It was observed that 100% of testicular, fallopian, ovarian, and urinary tract-TB cases disseminated to Bone-TB. Meanwhile, seven out of nine (77.8%) CNS-TB diagnosed cases developed Bone-TB in later stages and one out of two (50%) lymph nodes-TB cases disseminated to the bone. Interestingly, seven cases (6.1%) were among the medical team who acquired TB-Bone from their continuous and unsafe contact with patients. Most of these cases (six out of seven cases) were primarily respiratory tract infected and then disseminated to the bone. In the same context, five patients (4.3%) acquire TB after accidental use of contaminated tools or after trauma which leads to dissemination of TB to bone. About 5% of cases acquired TB from long contact with their family members, which was primarily transmitted by droplets or using patients’ tools. Surprisingly, eight cases (7%) were infected by TB after BCG vaccine. It is worthy to mention that about 49% of cases were not previously diagnosed as TB cases and were diagnosed as Bone-TB for the first time with an unknown transmission method.
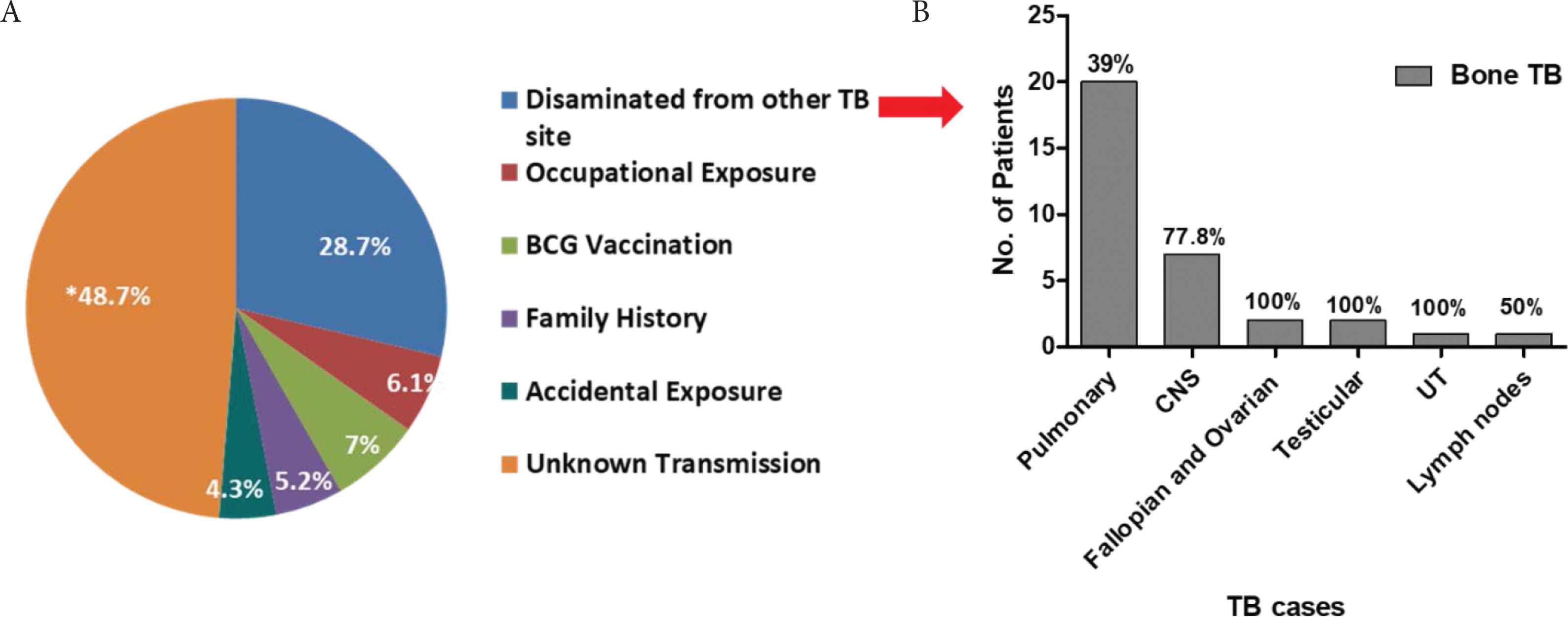
Bone-TB transmission. (A) The mode of Bone-TB transmission from the patients’ histories. (B) The numbers and percentages of Bone-TB cases disseminated from other infected sites. (*) Unknown transmission or not previously diagnosed as TB case and first time diagnosed as Bone-TB.
3.3. Anatomical Distribution of Bone-TB
The percentages of affected bones by TB were represented in Figure 3 and the detailed anatomical distribution was shown in Table 1 among male and female cases.
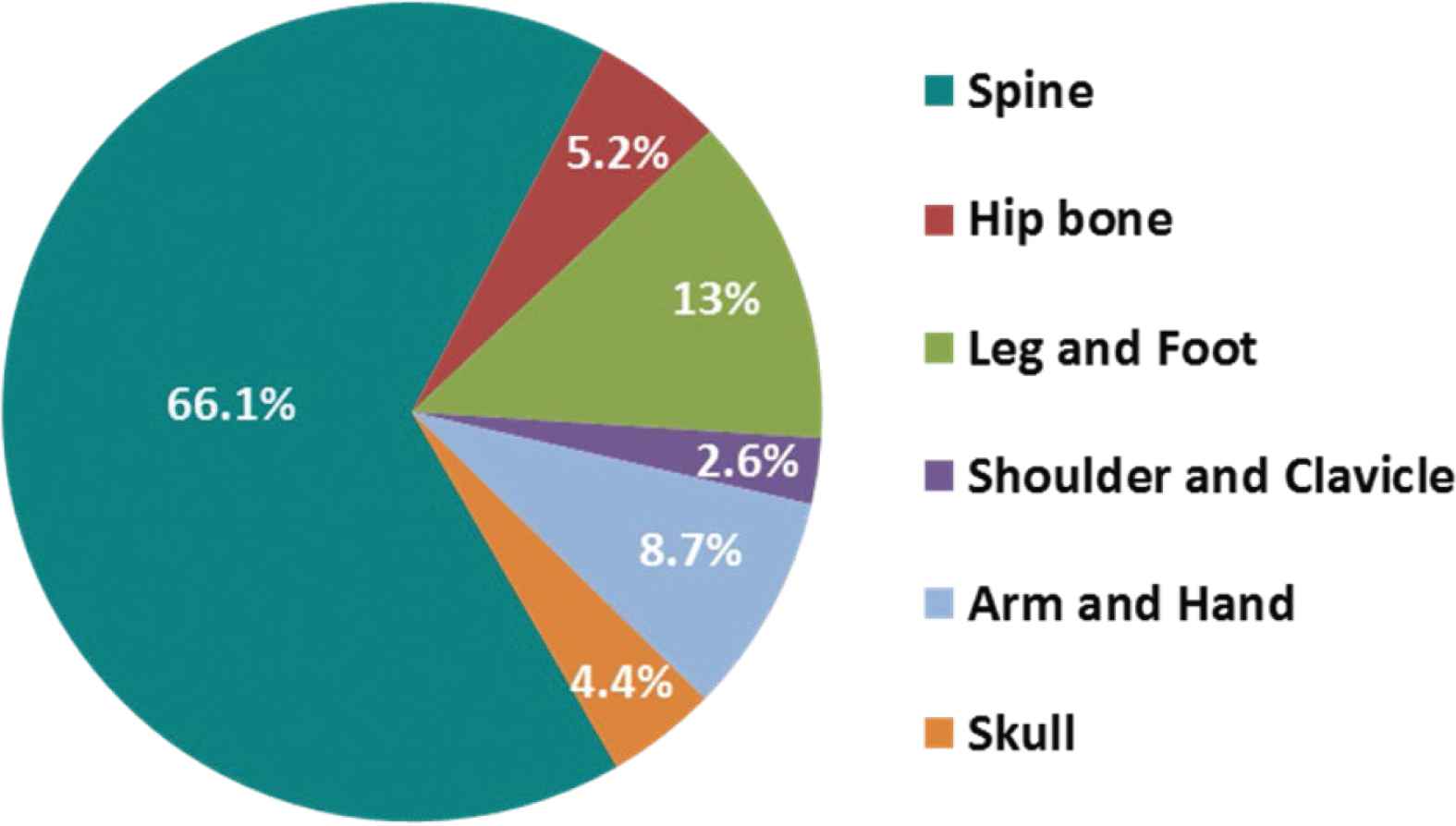
Anatomical distribution of Bone-TB.
| Bone | No. of patients/Av. age (years) | Female/Av. age (years) | Male/Av. age (years) |
|---|---|---|---|
| Spine | |||
| Cervical | 6/49.5 | 2/62.5 | 4/43 |
| Cervicodorsal | 4/40 | 1/19 | 3/47 |
| Dorsal | 25/29.3 | 9/31.1 | 16/38.9 |
| Dorsol-lumbar | 14/50.9 | 8/48.3 | 6/61 |
| Lumbar | 16/40.4 | 8/32.2 | 8/48.6 |
| Lumbosacral | 6/60.3 | 3/53 | 3/67.7 |
| Sacroiliac | 3/27.3 | 3/27.3 | 0/0 |
| Iliac | 2/48.5 | 1/32 | 1/65 |
| Hip bone | 6/47.7 | 4/51.7 | 2/39.5 |
| Leg and foot | |||
| Femur | 3/45.6 | 1/73 | 2/32 |
| Femur/Knee | 4/42.75 | 0/0 | 4/42.75 |
| Tibia/Knee | 3/0.97 | 2/0.95 | 1/1 |
| Tibia/Fibula | 1/40 | 0/0 | 1/40 |
| Tibia | 1/0.5 | 0/0 | 1/0.5 |
| Tibia/Ankle | 1/67 | 1/67 | 0/0 |
| Foot | 2/36.5 | 1/63 | 1/10 |
| Shoulder | 3/42.7 | 1/86 | 2/21 |
| Arm and hand | |||
| Humerus and Elbow | 3/1.7 | 2/2 | 1/1 |
| Radius | 5/12.4 | 0/0 | 5/12.4 |
| Carpus and wrist | 2/48 | 0/0 | 2/48 |
| Skull | 5/41.4 | 2/41 | 3/42 |
Anatomical distribution of Bone-TB
3.3.1. Spine-TB
Spine-TB was detected among 66% of cases. However, with a higher incident rate in males (41) compared to females (35), however, it was diagnosed at a younger age in females than males. It is more prevalent in dorsal and lumbar parts, while sacral and cervical vertebra were the least affected. Additionally, dorsal and sacroiliac-TB was observed in younger ages and TB in the dorsal-lumbar region was observed in higher Body Mass Index (BMI), especially among females. While sacroiliac-TB was observed only in females not males, TB in the dorsal-lumbar and cervical region is more prevalent in males than females. Kyphosis was observed in five cases, and 10% of cases were diagnosed with neurological deficits and needed surgical intervention in addition to drug treatment.
3.3.2. Hipbone-TB
This was more prevalent among young females (four out of six cases) than males. Moreover, it was observed in obese females (average BMI: 35). From patients’ history, one case was disseminated from fallopian tubes, while the other from pulmonary-TB. Interestingly one case was diagnosed as BCG strains in a baby (below 2 years). Most cases were diagnosed as arthritic-TB (five out of six cases), and pyomyositis and septic joint infection were observed in one case.
3.3.3. Leg and foot-TB
This was more prevalent in males than females. Eight cases were disseminated to involve bone and joints (arthritic-TB) and were observed in obese males and females (BMI > 32). The most prevalent TB was observed in the femur and knee (seven cases), while the least diagnosed TB was in foot bones (two cases). Clinically, three patients were diagnosed with tenosynovitis in ankle and knee and two patients suffered from bursitis due to knee-TB. Moreover, Tibia-TB was more observed in babies below 2 years old (four out of six cases). Interestingly, five cases were diagnosed as BCG strains in ages below 2 years.
3.3.4. Shoulder-TB
Three cases were disseminated from pulmonary or lymph nodes to bones of the shoulder (the scapula and the clavicle). Arthritic-TB was observed in three cases, while only one of these cases was diagnosed with pyomyositis. BCG strain was isolated in one baby below 2 years with the diagnosis of arthritic-TB in the shoulder.
3.3.5. Arm and hand-TB
This was more prevalent in males (eight cases) than in females (two cases). Cases were clinically and radiologically diagnosed osteomyelitis and arthritis, only one case was bacterial infection to develop pyomyositis and bursitis. Carpus and wrist-TB (two cases) with tenosynovitis were observed only in expatriates. One Radius-TB case was observed after vaccination with BCG at the age of below 2 years.
3.3.6. Skull-TB
Five cases were disseminated from CNS-TB, four of them were diagnosed as sequelae of TB meningitis accompanied by epidural infections. All cases were considered as relapsed TB cases after failure to pulmonary TB treatments. It is worth mentioning that the difficulty of sample collection for microbiological and pathological examination makes the radiological methods the main diagnostic tools. Due to clinical considerations and surgical interventions, two cases did not comply with the drug treatment regimens after recommendations of specialists.
3.4. Bone-TB in Immunocompromised Patients
Out of five patients who were primarily HIV patients and were diagnosed with pulmonary-TB, two (40%) of them were found to have Bone-TB. By considering that the immunity of babies and elderly people is weaker than the optimum normal, Bone-TB was observed in 10 cases (below 2 years), eight cases were infected with BCG strains and two cases were disseminated from other sites. Eleven Bone-TB cases were >70 years old, one case was HIV patient and all cases were primarily TB infected in other sites. Moreover, immunocompromising diseases or conditions such as diabetes, chronic lung, kidney and liver diseases, addiction, and alcoholism were identified in 66 (57.4%) of Bone-TB cases.
3.5. Diagnosis of Bone-TB
Routinely the collected samples or biopsies were Acid-Fast Stained (AFS) for microbiological TB diagnosis. While AFS results were positive in 68 (59.2%) cases, the tubercle bacilli were not seen in 42 (36.5%) cases. Due to the difficulty in sample collection from Skull-TB, five cases were not exposed to AFS and were diagnosed by radiological methods. Polymerase Chain Reaction (PCR) diagnostic tools were applied to amplify different TB genes. Surprisingly, in one case which was AFS positive, the TB genes were not amplified by PCR. On the other hand, all AFS negative results were confirmed by PCR.
3.6. Treatment Regimens
During the study period, two regimens were used following the internal protocols for TB and Bone-TB treatments (Table 2). Surgical interventions were applied in parallel to anti-TB therapeutics to 10% of patients when neurological deficit had been observed. The first regimen was used in the treatment of 45 (39.1%) cases, while the second regimen was used for 70 (60.9%) cases. It is noteworthy to mention that the Bone-TB and its complications were considered as the direct cause of death in eight (6.95%) cases. Importantly, therapeutic approaches and/or surgical interventions failed to cure the five cases who were diagnosed skull-TB with a death rate of 100%.
| Regimen 1 | Regimen 2 | ||
|---|---|---|---|
| Phase 1: 3 months (four drugs + Vit. B6) | Isoniazid 300 mg/OD | Phase 1: 2 months (four drugs + Vit. B6) | Isoniazid 300 mg/OD |
| Rifampicin 450 mg/OD | Rifampicin 450 mg/OD | ||
| Ethambutol 1.2 g/OD | Ethambutol 1.2 g/OD | ||
| Pyrazinamide 1.5 g/OD + Pyridoxine 20 mg/OD | Pyrazinamide 1.5 g/OD + Pyridoxine 20 mg/OD | ||
| Phase 2: 3 months (three drugs + Vit. B6) | Isoniazid 300 mg/OD | Phase 2: 10 months (two drugs + Vit. B6) | Isoniazid 300 mg/OD |
| Rifampicin 450 mg/OD | Rifampicin 450 mg/OD | ||
| Ethambutol 1.2 g/OD + Pyridoxine 20 mg/OD | |||
| Phase 3: 6 months (two drugs + Vit. B6) | Isoniazid 300 mg/OD | ||
| Rifampicin 450 mg/OD | |||
Nb 1. Phase 3 may be extended according to orthopedic surgeon recommendations.
Nb 2. LFT routinely every 6 weeks.
Nb 3. Dose was adjusted according to weight of patients.
OD, once daily.
The used treatment regimens
3.6.1. Compliance to treatment regimens and relapse of TB
About 30% of patients did not comply with the used treatment regimens, the discontinuation of treatment was due to drugs’ and patients’ factors (Figure 4). The exaggerated side effects and resistance to TB drugs represented 44% and 29.5% of non-compliant patients, respectively. The serious patients’ health conditions due to major surgical operations or incapability to administrate the treatment was also reported in about 12% of non-compliant patients. Unfortunately, about 15% of non-compliant patients either did not follow or rejected to continue the treatment (Figure 4B). The compliance to each regimen did not vary greatly between the two regimens (68% and 71%, respectively) (Figure 4A and 4C). The most reported side effects to the prescribed medications were summarized in Table 3 and represented in each regimen in Figure 4D.
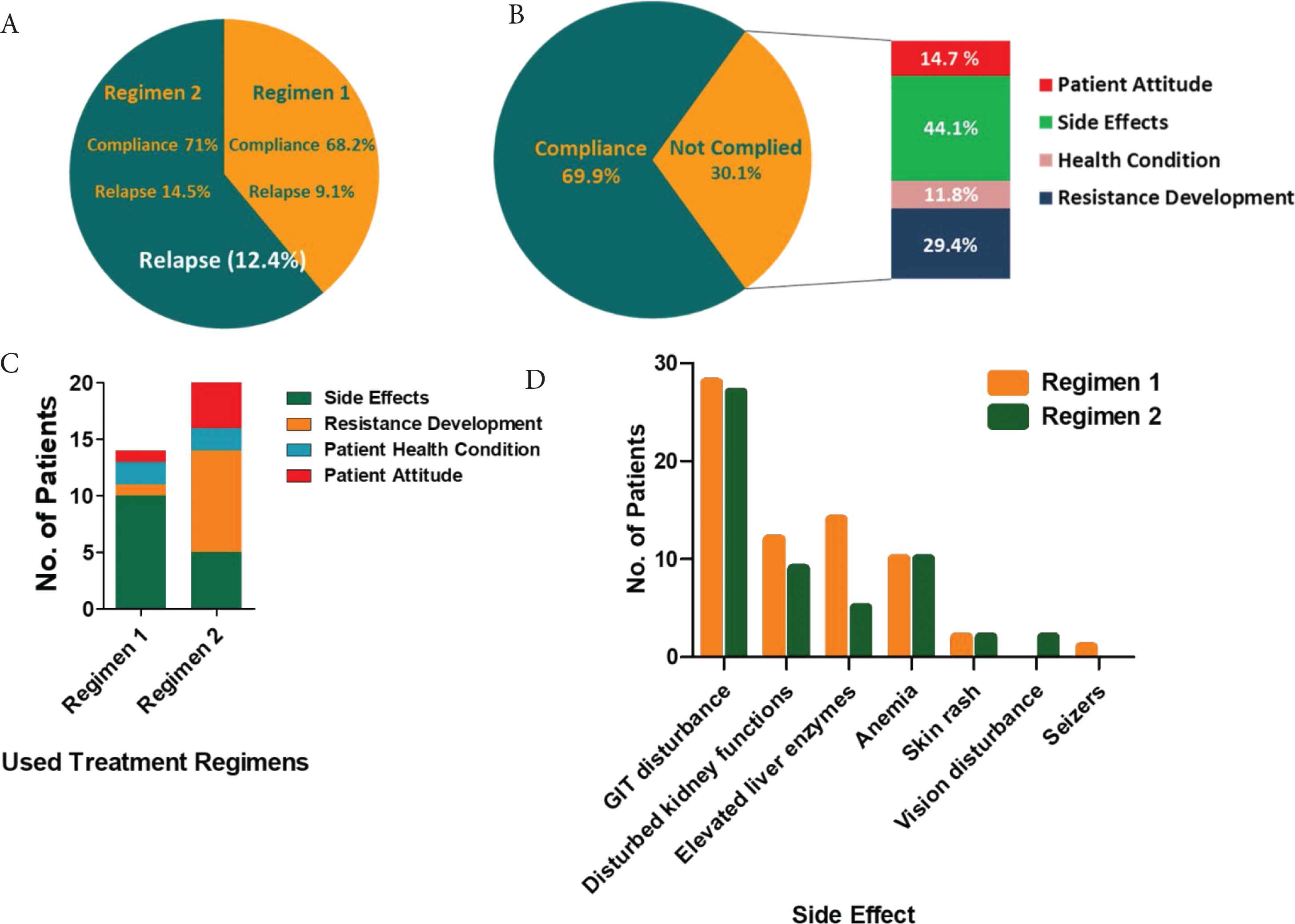
Compliance to TB treatment used regimens. (A) Compliance to the used regimens and percentage of relapse. (B) The causes of non-compliance to used treatments. (C) The causes of non-compliance to each used regimen. (D) The most observed side effects in both regimens.
| Side effects | No. of cases | Notes |
|---|---|---|
| Gastritis/GIT disturbance | 55 | Vomiting was observed in three cases |
| Constipation was observed in two cases | ||
| Disturbed kidney functions | 21 | Streptomycin-induced nephrotoxicity in one |
| Elevated liver enzymes | 19 | Isoniazid-induced hepatotoxicity in five cases |
| Pyrazinamide-induced hepatotoxicity in two cases | ||
| Anemia/lowered HB | 20 | Lowered HB improved after stop of treatment |
| Skin rash | 4 | Relief by time |
| Ototoxicity | 1 | Streptomycin-induced ototoxicity in one case |
| Vision disturbance | 2 | Ethambutol-induced visual disturbances and pain of eye in two cases below 7 years old |
| Seizers | 1 | Ethambutol-induced seizers in one case |
The most observed side effects to the used treatments
3.6.2. Relapse of TB and resistance development to anti-TB drugs
Relapse was observed in about 12.4% of total cases, with 9% and 14.5% of patients treated with two regimens respectively. Chi-square test (GraphPad Prism 8 software) was used to compare the relapse in the used two regimens. Chi-square was not statistically significant (p = 0.45); indicating that there was no significant difference in relapse in the used regimens. Interestingly, five out of 14 relapsed patients were compliant to treatment regimens, two of five cases were HIV patients. Among non-compliant patients, nine cases showed TB relapse, either due to drug resistance development (three cases) or discontinuation of the treatment (six cases). While the pyrazinamide resistance was detected in six patients, the resistance to rifampicin was identified in three patients. Three of the identified BCG strains developed resistance to both pyrazinamide and rifampicin. Interestingly, one case was resistant to rifampicin, isoniazid, streptomycin, and hanamycin (Table 4).
| Drugs | No. of resistant cases | Notes |
|---|---|---|
| Pyrazinamide | 6 | Three out of six cases were BCG strains |
| Rifampicin | 3 | One out of three cases was BCG strains |
| Isoniazid | 1 | One case was resistant to rifampicin + isoniazid + streptomycin + kanamycin |
| Streptomycin | 1 | |
| Kanamycin | 1 |
The observed resistance to the used anti-TB drugs
4. DISCUSSION
Millions of people contract TB each year, making it a major public health issue globally. Despite the low numbers of TB cases in Oman (WHO Global tuberculosis report, 2019 [1]), the efficient documentation facilitates the follow-up by the medical teams. While, all TB complicated cases are referred to tertiary care centers as routine, Bone-TB cases are directed to Khoula hospital. In this study, we retrospectively reviewed all the referred Bone-TB cases (115 cases) from all of Oman to Khoula hospital.
Bone-TB was not greatly varied between males and females (57.5% and 42.5%, respectively); however, we observed the highest incidence of Bone-TB in ages 19–61 years and in females more than males. Following these observations, the highest TB rates were observed in ages between 25 and 64 years [31]. Although there is no real correlation between dissemination of TB and age reported, we can assume higher Bone-TB cases disseminated from other infected sites in immunocompromised elderly patients.
Surprisingly, Bone-TB was diagnosed in 10 babies below 2 years, and the isolated strains were of BCG strains. Moreover, the developed Bone-TB was detected anatomically near injection sites especially in the thigh region. Regional bone infections such as BCG osteomyelitis or osteitis and disseminated BCG infections are rare complications of BCG vaccination [32]. BCG vaccine should be intradermally injected, but if given subcutaneously, it may spread to the regional lymph nodes, causing either suppurative or nonsuppurative lymphadenitis [32]. On the other hand, cold abscesses are the most significant clinical presentation of the erroneous administration of the BCG vaccine when intramuscularly injected into the thigh [33].
Tuberculosis is an extremely contiguous disease and can infect all organs. In the current study, we observed the dissemination of TB to infect bone in 57.5% of immunocompromised or chronic patients. PTB is the most common TB [5], Bone-TB was diagnosed in 40% of the referred PTB cases to Khoula hospital. However, 50% of the TB transmission to bone cases were not documented or traced, but we observed few Bone-TB cases in TB patient’s family members, among medical team co-workers, and even accidentally after trauma.
Bone-TB anatomical distribution was represented in detail (Table 1 and Figure 3). Pott’s disease is spinal tuberculosis, it spreads through hematogenous route from other sites, often the lungs. Pott’s disease is the most common extrapulmonary manifestation of TB associated with constitutional symptoms, tenderness, back pain, paraplegia, and scoliotic or kyphotic deformities [16,34–36]. It accounts for 2% of all TB cases, 15% of EPTB, and 50% of skeletal-TB [34,36]. In compliance with these results, spine-TB was diagnosed in 66% of all Bone-TB cases. Moreover, most cases were detected in the dorsal-lumbar region, as an implication of hematogenous spread from the lungs. Furthermore, Bone-TB was diagnosed in the foot, hand, skull, hipbone, shoulder, and clavicle as is described in detail in the “Results” section.
The delayed or even missed diagnosis of EPTB in general and Bone-TB in particular is often owed to insidious clinical manifestations and/or poor performance of diagnostic tools [35,37–40]. However, culturing and AFS of Mycobacterium species are classical gold standards for TB diagnosis and technical and logistical restrictions in Bone-TB cases are increasingly recognized [39,40]. In the current work, AFS failed to diagnose 42% of cases because of the difficulty of sample collection or event failure in staining or culturing of the microbe. PCR is significantly used for an early diagnosis of EPTB, in spite of high variations in its results. However, there are different gene targets, IS6110 followed by 16S rRNA genes encoding MPB-64 proteins are the most widely used gene targets [37]. Multiplex PCR, in which two or more genes are targeted, is used to diagnose many suspected cases, when conventional microbiological tests fail [19,37,41,42]. In this study, it was observed that all AFS negative cases were diagnosed by Multiplex PCR. Although the incapability of PCR to differentiate between viable and nonviable Mycobacterium, PCR results plus clinical diagnosis along with histopathology if affordable are adequate to initiate anti-TB treatment [19,34,37,38].
The Bone-TB is protracted through three stages over 3–5 years: onset, destruction, and the last stage of repair and ankyloses resulting in high morbidity and mortality [43,44]. Anti-TB chemotherapy achieved dramatic resolution of TB lesions. The chemotherapeutic treatment of TB is aimed to cure the individual patient, minimize the risk of death, decrease the transmission to other people and prevent the development of drug resistance during therapy course [44–46]. The resistance to anti-TB is a global health threat with increasing incidence worldwide [44]. Anti-TB resistance is developed when treatment regimens are not properly administered or adhered to, it occurs also as a result of biological variations in drug uptake or substandard drugs [44,47–49]. Multidrug-resistant (MDR) TB includes the resistance to at least two of the most effective anti-TB drugs, isoniazid, and rifampicin. Extensively Drug-resistant (XDR) TB involves an extra resistance to any fluoroquinolone and to any of the second line injectable anti-TB aminoglycosides (amikacin, capreomycin and kanamycin) [44,47].
Multidrug-resistant tuberculosis is an important public health problem and increasing rates are reported globally, in Oman the percentage of MDR-TB increased from 0% in 2017 to 2.9% in 2018 according to the WHO Global tuberculosis report, 2019 [1]. While the WHO Global tuberculosis report documents high resistance to rifampicin in Oman (≥16 data points) between 1995 and 2019, the resistance to rifampicin was detected in six (5.2%) of studied Bone-TB cases. Moreover, resistance to pyrazinamide has been observed in six patients and one case was XDR-TB. Over the period of study, two treatment regimens were used (Table 2). Importantly, about 30% of patients were non-compliant to applied regimens, mainly due to side effects particularly GIT disorders, resistance development, and patients’ attitudes or bad health situations. Interestingly, the second regimen was used as a modification to first regimen and there is no great difference between percentages of patients’ compliance to each regimen, the percentage of relapse in second regimen (14.5%) was higher than relapse to first regimen. The success of treatment of new and relapse cases in 2017 was 51% in Oman according to the WHO Global tuberculosis report, 2019 [1].
In this study, we recognized relapse in 12% of Bone-TB cases. The relapse was observed significantly in non-compliant patients. Furthermore, in this study, surgical intervention is an obligation when the neurological deficit has been observed [50,51], only 10% of cases needed surgical interventions. Despite the presence of all required data saved in electronic files since 2002; there are some limitations of this study. The most important is the difficulty to follow-up foreign patients who left Oman or patients who continue their treatment out of Oman.
In conclusion, we conducted this study to assess the epidemiology of Bone-TB in Oman. We retrospectively collected all the referred Bone-TB cases from the whole country. We found that the most predominant Bone-TB is spine-TB (66%), and mainly disseminated from the lungs. We documented the Bone-TB after vaccination with BCG vaccine in babies below 2 years old. However, AFS is considered the golden diagnostic test for TB, but it was not helpful in the diagnosis of 40% of cases because the difficulty of sample collection from bones or the scanty nature of the microbe itself; that is why PCR testing is mandatory for diagnosis and also for detection of resistance genes. It has been noticed that there is no significant difference in the relapse to the first older regimen and second newer regimen. Interestingly, all the patients who were diagnosed with TB in their skulls died, and treatment or surgical approaches were failed. It has been observed that the non-compliance of patients is mainly due to raised side effects and developed resistance to anti-TB drugs. However, GIT-related side effects are the most observed, kidney and liver function tests and blood pictures must be regularly performed. Monitoring of resistance development is crucial to avoid recurrences and relapses; in this study, the highest resistance was recognized to pyrazinamide (six cases) then rifampicin (three cases).
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
WAAH contributed in study conceptualization and writing (review & editing) the manuscript. RA, KA, AA, AK and WAAH contributed in data curation, formal analysis and writing (original draft). HA, AIA, AHA and WAAH contributed in funding acquisition and project administration. WAAH and RA supervised the project.
FUNDING
No financial support was provided.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Wael A.H. Hegazy AU - Raqiya Al Mamari AU - Khalfan Almazroui AU - Ali Al Habsi AU - Ahmed Kamona AU - Huda AlHarthi AU - Areej I. Al Lawati AU - AlZahra H. AlHusaini PY - 2021 DA - 2021/04/26 TI - Retrospective Study of Bone-TB in Oman: 2002–2019 JO - Journal of Epidemiology and Global Health SP - 238 EP - 245 VL - 11 IS - 2 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.210420.002 DO - 10.2991/jegh.k.210420.002 ID - Hegazy2021 ER -
