Practical solutions for hypertensive patients with dyslipidemia☆
This article was presented as lecture in the symposium on “Protecting arteries against hypertension and dyslipidemia” at the ARTERY 16 Congress in Copenhagen, Denmark (October 13–15, 2016).
- DOI
- 10.1016/j.artres.2017.03.002How to use a DOI?
- Keywords
- ACE inhibitors; Amlodipine; Aortic stiffness; Central pressures; Dyslipidemia; Hypertension
- Abstract
Arterial hypertension and dyslipidemia often coexist and constitute major risk factors of ischemic heart disease. Aggressive treatment of both comorbidities is of paramount importance to decrease global risk. Low adherence is a determinant of poor risk factor control and increases adverse cardiovascular outcomes. Regarding treatment of hypertension, combination therapy is superior in achieving target BP values compared to up-titrating monotherapy and it is recommended in hypertension guidelines. The combined use of drugs in a single pill formulation increases adherence and reduces cardiovascular risk. Our review of the literature indicates that triple therapy with an angiotensin converting enzyme inhibitor, a calcium channel blocker and a statin is associated with a significant reduction in major cardiovascular events. This is attributed to synergy at the vascular, and is translated into efficacy at the clinical level.
- Copyright
- © 2017 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Why should we care?
Hypertension and dyslipidemia are among the leading cardiovascular (CV) risk factors associated with deaths.1 The two conditions frequently coexist. Two out of three hypertensive patients have dyslipidemia and, conversely, half of dyslipidemic patients are hypertensives.2,3 In risk score models, high cholesterol levels doubles the CV risk of hypertensive patients.4 Cardiovascular disease (CVD) is preventable through treatment of risk factors; however, managing global CV risk has received less attention compared with treating individual diseases that affect CV risk, such as hypertension or hypercholesterolemia.
One out of three hypertensive patients are already treated with more than three antihypertensive drugs.5 In spite of the introduction of drugs that can efficiently reduce blood pressure (BP) and cholesterol levels, a considerable proportion of patients with established CVD cannot achieve the guideline-recommended BP and low density lipoprotein cholesterol (LDLc) goals. The European Society of Cardiology European Action on Secondary and Primary Prevention by Intervention to Reduce Events (EUROASPIRE) IV cross-sectional survey reported recently that risk factor control is very poor, with less than half (42.8%) of the patients on BP lowering medications reaching the target of <140/90 mmHg (<140/80 mmHg in people with self-reported diabetes)6 (Fig. 1A). Also, among treated dyslipidemic patients only 32.7% attained the low-density lipoprotein (LDL)-cholesterol target of <2.5 mmol/l (70 mg/dl)6 (Fig. 1B). Poor adherence, need for multiple medications, physician inertia and deficiency of health-care systems are important factors that affect control rates of both hypertension and dyslipidemia.
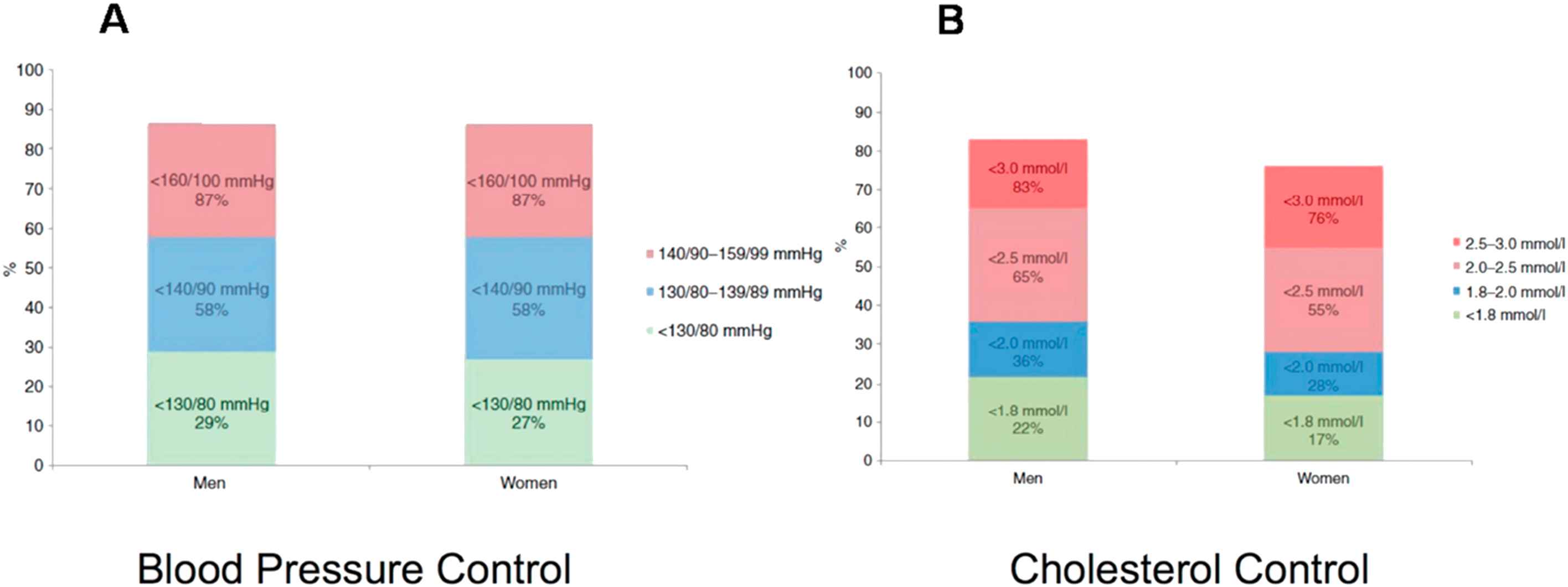
A. Proportions (%) at BP target (<130/80 mmHg, <140/90 mmHg, <160/100 mmHg) in patients on BP lowering medication. B. Proportions (%) at low-density lipoprotein cholesterol target (<1.8 mmol/l, <2.0 mmol/l, <2.5 mmol/l, <3.0 mmol/l) in patients on lipid lowering medication. Modified from: Gyberg V et al. Eur J Prev Cardiol 2015;22(6):753–61.
Therefore, current evidence clearly shows that more efforts must be taken to improve CV prevention in people at high CVD risk. The aim of this review article is to explore efficacy of practical solutions such as the use of fixed-dose combinations of antihypertensive agents and a statin, which might improve the management and prognosis of hypertensive patients with coexisting hypercholesterolemia.
What to combine?
Antihypertensive combination therapy
Dual combination therapy is an important component of guideline-recommended therapy in hypertension because it has numerous benefits. Indeed, adding a drug from another class is 5-fold more effective than doubling the dose of the first drug and BP targets are achieved faster; complications are reduced and adherence is enhanced.7 Overall, better adherence contributes to improved CV protection.
Renin-angiotensin aldosterone system (RAAS) inhibitors are a well-established drug class for the reduction of CVD mortality. Pooled analysis of RAAS inhibitor trials in populations with a high prevalence of hypertension (≥66%) demonstrated a significant reduction in the relative risk (RR) of all cause mortality by 5% and in the RR of all cause mortality by 7% reduction.8 The observed treatment effect resulted entirely from the class of angiotensin converting enzyme (ACE) inhibitors, which were associated with a significant 10% and 12% reduction in all cause mortality and CVD mortality, respectively, whereas no mortality reduction could be demonstrated with angiotensin receptor blocker (ARB) therapy. The largest reductions in the RR of all-cause mortality (by 13%) occurred in three trials in which the ACE inhibitor perindopril (ASCOT-BPLA, ADVANCE and HYVET – 34,242 patients) (Fig. 2).8 Also, ACE inhibitors reduced all-cause mortality, CVD mortality and major CV events in patients with diabetes, whereas ARBs had no benefits on these outcomes.9 In light of these data, ACE inhibitors could be considered as first-line therapy to limit mortality and morbidity in these populations.
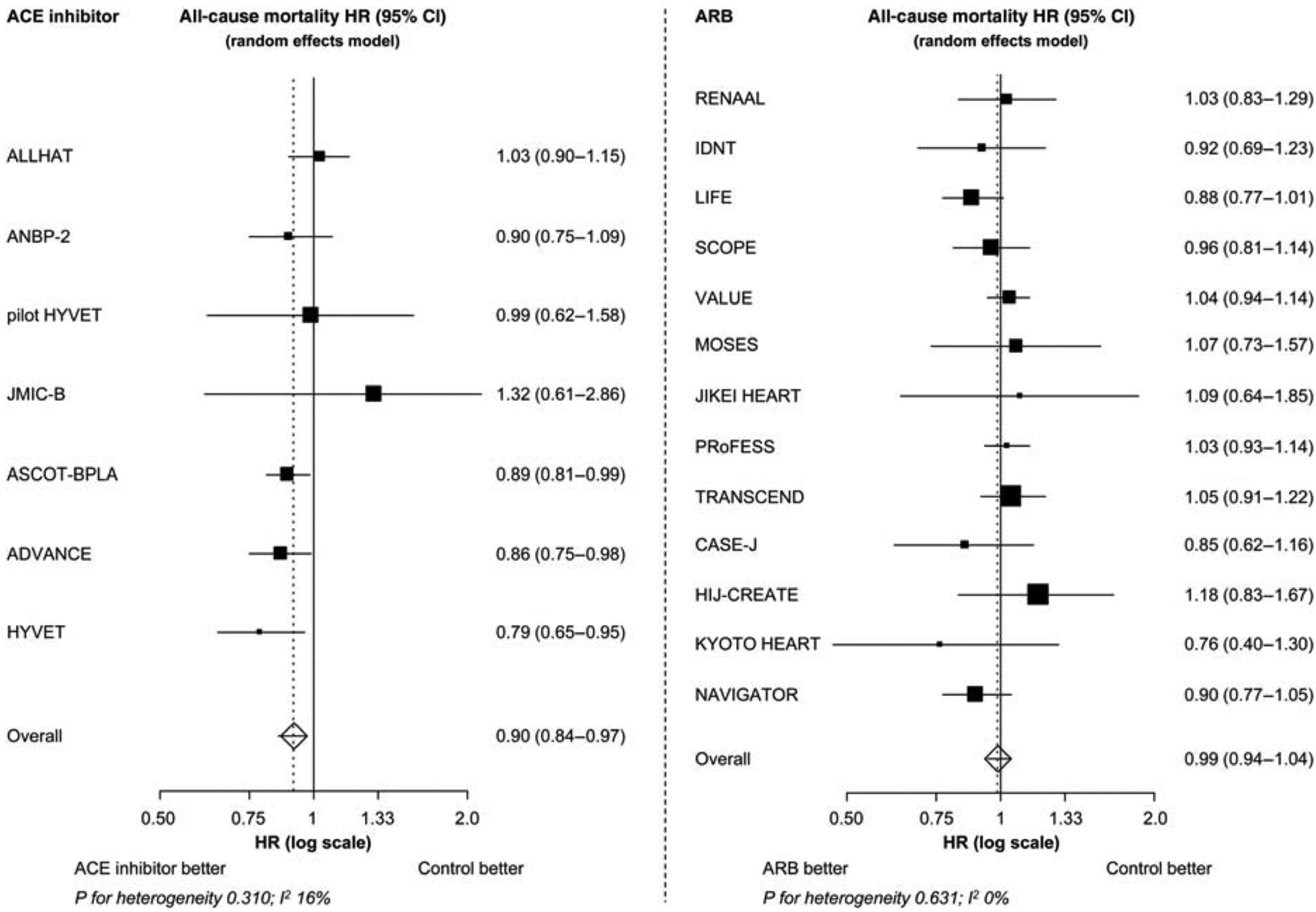
The all-cause mortality treatment effect of ACE inhibitor and ARB trials. HR, hazard ratio; CI, confidence interval; ACE, angiotensin converting enzyme; ARB, angiotensin receptor blocker. P = 0.004 for the treatment effect of ACE inhibitor on all-cause mortality. P = 0.683 for the treatment effect of ARB on all-cause mortality. Modified from: van Vark et al. Eur Heart J 2012;33(16):2088–97.
The combination of a RAAS blocker and a calcium channel blocker (CCB) is very effective in controlling BP. Further, there is convincing evidence that ACE inhibitors and CCBs may be a particularly useful combination in terms of clinical synergy. Protection from coronary artery disease and stroke conferred by ACE inhibitors and CCBs in hypertensive patients that can be explained by the specific drug is of paramount importance. Interestingly, ACE inhibitors appear to preferentially protect from coronary artery disease, while CCBs appear to protect from stroke, over and beyond BP reduction in meta-regression analyses.10 Furthermore, recent data support modern antihypertensive regimen based on an ACE inhibitor and a CCB because this combination therapy improve prognosis by furthering reducing CV endpoints compared with an older antihypertensive treatment regimens based on beta-blocker and diuretic, independent of similar BP control.11,12
Further to hard endpoints, a favorable side-effect profile is very important for patients’ adherence. The addition of ACE inhibition or ARB to CCBs has been shown to reduce peripheral edema, a common adverse effect of therapy with CCBs. According to a meta-analysis, ACE inhibitors seem to be more efficacious than ARBs (by 26% in indirect comparison) in reducing CCB-associated peripheral edema, although head-to head comparisons are desired.13
The combination with statins
It has been clearly demonstrated that cholesterol-lowering therapy with statins reduces morbidity and mortality in patients with coronary artery disease. The post hoc subgroup analysis of the GREek Atorvastatin and Coronary-heart-disease Evaluation (GREACE) study involving high-risk dyslipidemic patients with coronary artery disease demonstrated that statin-ACE inhibitor combination reduces cardiovascular events more than a statin alone (by 34%) and considerably more than an ACE inhibitor alone (by 64%).14 This implies a synergistic effect of these two drug classes regarding secondary prevention in dyslipidemic patients with established coronary artery disease. Furthermore, evidence indicates that triple therapy with a statin, ACE inhibitor, and CCB is associated with a significant reduction in major cardiovascular events. In a post hoc analysis in 1056 patients with stable coronary artery disease participating in the EURopean trial On reduction of cardiac events with Perindopril in stable coronary Artery disease (EUROPA) trial, we showed that the addition of perindopril to CCB and lipid lowering agent was associated with a 46% reduction in the composite of cardiovascular death, myocardial infarction, and resuscitated cardiac arrest15,16 (Fig. 3). The use of the triple combination has been thoroughly explored in an on-treatment sub-analysis of the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) in 1814 patients with at least three CV risk factors and total cholesterol ≤6.5 mmol/l who took atorvastatin, perindopril, and amlodipine at every visit, versus 1978 ASCOT patients who took atorvastatin, atenolol, and bendroflumethiazide at each visit. Patients with other antihypertensive treatments or who stopped taking one of the sub-analysis treatments were excluded, and only events occurring on treatment with the triple therapies were considered in the analysis. The triple therapy of atorvastatin, perindopril, and amlodipine was associated with a significant 42% reduction in relative risk of cardiovascular mortality, nonfatal myocardial infarction, and stroke after a median of 3.3 years compared with patients on atorvastatin, atenolol, and bendroflumethiazide. Similar reductions were observed in the risk of nonfatal myocardial infarction, fatal coronary artery disease and coronary revascularization (39%), stroke (50%), and total cardiovascular events and procedures (24%) systematically in favor of the triple combination of atorvastatin, perindopril, and amlodipine.16,17
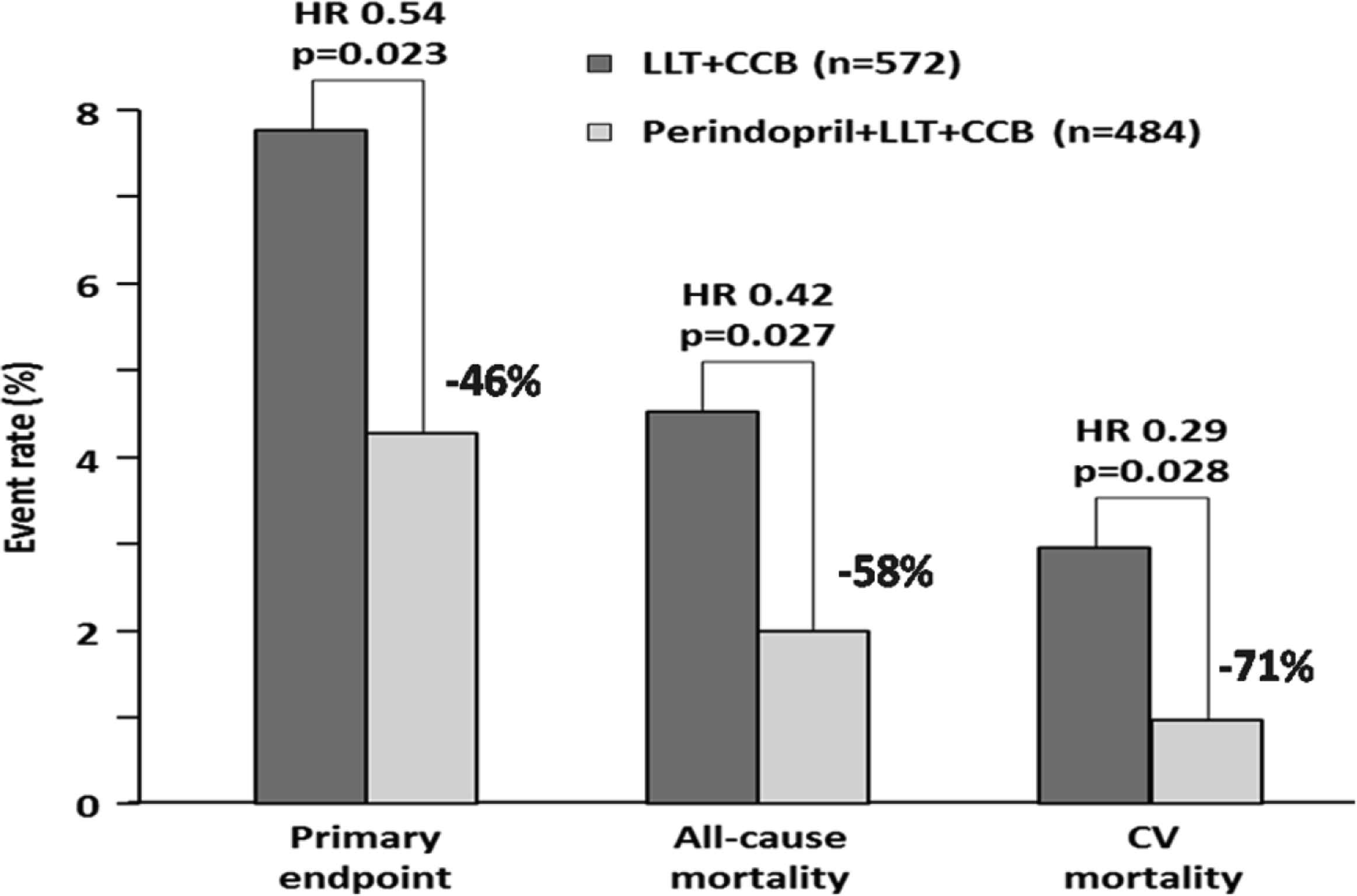
The effect on outcomes of adding perindopril to lipid-lowering therapy (LLT) and calcium channel blockers (CCB) in a subgroup of patients (n = 1056) from EUROPA. Modified from: Bertrand ME et al. Am Heart J 2010;159:795–802.
Possible mechanisms – synergy at the vascular level
The aforementioned sub-analyses of EUROPA andASCOT imply a clinical synergy between perindopril, amlodipine and atorvastatin and prompt for elucidation of potential mechanisms. All three agents have proven anti-atherosclerotic properties. They abrogate endothelial dysfunction, reduce LDL oxidation, prevent proliferation and migration of smooth muscle cells, and they protect from degradation of the fibrous cap of atherosclerotic plaque, all of which contribute to the inhibition of plaque formation and the increased stability of existing atherosclerotic plaque.17–20 Amlodipine has been shown to inhibit the clustering of modified LDL molecules, which prevents foam cells from forming.20 We have shown that atorvastatin protects from endothelial dysfunction induced by acute inflammatory activation.21 Experimental data also suggest a protective effect of ACE inhibitors on endothelial apoptosis with and perindopril exerting greater beneficial effect.22 Furthermore, despite the fact that all antihypertensive agents decrease BP, this is not the case with aortic stiffness and central hemodynamics, which are important predictors of CV risk.23,24 Several studies attest to a superiority of RAAS and CCBs compared with other antihypertensive agents, such as diuretics and non-vasodilating β-blockers, on aortic elastic properties, as well as on central pressures and wave reflections.25–27 The vasodilating effect of ACE inhibitors and CCBs reduces aortic pulse wave velocity thus delaying the return of the reflected wave from the lower body to the heart, while also decreasing its amplitude by dilating conduit muscular arteries.26,27 These modifications of reflected wave characteristics reduce central systolic and pulse pressure. Differences in central and peripheral pressure-lowering effects by vasodilator drugs suggest that their beneficial cardiovascular effects may have been underestimated in studies that measure brachial artery cuff BP with no central aortic pressure determination.25–27 Differential effects on central pressure despite similar effects in brachial pressures evidenced in the Conduit Artery Function Evaluation (CAFÉ) study, a sub-study of the ASCOT, may explain the superiority of the amlodipine ± perindopril arm over the atenolol ± diuretic based arm regarding the clinical benefit documented in the larger study.25 A recent meta-analysis reported that ACE inhibitors reduced pulse wave velocity and augmentation index, which are markers of arterial stiffness and wave reflections.28 Statins also do reduce arterial stiffness in hypercholesterolemic patients and in patients with high CV risk both short- and long-term.27
All in a single pill?
The presence of both hypertension and dyslipidemia places patients at substantially greater risk of CV events than either condition alone. In these patients, adherence with concomitant antihypertensive and lipid-lowering therapy is particularly important. Unfortunately, adherence with concomitant medications antihypertensive drugs and lipid-lowering therapy declines sharply following treatment initiation, with only one out of three patients being adherent to both medications at 6 months.2 Regrettably, non-adherence of protective therapies is associated with higher CV event rates.29 Of interest, occurrence of cardiovascular events may further reduce adherence leading to a vicious cycle with increased risk for further CV outcomes30 (Fig. 4). Clinicians should be aware of the factors likely to be associated with poor adherence, such as time taking therapy, young age, female sex, and the absence of CV events. Identification and attention to these high-risk groups for reduced medication adherence is the first step to reducing CV events.
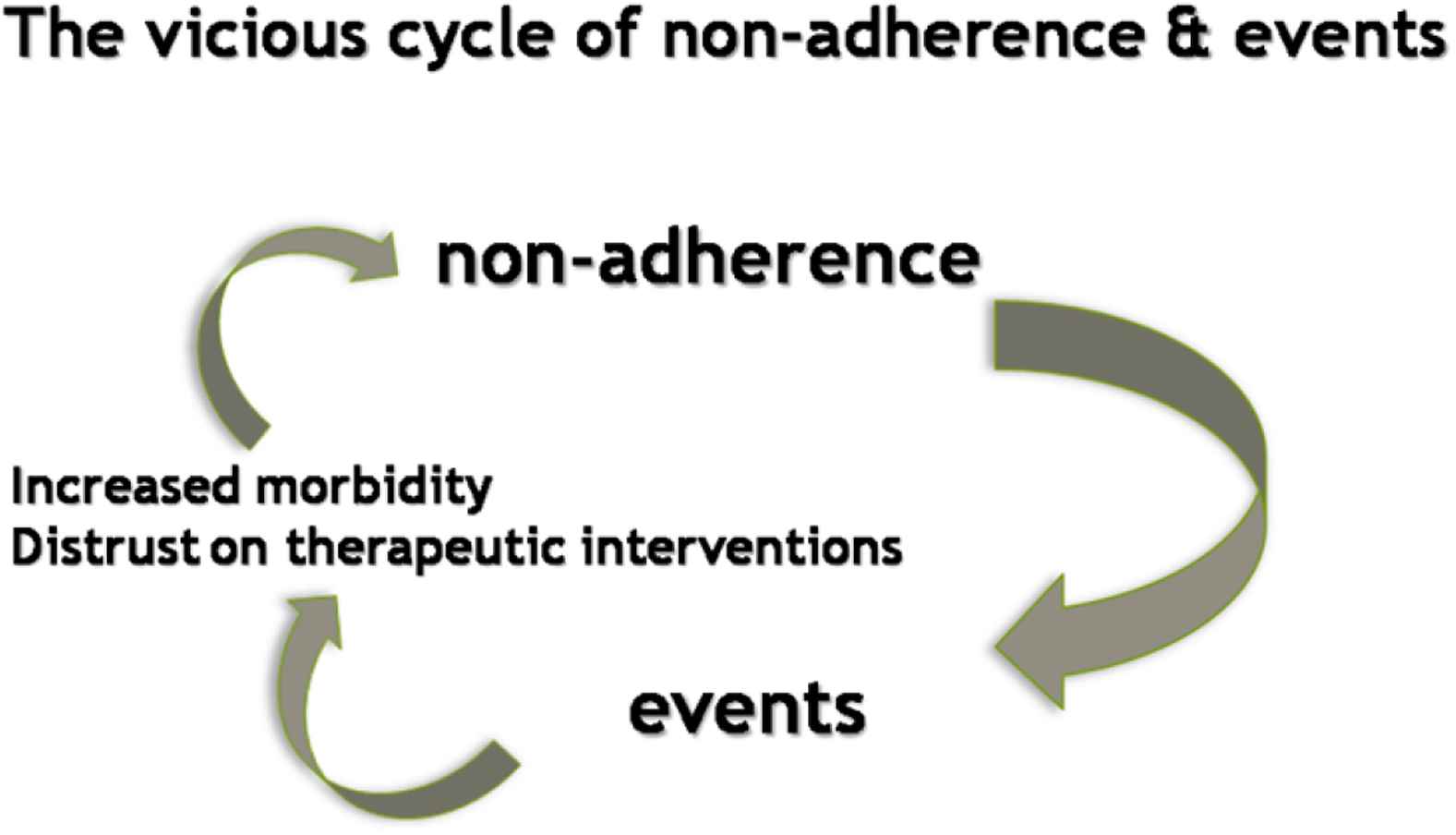
Non-adherence to protective therapies is associated with higher CV event rates. The latter may further reduce adherence, leading to a vicious cycle with increased risk for CV outcomes.
Adherence may be improved significantly by initiating therapies concomitantly and by reducing pill burden. Fixed-dose combination therapies are designed to simplify the medication regimen and potentially improve compliance interrupting the abovementioned vicious cycle. A subgroup meta-analysis of 4 studies on hypertension showed that fixed-dose combination decreased the risk of medication non-compliance by 24% compared with free-drug combination regimen which may translate into better clinical outcomes.31 In adults at high risk of CVD who were recommended for treatment with antiplatelet, statin, and two or more BP lowering drugs, adherence to all four recommended drugs was greater among fixed dose combination than usual care participants at 12 months follow-up (81% versus 46%; relative risk: 1.75).32
The benefits of adherence to cardiovascular medications are clear. In a systematic review and meta-analysis of prospective epidemiological studies, involving adult populations and reporting risk estimates of cardiovascular medication adherence with any good adherence to cardiac therapies could be associated with a 20% lower risk of CVD and a 35% reduced risk of all-cause mortality, irrespective of most clinically relevant patient and study characteristics.33 Accordingly, the recent ESC guidelines for the management of dyslipidemias recommend the use of fixed-dose combination pill for improving adherence.34
Managing hypertension and dyslipidemia at the same time brings enormous benefits for patients. The effect is not just additive but synergistic. It is estimated that 10% reductions in long-term mean blood cholesterol and BP could have reduced major CVD by 45%.35 The primary results of the Heart Outcomes Prevention Evaluation (HOPE)-3 trial clearly show that lowering both cholesterol and BP with a combination therapy is associated with a significantly lower rate of CV events compared to dual placebo among persons at intermediate risk who did not have CVD.36 Therefore, population-wide concurrent reduction of major risk factors is needed if CVD is to be substantially reduced.
Conclusions
In patients with hypertension and hypercholesterolemia combining antihypertensive agents and lipid-lowering therapy, such as ACE inhibitors, CCBs, and statins in a single-pill formulation increases adherence, therapeutic goals are attained faster and adverse CV outcomes decrease. The combination of perindopril, amlodipine and atorvastatin offer a novel and effective approach to the reduction of global CV risk in these patients.
Conflicts of interest
CV has received honoraria from Servier.
References
Cite this article
TY - JOUR AU - Charalambos Vlachopoulos AU - Nikolaos Ioakeimidis PY - 2017 DA - 2017/04/05 TI - Practical solutions for hypertensive patients with dyslipidemia☆ JO - Artery Research SP - 49 EP - 54 VL - 18 IS - C SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2017.03.002 DO - 10.1016/j.artres.2017.03.002 ID - Vlachopoulos2017 ER -
