Aortic Stiffness in HIV Infection with and without Antiretroviral Therapy. A Meta-analysis of Observational Studies
These two authors contributed equally to this work.
- DOI
- 10.2991/artres.k.200314.002How to use a DOI?
- Keywords
- HIV infection; cardiovascular risk; pulse wave velocity; aortic stiffness
- Abstract
Background: The risk of Cardiovascular (CV) events is higher in HIV-infected patients (HIV+) compared to HIV-uninfected persons (HIV−). Large artery stiffness, a well-documented predictor of adverse CV prognosis, may mediate this enhanced risk. It is usually assessed by measuring aortic Pulse Wave Velocity (aPWV). Studies examining arterial stiffness in HIV+ yielded inconsistent results. We performed a meta-analysis with the aim to evaluate the association of HIV infection and its therapy [Antiretroviral Therapy (ART)] with aPWV.
Design and Method: The Standardized Mean Difference (SMD) and corresponding 95% confidence intervals were calculated for aPWV in different comparison groups. Statistical heterogeneity, assessed by Q-test and I2 statistic, was observed in all these comparisons. Therefore, random effects model was implemented.
Results: In a total of 12 studies, naive HIV+ (n = 547) showed increased aPWV compared to HIV− (n = 864): SMD = 0.333 (0.125–0.542), p < 0.002. A total of 22 studies were identified comparing HIV+ treated with ART (n = 3348) to HIV− (n = 2547) showing higher values of aPWV in the former than in latter: SMD = 0.391 (0.225–0.556), p < 0.001. In 10 studies, HIV+ treated with ART (n = 761) exhibited greater aPWV values than those of naive HIV+ (n = 457): SMD = 0.262 (0.006–0.518), p = 0.045.
Conclusion: Our meta-analysis seems to suggest that HIV infection “per se” and ART may impair aortic distensibility. However, interpretation of our results needs caution due to between-study heterogeneity and some potential publication biases.
- Copyright
- © 2020 Association for Research into Arterial Structure and Physiology. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
The introduction of Antiretroviral Therapy (ART) has dramatically changed the life expectancies of people infected with HIV that now approach those of HIV negative persons. However, they have an increased risk of Cardiovascular (CV) diseases, compared to HIV-uninfected subjects. HIV infection itself, duration of infection, chronic low-grade inflammation, immune activation, ART-related metabolic disturbances, drug abuse, smoking, opportunistic infections, and renal damage might contribute to the deterioration of the structure and function of the CV districts [1,2], thus enhancing CV risk. Large artery stiffness may mediate this increased risk.
During the last 15 years, a large amount of evidence has accumulated demonstrating that arterial stiffness is a marker of arterial damage [3–5]. It can be assessed in a number of ways, but Pulse Wave Velocity (PWV) provides a noninvasive method of assessing stiffness along an arterial section that is easy to learn and reproducible [4]. Although PWV can be measured in any arterial segment, PWV of the aorta (aPWV) is considered the ‘gold-standard’ measurement of arterial stiffness. Aortic PWV has the clearest pathophysiological significance as the majority of arterial ‘buffering’ occurs in the aorta. In addition, unlike PWV of other arterial segments, aPWV is independently associated with adverse cardiovascular outcomes in large-scale prospective studies [3–5]. Moreover, improving risk classification, aPWV may enable better identification of high-risk populations [3].
In the vast majority of studies measuring aPWV to date, devices endowed with probes placed on the carotid and femoral arteries were used. However, these require access to the femoral artery at the groin, which takes time and may cause discomfort for the patient. This has promoted the use of newer devices, which derives values of aPWV from oscillometric measurements of the brachial artery waveform [4]. Although these new devices are promising, they do not yet have the robust outcome data of the older ones [3,4]. Several studies examined arterial stiffness in HIV+ with inconsistent results [6–29]. In a previous meta-analysis, studies assessing aortic and peripheral PWV were pooled together [30]. This may be misleading, because aortic and peripheral stiffness have different clinical and prognostic significance [3–5]. Other papers on the same issue were published after this meta-analysis.
We performed a new meta-analysis with the aim to evaluate comprehensively the association of HIV infection and its therapy only with aPWV.
2. MATERIALS AND METHODS
2.1. Publication Search Strategy
A systematic literature search was performed by using the following electronic databases: PubMed, SCOPUS, Web of Science and Google Scholar. An upper date limit of 31 December 2018 was applied with no lower date limitation. The key terms used to identify studies were: “HIV and arterial stiffness”; “HIV”; “PWV”. We also searched the reference lists of articles meeting the inclusion criteria to look for additional pertinent studies.
2.2. Selection Criteria
A systematic review was performed using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [31].
Eligible studies were:
- –
Articles, published in English language in peer-reviewed journals.
- –
Studies with an observational design (case-control study, cross-sectional study, or cross-sectional data derived from prospective cohort study) evaluating the effect of HIV infection, or ART, on aPWV.
Studies clearly reporting the values of aPWV, expressed as mean ± SD.
When only median and interquartile range were reported the method of Wan et al. [32] was used to estimate mean ± SD.
2.3. Data Extraction
Two of the investigators (Giovanni Mulè and Giuseppe Mulè) independently screened titles and abstracts and retrieved all articles that either reviewer regarded as potentially relevant. Disagreement was resolved by consensus or discussion with a third investigator (Antonio Cascio).
2.4. Statistical Analyses
Meta-analysis was performed based on aggregate data from selected studies. We used Standardized Mean Difference (SMD) as measure of effect size. The significance of pooled SMD was determined by the Z-test and a p-value <0.05 was considered statistically significant. We ran only the random effects model due to the presence of heterogeneity between studies and it was quantified by Cochrane Q-test and Higgins’ I2 statistic [33]. Subgroup meta-analysis was performed to analyse possible sources of heterogeneity [33]. Random-effects meta-regression analysis was also conducted to assess whether specific continuous variables (effect modifiers) influence the magnitude of effect across studies [33]. Tau2 and the restricted maximum likelihood methods were used to explain residual heterogeneity not explained by potential effect modifiers [33]. The sensitivity of the meta-analysis was assessed by the leave-one-out analysis. We evaluated potential publication bias by visually examining for possible skewness in funnel plots and statistically with the Begg–Mazumdar’s rank correlation test [34] and Egger’s linear regression test [35]. If a bias was evident, we used the “trim and fill” approach [36] to generate a pooled estimate that accounted for the potential unpublished negative findings.
Further details about the statistical methods are reported in the Supplemental digital content.
3. RESULTS
The original search retrieved 59 articles/abstracts of which 23 satisfied the inclusion criteria [6–29]. The main reason for excluding studies was measurement of arterial stiffness in vascular districts different from aorta (Figure 1). In the 24 selected studies, aPWV was determined by four different devices: the Complior System® (ALAM Medical, France) in 10 studies, the SphygmoCor® system (AtCor, Sydney, Australia) in nine studies, the Millar tonometer (SPT-301, Millar Instruments Inc., Houston, TX, USA) in one study; the Arteriograph® (TensioMed, Budapest, Hungary) in the remaining ones. This latter is a one-site device which provides an estimation of aPWV from oscillometric measurements of the brachial artery waveform, whereas the other devices derive aortic stiffness from the measurement of carotid-femoral PWV.
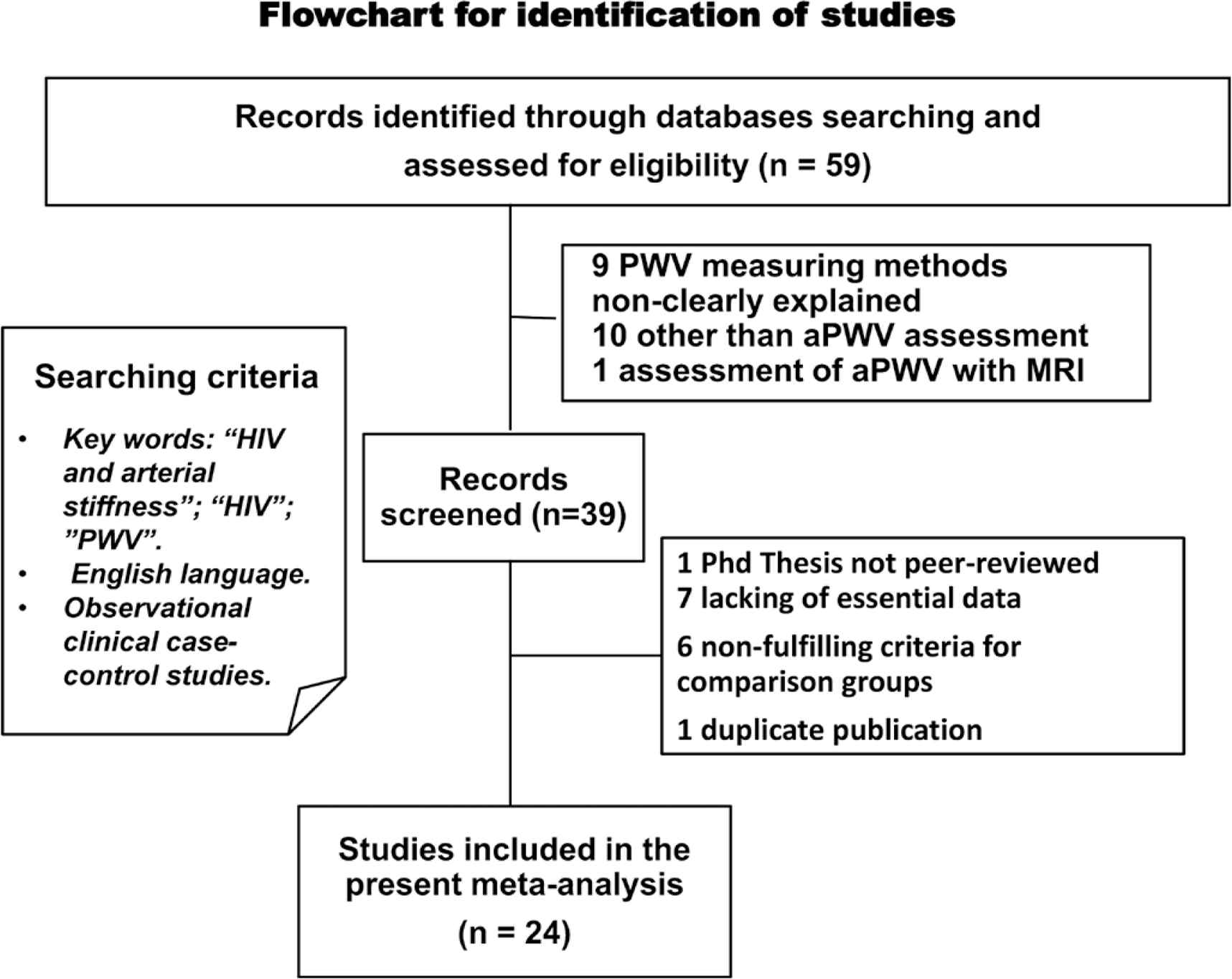
Flow diagram illustrating the process of studies selection.
All studies were observational with cross-sectional design. In three studies, cross-sectional data were derived from prospective cohort investigations. The number of participants in each investigation was relatively small (median value: 55). All the three studies enrolling more than 500 HIV+ patients were published after 2014. The age range was 9–49 years.
3.1. Comparison of HIV Patients Never Treated with Antiviral Drugs with Control Subjects
Of the studies included in the meta-analysis, 12 had sufficient information to allow the comparison of HIV patients never treated with antiviral drugs (naïve) with control subjects without HIV infection (Table 1). HIV positive patients (n = 547) showed higher aPWV than HIV negative subjects (n = 864) with significant between-study heterogeneity (Figure 2A). Subgroup analyses revealed that this difference was significant in studies with the greatest number of participants, in those published after 2012, in studies using SphygmoCor, in youngest age groups and in studies conducted in Africa (Supplemental Digital Content, Table S1). In meta-regression analyses, none of the potential modifiers exhibited significant association with the effect size (Supplemental Digital Content, Table S2). The leave-one-out sensitivity analysis, that iteratively removes one study at a time and recalculates the summary SMD (Supplemental Digital Content, Table S3), suggests the stability of the effect size. No evidence of publication bias was found as indicated by the funnel plot, the Begg–Mazumdar Rank Correlation and the Egger Regression (Figure 2B).
| Author. year | Study design | Country | Site measured | Sample size | Mean age (years) | Males (%) | SBP/DBP (mmHg) | PWV (m/s) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HIV+ naïve | ART+ | HIV− | HIV+ naïve | ART+ | HIV− | HIV+ naïve | ART+ | HIV− | HIV+ naïve | ART+ | HIV− | HIV+ naïve | ART+ | HIV− | ||||
| Awotedu, 2015 | CS | South Africa | Car-Fem | 54 | 52 | 63 | 36.3 | 40.21 | 35.90 | * | * | * | 123/83 | 126/85 | 121/80 | 7.21 | 6.84 | 6.38 |
| Echeverria, 2014 | CS | Spain | Car-Fem | 52 | 19 | 46.50 | 46.43 | 84.10 | 78.80 | * | * | 8.10 | 7.10 | |||||
| Eckard, 2017 | CS | USA | Car-Fem | 101 | 86 | 20.00 | 18.67 | 64.00 | 59.00 | 120/73 | 142/71 | 5.73 | 5.70 | |||||
| Eira, 2012 | CS | Brazil | Car-Fem | 28 | 28 | 30 | 42.0 | 44.11 | 42.39 | 64.3 | 71.43 | 53.33 | 118/* | 125/* | 120/* | 8.80 | 9.72 | 8.58 |
| Guaraldi, 2010 | CS | Tanzania | Car-Fem | 89 | 75 | 93 | 35.9 | 38.40 | 21.60 | 37.1 | 38.67 | 1.08 | 112/74 | 121/77 | 120/77 | 10.60 | 10.10 | 8.30 |
| Kooij, 2016 | CS | Netherland | Ao-PWV | 566 | 507 | 53.50 | 52.60 | 89.40 | 86.00 | 130/84 | 128/782 | 8.03 | 7.83 | |||||
| Kuilder, 2017 | CS | Indonesia | Ao-PWV | 51 | 52 | 8.40 | 8.90 | 51.00 | 44.20 | 108/61 | 111/60 | 6.28 | 6.13 | |||||
| Lekakis, 2009 | CS | Greece | Car-Fem | 22 | 34 | 56 | 40.0 | 40.00 | 40.50 | 100 | 96.00 | 96.43 | 114/70 | 116/77 | 128/84 | 7.50 | 8.40 | 7.85 |
| Lucas, 2013 | CS-PRO | USA | Car-Fem | 192 | 100 | 49.00 | 49.33 | 65.00 | 81.00 | 119/* | 125/* | 8.55 | 8.22 | |||||
| Maia-Leite, 2016 | CS-PRO | France | Car-Fem | 133 | 135 | 47.90 | 47.70 | 91.70 | 91.10 | 132/79 | 126/77 | 7.50 | 7.53 | |||||
| Maloberti, 2013 | CS | Italy | Car-Fem | 36 | 72 | 224 | 40.7 | 46.50 | 44.90 | 80.6 | 83.40 | 74.20 | 126/76 | 126/74 | 124/76 | 9.90 | 10.80 | 9.30 |
| Monteiro, 2012 | CS | Brazil | Car-Fem | 28 | 233 | 82 | * | 42.00 | 42.00 | * | 33.00 | 32.90 | 122/77 | 124/80 | 7.26 | 7.92 | 7.75 | |
| Moreira, 2018 | CS | Brazil | Car-Fem | 644 | 105 | 43.47 | 44.29 | 57.92 | 35.24 | 125/76 | 129/78 | 8.51 | 8.93 | |||||
| Msoka, 2016 | CS | Tanzania | Car-Fem | 51 | 55 | 40 | 45.0 | 45.00 | 45.00 | 23.4 | 17.65 | 62.50 | 127/77 | 123/76 | 125/75 | 7.30 | 8.20 | 7.00 |
| Ngatchou, 2013 | CS | Cameroon | Car-Fem | 108 | 130 | 96 | 39.0 | 41.00 | 41.00 | 26.7 | 26.00 | 28.00 | 117/77 | 118/81 | 128/83 | 7.50 | 7.20 | 6.90 |
| Okello, 2017 | CS | Uganda | Ao-PWV | 577 | 538 | 45.33 | 46.33 | 43.00 | 44.00 | 123/76 | 127/8 | 7.80 | 8.00 | |||||
| Papita, 2012 | CS | Romania | Ao-PWV | 43 | 25 | 37.80 | 37.80 | 60.50 | 60.00 | 122/73 | 119/74 | 5.59 | 4.43 | |||||
| Rose, 2013 | CS-PRO | Australia | Car-Fem | 19 | 27 | 15 | 40.6 | 39.83 | * | * | * | 60.00 | 122/73 | 117/73 | * | 7.30 | 7.50 | 6.30 |
| Schillaci, 2005 | CS | Italy | Car-Fem | 32 | 32 | 41.00 | 41.00 | 78.00 | 78.00 | 128/80 | 126/82 | 7.60 | 6.80 | |||||
| Schillaci, 2008 | CS | Italy | Car-Fem | 39 | 23 | 23 | 37.0 | 40.00 | 39.00 | 67.0 | 83.00 | 83.00 | 120/78 | 120/77 | 122/80 | 7.50 | 7.70 | 6.40 |
| van Vonderen, 2009 | CS | Netherland | Car-Fem | 22 | 55 | 52 | 38.0 | * | 50.47 | * | * | * | * | * | * | 7.00 | 7.00 | 6.70 |
| Vlachopoulos, 2009 | CS | Greece | Car-Fem | 51 | 35 | 33.1 | 33.2 | 92.0 | 88.5 | 126/73 | 127/77 | 6.40 | 6.30 | |||||
| Yannoutsos, 2014 | CS | France | Car-Fem | 173 | 174 | 49.00 | * | 80.00 | * | 126/81 | * | 8.43 | 8.17 | |||||
Not reported.
CS, cross-sectional study; CS-PRO, cross-sectional data derived from prospective cohort study; Car-Fem, carotid artery to femoral artery; SBP, systolic blood pressure; DBP, diastolic blood pressure; PWV, pulse wave velocity.
Characteristics of the included studies comparing HIV patients never treated with antiviral drugs (HIV+ naïve), HIV patients treated with antiviral drugs (ART+) and HIV negative (HIV−) subjects
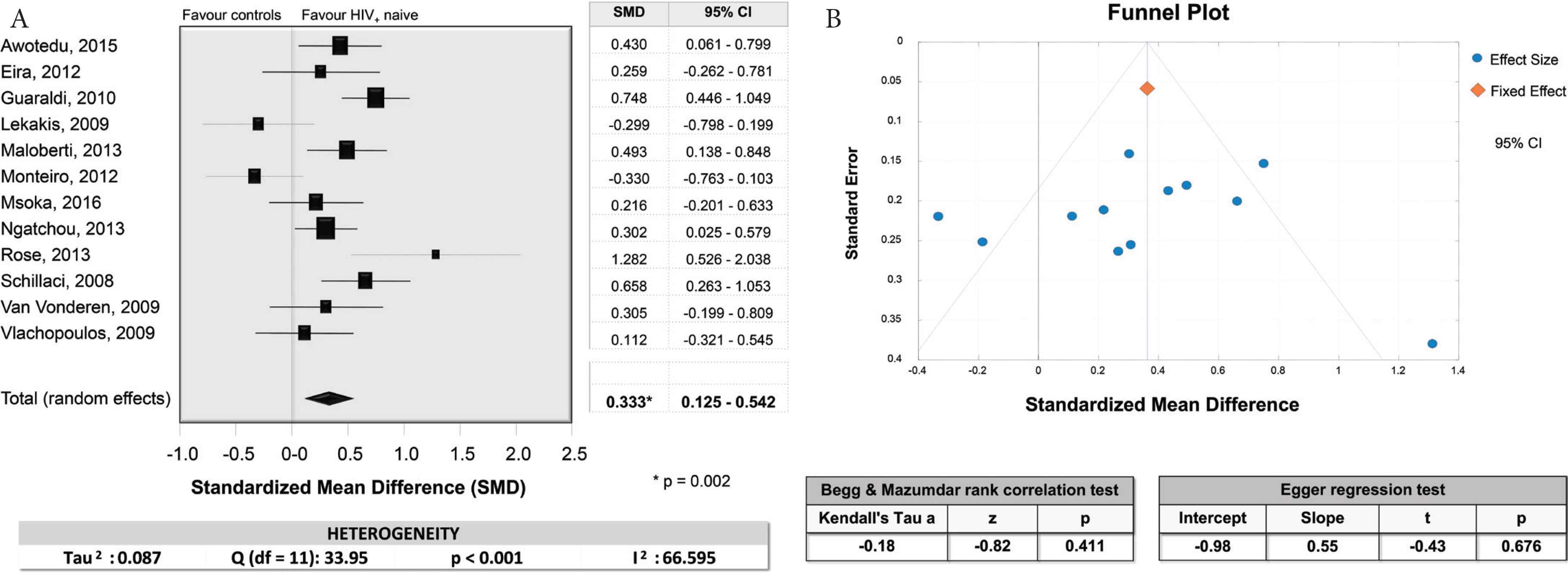
(A) Forest plot for the aortic PWV comparison of HIV patients never treated with antiviral drugs (naïve) with control subjects. At the bottom of the figure, on the left, are also reported the results of the Q-test and of the I2 statistic indicating a moderate between-study heterogeneity. (B) Funnel plot and results of the Begg–Mazumdar rank correlation and the Egger regression tests indicating the likely absence of publication bias.
3.2. Comparison of HIV Patients Treated with Antiviral Drugs with Control Subjects
The comparison of HIV+ on ART (n = 3348) with HIV− subjects (n = 2547) (Figure 3A), performed in 22 studies (Table 1) disclosed greater values of aPWV in ART+ than in HIV− (p < 0.001), with highly significant between-study heterogeneity. In subgroup analyses this difference remained statistically significant in studies with lower number of participants (<64), in those published before 2012, in studies with a lower proportion of males, in those with systolic BP below 122 mmHg, in studies using SphygmoCor and Complior, in those performed in Europe. The effect size was higher in subjects aged below the median age of 42.6 years (0.452) than in the older ones (0.325), but in both subgroups it was statistically significant (Supplemental Digital Content, Table S4).
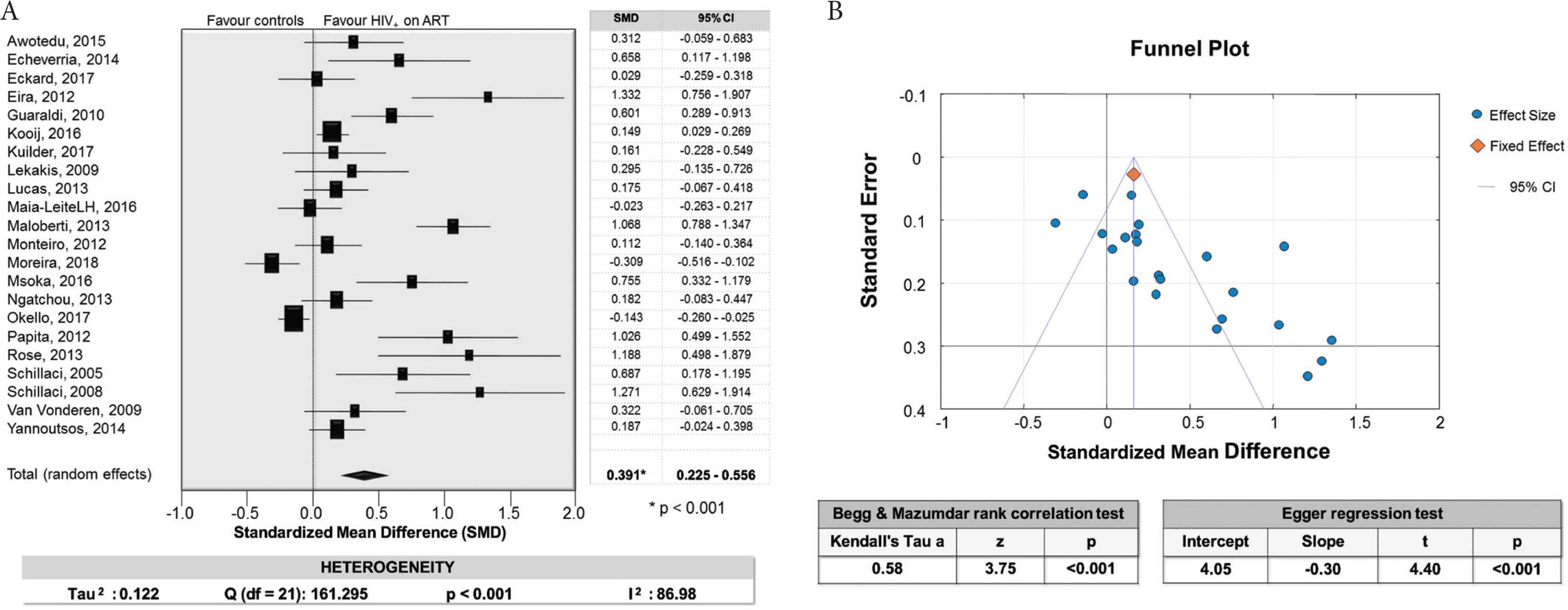
(A) Forest plot for the aortic PWV comparison of HIV patients treated with antiviral drugs with control subjects. At the bottom of the figure, on the left, are also reported the results of the Q-test and of the I2 statistic indicating a high between-study heterogeneity. (B) Funnel plot and results of the Begg–Mazumdar rank correlation and the Egger regression tests indicating the presence of publication bias.
In meta-regression analyses (Supplemental Digital Content, Table S5), aPWV SMD was inversely related to the year of publication (Figure 4), the number of participants and the proportion of diabetic patients. The proportion of hypertensive patients and the prevalence of smokers showed respectively negative and positive relationships with aPWV SMD of borderline statistical significance (p = 0.054 the former and p = 0.058 the latter). In leave-one-out sensitivity analysis, no substantial difference was observed in aPWV SMD (ranging from 0.351 to 0.426), when individual studies were removed one at a time (Supplemental Digital content, Table S6). The analysis of the funnel plot, the Begg–Mazumdar Rank Correlation and the Egger regression revealed a publication bias (Figure 3B). The trim-and-fill approach showed that nine potentially missing studies would be needed to obtain funnel plot symmetry. By using this method, the adjusted pooled SMD changed substantially after correction for potential unpublished negative findings [0.04 (−0.01 to 0.09)], shifting to non-significance. This suggests that the influence of this bias was likely important.
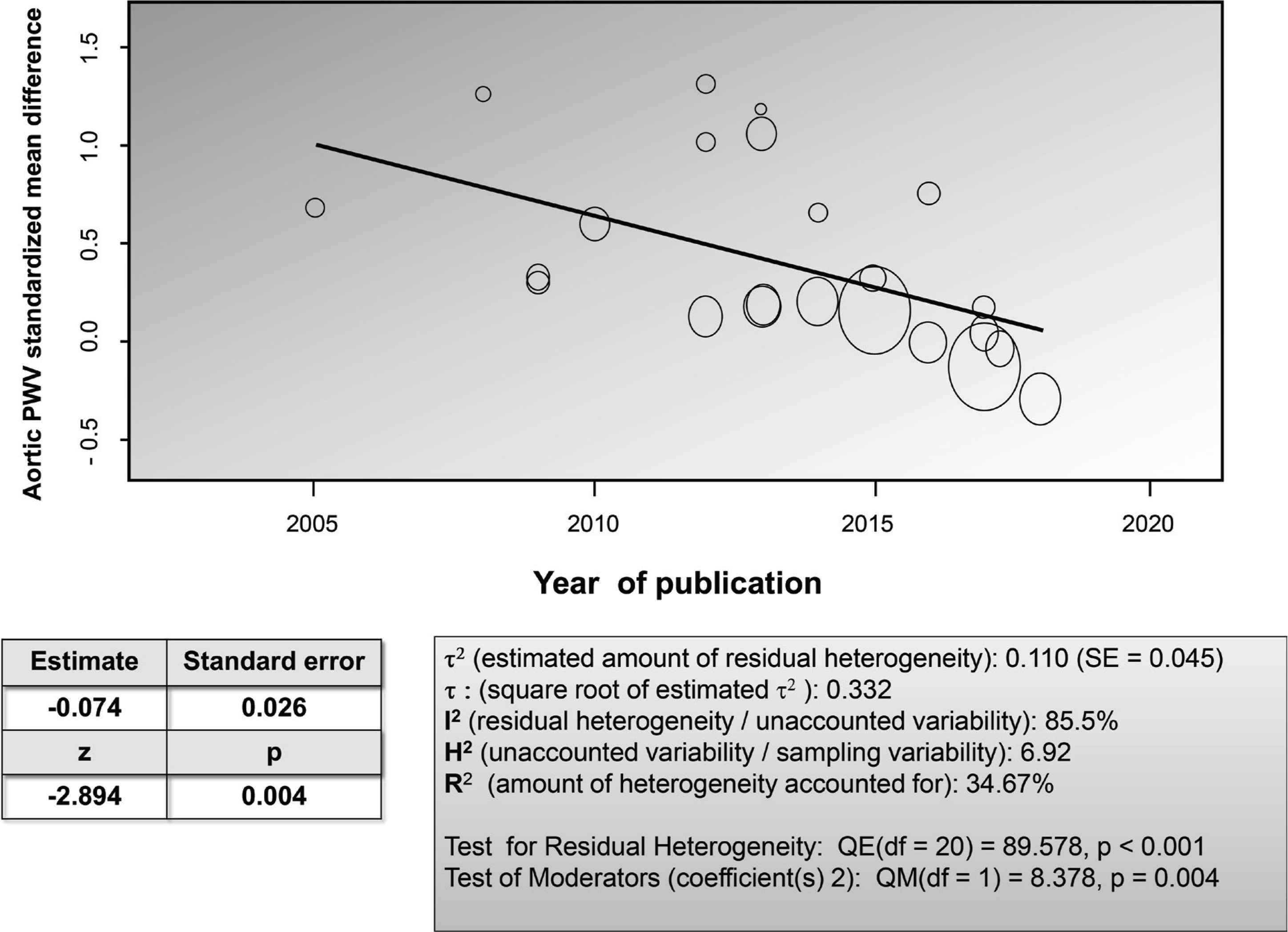
Meta-regression relating-year of studies publication and aortic PWV standardized mean difference between HIV+ patients treated with antiviral drugs and control subjects.
3.3. Comparison of HIV Patients Treated with Antiviral Drugs with HIV+ Naïve Patients
HIV patients treated with antiviral drugs (ART+) (n = 761) showed slightly increased aPWV when compared to naïve patients (n = 457) (Table 1). This difference was barely significant, p = 0.045 (Figure 5A). Heterogeneity between studies was highly significant. Subgroup analyses showed that this difference was significant only in the studies with a lower proportion of males and in those conducted in Europe and in South America (Supplemental Digital Content, Table S7). The effect size was of borderline statistical significant in studies with lower number of participants, with subjects older than 40 years, in those published before 2012 and with higher systolic BP (Supplemental Digital Content, Table S7).
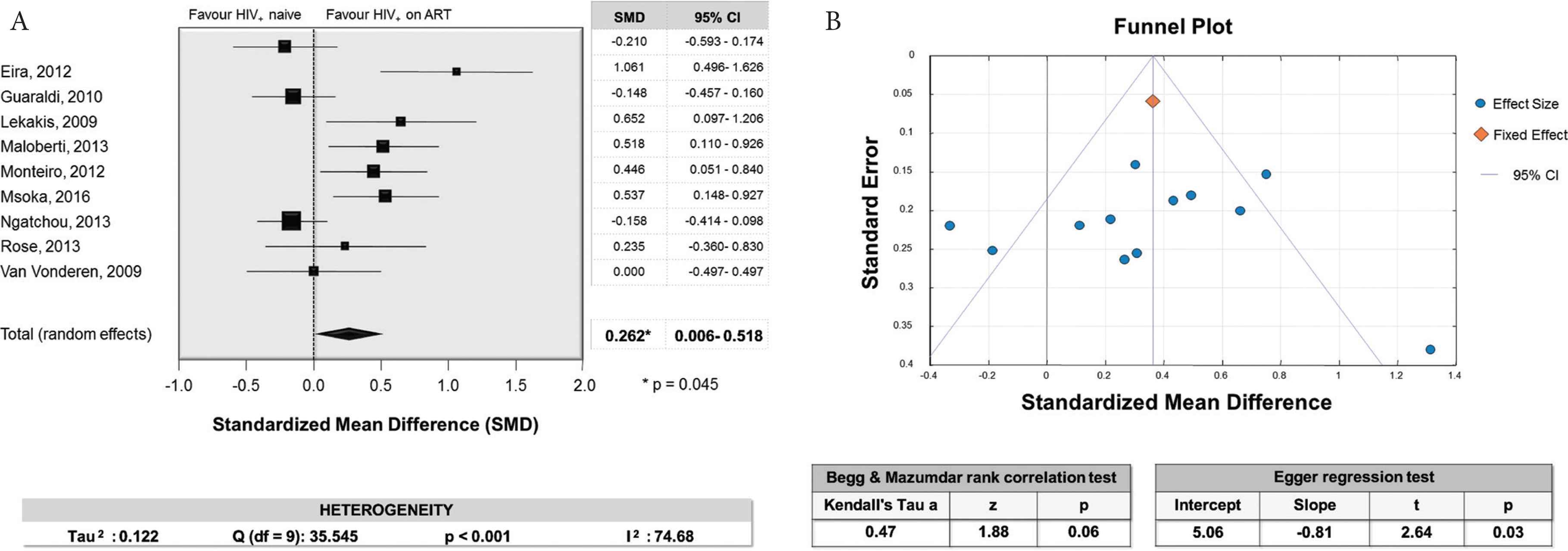
(A) Forest plot for the aortic PWV comparison of HIV patients treated with antiviral drugs with HIV+ naïve patients. At the bottom of the figure, on the left, are also reported the results of the Q-test and of the I2 statistic indicating a high between-study heterogeneity. (B) Funnel plot and results of the Begg–Mazumdar rank correlation and the Egger regression tests indicating the likely absence of publication bias.
In meta-regression analysis age was directly associated with the magnitude of the aPWV SMD (Supplemental Digital Content, Table S8).
The leave-one-out sensitivity analysis disclosed some difference in results (Supplemental Digital Content, Table S9), with SMD ranging from 0.182 (p = 0.127), after removing the study of Eira [24], to 0.41 (p < 0.001) excluding the study of Kooij [16]. However, after the exclusion of these or other individual studies included in the meta-analysis, the point estimate of the combined effect size remained inside the confidence interval of the overall estimate with all available studies. Therefore, no specific study may be considered to have an excessive influence on results.
The analysis of the funnel plot, the Begg–Mazumdar Rank Correlation and the Egger regression did not show evidence of publication bias (Figure 5B).
4. DISCUSSION
The main findings of this meta-analysis can be summarized as follows:
- 1)
HIV+ patients never treated with antiviral drugs showed higher values of aPWV than control subjects without HIV infection (Figure 2A).
- 2)
HIV+ patients treated with antiviral drugs exhibited greater values of aPWV than HIV negative subjects (Figure 3A).
- 3)
HIV+ patients treated with antiviral drugs showed increased aPWV when compared to HIV+ subjects naïve to antiviral therapy, although this difference was of marginal statistical significance (Figure 5A).
Though there was a moderate-to-high between-study heterogeneity in all these comparisons, sensitivity analyses showed that none of the selected studies had a significant influential effect on the overall estimates.
Subgroup analyses and meta-regression analyses revealed that some variables may influence the magnitude of effect across studies, explaining only a small fraction of the heterogeneity. The impact of these variables is different in relation to the comparisons evaluated. When HIV+ naive patients were compared to control subjects, the factors positively associated with a greatest effect size were the number of participants, the year of publication after 2012, the use of SphygmoCor, the youngest age groups. Moreover, the aPWV difference was greater in studies performed in Africa than in other geographic areas.
In the comparison of HIV+ treated with ART with HIV− an increased aPWV difference was associated with studies having a smaller sample size or published before 2012, studies with a lower proportion of males, those with systolic BP below 122 mmHg, studies using SphygmoCor and Complior, or performed in Europe. In meta-regression analyses there was an inverse relationship between aPWV SMD and year of publication, number of participants, proportion of diabetic patients. Moreover, the difference in triglycerides and the differences in smokers and diabetic subjects proportions were directly associated to the magnitude of the effect size.
The first result of our meta-analysis seems to support the notion that HIV infection “per se” may increase large arteries stiffness. One of the mechanisms by which HIV impairs aortic elasticity may be chronic immune activation and systemic inflammation [1,2]. The HIV-induced up-regulation of some proinflammatory cytokines might trigger endothelial dysfunction leading to changes in the extracellular matrix (arterial smooth muscle cell proliferation, increased synthesis of collagen, and loss of elastin) and ultimately to stiffening of the arteries [1].
It is interesting to note that using fluorodeoxyglucose–positron emission tomography and coronary computed tomographic imaging, Subramanian et al. [37] found that compared with HIV-uninfected control groups without atherosclerotic disease, HIV infected participants demonstrated increased arterial inflammation of the aorta.
The second result of our meta-analysis, that is aPWV higher in HIV+ on ART than in control subjects, is in line with a previous meta-analysis on the same issue and with several studies showing that highly active antiretroviral therapy may have pro-atherogenic properties, caused by a derangement of lipid and glucose metabolism [30].
Paradoxically, although long-term exposure to antiretroviral therapy is associated with an increased risk of CV events, interruption of ART has also been associated with enhanced CV risk [38].
The protease inhibitor class of antiretroviral drugs is most widely associated with atherosclerosis and increased PWV [8,12]. However, in our meta-regression analysis no relationship was observed between the effect size and the proportion of protease inhibitors (PI) used in 15 of the 22 studies included (Supplemental Digital Content, Table S5). On the other hand, in a recent prospective study, age, BP, nadir CD4+ count < 200/mm3, but not ART, were related to a worsening of aortic stiffness after 7 years of follow-up [14]. This finding, as well as other cross-sectional reports, suggest that the impact on vascular health of HIV infection severity or dysimmunity may be more important than the metabolic derangements related to ART. On the other hand, it is very likely that untreated HIV patients are newly infected subjects. Therefore, the difference regarding aPWV between treated and untreated HIV individuals may be due to the longer duration of HIV infection in the former than in the latter, rather than to the direct unfavourable effects of ART on aortic stiffness.
In meta-regression analysis an inverse association was found between the aPWV SMD and the publication year. In other words, in most recent studies ART seem to have neutral or favourable influence on arterial elasticity. This finding may be probably due to an earlier initiation of ART in the studies published more recently.
Another explanation may be a more extensive use in last years of cardiovascular prevention therapies, such as antihypertensive drugs or statins, in the HIV population. It is important to note that the analysis of the funnel plot, the Begg–Mazumdar Rank Correlation and the Egger regression revealed a publication bias (Figure 3B), that is likely to be important since, the trim-and-fill procedure provided an adjusted pooled SMD markedly different from the unadjusted effect size and no more statistically significant.
4.1. Strengths and Limitations
One strength of our study was the inclusion of reports exploring only aPWV. This is at variance with a previous meta-analysis on a similar issue [30] in which were included also studies investigating stiffness of peripheral arterial districts, that are not endowed with prognostic significance like impaired aortic elasticity. Furthermore, more metaregression and subgroup analyses were performed in our study as compared to the previous one [30].
Our study shares other limitations inherent with meta-analyses. Since individual patient data were unavailable, we used aggregate data as reported in published articles. This commonly used approach cannot solve methodological problems affecting the primary studies. Our data sources were observational cross-sectional studies, thus restricting our ability to detect causality relations and to explore fully the influence of unmeasured confounding variables.
Not all information regarding potentially relevant variables was available or it was available only in a small fraction of the selected studies thereby reducing the power of the statistical tests.
The heterogeneity between studies was not fully explained by the subgroup analysis and meta-regression.
With these limitations in mind, our findings suggest that HIV infection per se and ART may impair aortic distensibility. These results may help to explain the enhanced CV risk of HIV+ patients.
Additional prospective investigations with long-term follow-up are warranted to further explore the impact of HIV infection and its therapy on aortic stiffness. Moreover, further studies should investigate the influence of new antiretroviral drugs, particularly integrase inhibitors, on the elastic properties of large arteries.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
Giovanni Mulè and Giuseppe Mulè contributed to the conception and design of the work. All authors (Giovanni Mulè, Giuseppe Mulè; VT, PC; G. Mazzola, MT; CC; AC) contributed to the acquisition, analysis, and interpretation of data for the work, drafted the manuscript and critically they revised it. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
SUPPLEMENTARY MATERIALS
Supplementary data related to this article can be found at
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Giovanni Mulè AU - Giuseppe Mulè AU - Valeria Tranchida AU - Pietro Colletti AU - Giovanni Mazzola AU - Marcello Trizzino AU - Claudia Colomba AU - Antonio Cascio PY - 2020 DA - 2020/03/19 TI - Aortic Stiffness in HIV Infection with and without Antiretroviral Therapy. A Meta-analysis of Observational Studies JO - Artery Research SP - 13 EP - 20 VL - 26 IS - 1 SN - 1876-4401 UR - https://doi.org/10.2991/artres.k.200314.002 DO - 10.2991/artres.k.200314.002 ID - Mulè2020 ER -
