Factors Associated with Cardio Ankle Vascular Index (CAVI) and its Mathematically Corrected Formula (CAVI0) in Community Dwelling Individuals
 , Azadeh Alizargar4, Chyi-Huey Bai5, Javad Alizargar6, *,
, Azadeh Alizargar4, Chyi-Huey Bai5, Javad Alizargar6, *, 
- DOI
- 10.2991/artres.k.201124.002How to use a DOI?
- Keywords
- Atherosclerosis; cardiovascular diseases; cardio ankle vascular index; ankle brachial index; hypertension; atherosclerosis; risk factor
- Abstract
Cardio Ankle Vascular Index (CAVI) and mathematically corrected formula derived from it (CAVI0) are indices for arterial stiffness and atherosclerosis. Role of different atherosclerotic risk factors on CAVI and CAVI0 is not clear in the community dwelling individuals. This study aims to evaluate the association of different Cardiovascular Disease (CVD) risk factors on CAVI and CAVI0. Participants from a prospective cohort study have been recruited for CAVI measurement. Known risk factors for atherosclerosis were assessed in the individuals. CAVI and CAVI0 is highly correlated (Pearson’s r = 0.95 and p < 0.001). Further correlation analysis of the study variables with CAVI shows that CAVI is significantly correlated with age, Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Mean Blood Pressure (MBP). CAVI0 is also significantly correlated with age, SBP and MBP. CAVI0 is not correlated with DBP (Pearson’s r = 0.05 and p = 0.46). Among laboratory tests, CAVI and CAVI0 are correlated with Blood Urea Nitrogen (BUN) (r = 0.20, p = 0.009 and r = 0.22, p = 0.004 respectively) and also with HBA1c (r = 0.21, p = 0.006 and r = 0.25, p = 0.001 respectively). Multivariate analysis showed that only age is independent determinant of CAVI and CAVI0. As SBP and DBP are not independently associated with CAVI and CAVI0, these indices could be considered reliable in differentiating people with high risks of CVD, as it is not dependent on other risk factors. As CAVI0 is not correlated with DBP, when evaluating the results of CAVI0, we should consider that this index maybe not be reflective of DBP in the patient.
- Copyright
- © 2020 Association for Research into Arterial Structure and Physiology. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Cardiovascular Disease (CVD) like Coronary Heart Disease (CHD) are leading cause of death in the world [1]. Screening to find subclinical damages due to CVD has been suggested by European Society of Hypertension and cardiology guidelines, because classical risk factors fail to predict it [2]. Arterial stiffness is one of these suggested parameters for screening subclinical organ damage [3]. Arterial stiffness can be calculated by different indexes. One of the most known indexes is carotid-femoral Pulse Wave Velocity (cfPWV), and that is the velocity of the arterial pulse moving along the vessel wall [4]. Although this method is the most frequently used method in evaluating arterial stiffness, it is dependent on current Blood Pressure (BP) and short term changes in BP [5]. A novel index has been introduced named Cardio Ankle Vascular Index (CAVI), solving this issue as it is not dependent on the current BP [6,7]. Although it is said that blood pressure has no independent effect on CAVI values, some studies report contradicting results [8]. Aside from blood pressure, other factors such as age, body compositions, history of CVD and Ischemic Heart Disease (IHD), Type 2 Diabetes Mellitus (T2DM), smoking, alcohol drinking, exercise and anxiety have been evaluated in this study. These factors have been suggested to be associated with arterial stiffness and atherosclerosis [9–12]. Lipid profile and fasting blood sugar also have been shown to influence CAVI and yet have not been agreed upon [13]. Some laboratory tests like high sensitivity C-reactive protein (hs-CRP), Blood Urea Nitrogen (BUN), Creatinine (Cr), serum Uric Acid (UA) and Fasting Blood Sugar (FBS) can also have some effects on CAVI measurement [14]. The question of independent association of these factors with CAVI has not been addressed in details so far.
A mathematically corrected formula derived from CAVI was proposed by Spronck et al. [15,16] they also provided a tool to easily convert CAVI into CAVI0 values. They claimed that CAVI0 is less dependent on blood pressure changes. Studies to compare CAVI and CAVI0 at the same time to observe the difference between associating factors can shed light on this matter.
This study primarily tries to answer the question of which one of the atherosclerosis and arterial stiffness risk factors has the most independent effect on CAVI and CAVI0 measurement. Our secondary objective is to try to find out the factors that should be considered if we are dealing with using CAVI and CAVI0 in clinical practice. We also try to understand what happens if we use CAVI0 as our primary measure instead of CAVI. Sex differences in association of serum levels of study variables with CAVI is also considered in this study. A study on community dwelling individuals without high risk of CVD may help us better understand the independent role of mentioned risk factors and if we find an appropriate model, distinguish between the people who may benefit the measurement of CAVI and CAVI0 in clinical practice.
2. MATERIALS AND METHODS
Participants were recruited as a part of annual checks of a community-based prospective cohort study on the community dwelling individuals of six villages in Shihlin District, and six villages in Wenshan District, Taipei, Taiwan (the coverage of Shin Kong Wu Ho-Su Memorial Hospital and Wan Fang Hospital respectively) that was designed to evaluate the CV and cerebrovascular risk factors in individuals. They were excluded if age ≤30, had an incomplete questionnaire, prior history of cancer, chronic kidney disease, refused to blood draw or perform CAVI measurement. Data of 198 individuals were collected. All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Taipei Medical University with the Institute Review Board (reference numbers 94E-183, 94E-198 and 96E-004). We excluded one individual that had prior history of admission due to stroke and nine that had admission due to CVD. Twenty two individuals that had positive hepatitis B infection and seven that had hepatitis C infection were also excluded. To exclude the people with high risk of atherosclerosis, we removed two cases with Ankle Brachial Index (ABI) >1.3. Final data of 163 individuals were analyzed.
All subjects’ demographic data were gathered on age, sex, body height and weight, history of IHD, T2DM, Family History of heart disease (FH) and Hypertension (HTN). IHD and T2DM was based on the physician diagnosis. FH is positive if there is a history of heart disease in brother or father <60 years old and in sister or mother before 65 years of age. Smoking history was also gathered, whether they ever smoked or not, and if so the number of cigarettes per day and the duration of smoking. Pack-years of smoking was calculated by multiplying the packs of cigarettes per day by years of smoking.
Habit of alcohol drinking and the volume (cc) of alcohol drinks per week was asked. Participants were asked whether they have the habit of exercising and the frequency of exercising per week was also questioned. Fasting blood was taken and sent to the laboratory for determination of serum levels of BUN, Cr, AST, ALT, FBS, UA, hs-CRP, High Density Lipoprotein (HDL), Low Density Lipoprotein (LDL) and Triglyceride (TGL) using standard methods (using an X-1500-Sysmex, Germany; Beckman AU5800, USA; and Tosoh HLC-723G8 automated glycol-hemoglobin analyzer, Japan). Evaluation of anxiety was carried out using the standard General Anxiety Disorder 7 questionnaire (GAD-7). Every question scores [range 0 (not at all) to 3 (Nearly every day)]. Overall score of 5, 10 and 15 were used to categorize mild, moderate and severe cases of anxiety.
Participants were asked to lie down in supine position for 10 min and electrocardiogram (ECG) and phonocardiogram (PCG) were performed on them. Pulse wave velocity (PWV) was measured by VaSera VS-1000 (Fukuda Denshi, Tokyo, Japan) [17]. All the CAVI measurement was done intrinsically by VS-1000. CAVI is measured by the following formula:
CAVI0 is calculated by the conversion tool that Spronck et al. [16] suggested from CAVI. The CAVI0 has been obtained from the following formula:
SBP and DBP are systolic and diastolic blood pressure. ΔP = SBP − DBP and ρ is the blood density. a and b are the constants automatically measured by the device to match aortic PWV. P0 is the reference pressure (100 mmHg).
All study variables were analyzed by ANOVA and Fisher’s exact test stratified by CAVI levels. CAVI was analyzed for normal distribution test (Shapiro–Wilk test) before performing a multiple regression analysis. Pearson’s correlation analysis performed on the study variables and 95% prediction eclipse of this study variables was drawn based on the study objectives to show the relationship between the variables. Linear regression model was used to evaluate the independency of associations of selected correlated factors with CAVI and CAVI0. CAVI and CAVI0 were served as the dependent variable in the linear regression model. All of the parameters with significant correlation with CAVI and CAVI0 was selected to be put in the models and different models were selected base on the objectives of the study. Logistic regression models were used to determine high CAVI and CAVI0. Odds ratio and Confidence Interval (CI) was calculated afterwards. All statistical analysis was performed using SAS 9.4. (SAS, Cary, NC, USA).
3. RESULTS
Data of 163 community individuals were analyzed. The mean age ± Standard Deviation (SD) was 63.06 ± 9.40. Sixty five (39.98%) were male. Table 1 summarized the study parameters stratified by CAVI level. It also contains the Pearson correlation coefficient (r) and p-value of different variables with CAVI measures. Study parameters stratified by CAVI level (using median and 75 percentile of CAVI as the cut point) can be found in Supplementary Materials (Tables 1–4).
CAVI and CAVI0 is highly correlated (Pearson’s r = 0.95 and p < 0.001). Further correlation analysis of the study variables with CAVI shows that CAVI is significantly correlated with age, SBP, DBP, MBP. CAVI0 is also significantly correlated with age, SBP and MBP. CAVI0 is not correlated with DBP (Pearson’s r = 0.05 and p = 0.46). Among laboratory tests, CAVI and CAVI0 are correlated with BUN (r = 0.20, p = 0.009 and r = 0.22, p = 0.004 respectively) and also with HBA1c (r = 0.21, p = 0.006 and r = 0.25, p = 0.001 respectively). CAVI and CAVI0 are not significantly correlated with other study variables (Table 1).
| Variables | Mean ± SD | Sex | p | Pearson correlation with CAVI | Pearson correlation with CAVI0 | |||
|---|---|---|---|---|---|---|---|---|
| Number (%) | Male | Female | r | p | r | p | ||
| CAVI | 8.64 ± 1.08 | 8.69 ± 1.15 | 8.60 ± 1.04 | 0.614 | 1 | – | 0.95 | <0.001 |
| CAVI0 | 13.33 ± 2.68 | 13.37 ± 2.88 | 13.30 ± 2.56 | 0.877 | 0.95 | – | 1 | – |
| Age (years) | 63.06 ± 9.40 | 63.36 ± 9.77 | 62.86 ± 9.19 | 0.739 | 0.57 | <0.001 | 0.61 | <0.0001 |
| BMI (kg/m2) | 24.76 ± 3.60 | 25.24 ± 3.29 | 24.44 ± 3.77 | 0.165 | −0.06 | 0.41 | −0.06 | 0.451 |
| WC (cm) | 80.53 ± 9.90 | 85.78 ± 8.55 | 77.05 ± 9.20 | <0.001 | −0.03 | 0.673 | −0.03 | 0.684 |
| HC (cm) | 93.92 ± 6.93 | 94.81 ± 5.93 | 93.33 ± 7.49 | 0.183 | −0.1 | 0.18 | −0.11 | 0.170 |
| ABI | 1.10 ± 0.06 | 1.12 ± 0.06 | 1.10 ± 0.05 | 0.021 | 0.08 | 0.296 | −0.01 | 0.897 |
| SBP (mmHg) | 130.10 ± 17.37 | 134.09 ± 16.57 | 127.45 ± 17.47 | 0.016 | 0.3 | <0.001 | 0.33 | <0.0001 |
| DBP (mmHg) | 80.74 ± 10.40 | 84.16 ± 10.29 | 78.46 ± 9.89 | <0.001 | 0.18 | 0.016 | 0.06 | 0.461 |
| HR (bpm) | 69.01 ± 9.38 | 69 ± 9.04 | 69.02 ± 9.65 | 0.989 | −0.09 | 0.216 | −0.13 | 0.092 |
| MBP (mmHg) | 97.19 ± 12.04 | 100.81 ± 11.82 | 94.79 ± 11.63 | 0.001 | 0.25 | 0.001 | 0.19 | 0.014 |
| T2DM | 25 (15.34) | 10 (15.38) | 15 (15.31) | 0.989 | – | – | – | – |
| HTN | 56 (34.57) | 26 (40) | 30 (30.93) | 0.234 | – | – | – | – |
| IHD | 14 (8.59) | 9 (13.85) | 5 (5.10) | 0.083 | – | – | – | – |
| FH | 45 (27.95) | 19 (30.16) | 26 (26.53) | 0.719 | – | – | – | – |
| SMK | 34 (20.86) | 32 (49.23) | 2 (2.04) | <0.001 | – | – | – | – |
| Pack-year | 0.86 ± 4.76 | 2.17 ± 7.38 | 0 | 0.004 | 0.11 | 0.129 | 0.14 | 0.073 |
| Habit Alc. | 103 (63.19) | 26 (40) | 77 (78.57) | <0.001 | – | – | – | – |
| Alc. vol. (cc) | 51.83 ± 153.65 | 117.29 ± 235.74 | 17.30 ± 60.75 | <0.001 | 0.02 | 0.726 | 0.05 | 0.595 |
| Hab. Exe. | 108 (66.26) | 44 (67.69) | 64 (65.31) | 0.453 | – | – | – | – |
| Exe. Freq. per week | 3.28 ± 3.34 | 3.57 ± 3.69 | 3.09 ± 3.09 | 0.371 | 0.08 | 0.259 | 0.11 | 0.151 |
| GAD-7 | 1.55 ± 2.49 | 1.20 ± 1.98 | 1.75 ± 2.76 | 0.135 | −0.15 | 0.041 | −0.18 | 0.019 |
BMI, body mass index; WC, waist circumference; HC, hip circumference; HR, heart rate; SMK, ever smoking cigarette; Pack-year, pack-years of smoking; Habit Alc., habit of alcohol drinking; Alc. Vol., alcohol volume consumption in a week; Hab. Exe, habit of doing exercise; Exe. Freq. per week, frequency of exercise per week; GAD-7, generalized anxiety disorder index (p-values of Fisher exact and ANOVA tests).
Characteristics of study participants stratified by sex
The Pearson correlation of CAVI and CVAI0 with GAD-7 overall score was −0.15 (p = 0.041) and −0.18 (p = 0.019) respectively (GAD-7 results can be seen in Table S5 of the Supplementary Material). Prediction eclipse of Pearson’s correlation analysis between CAVI and CAVI0 with age, MBP, DBP and SBP can be seen in Figure 1.
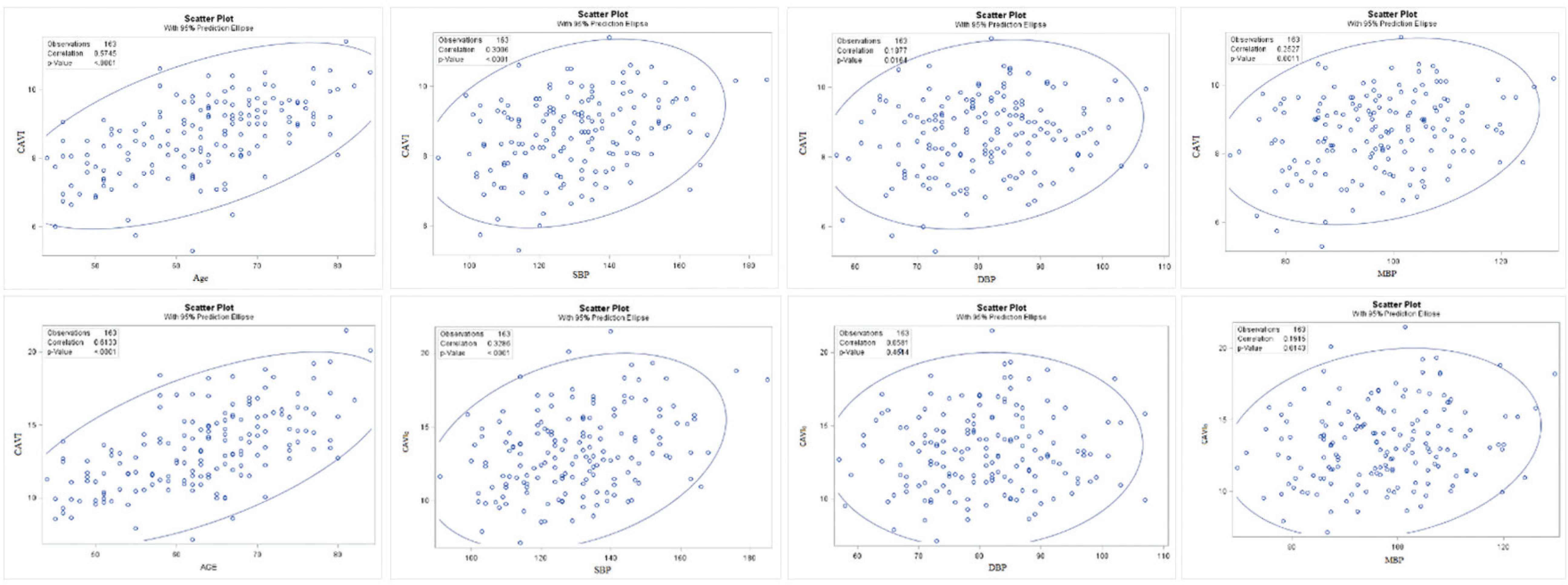
Scatter plots and 95% prediction eclipse of CAVI and CAVI0 with systolic blood pressure, diastolic blood pressure, mean blood pressure and age.
Results of the multiple linear regression models can be found in Table 2.
| Model 1 | Model 2 | Model 3 | Model 4 | |||
|---|---|---|---|---|---|---|
| CAVI | Age (years) | B | 0.066 | 0.061 | 0.066 | 0.064 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | ||
| SBP (mmHg) | B | – | 0.011 | – | – | |
| p | – | 0.005 | – | – | ||
| DBP (mmHg) | B | – | – | 0.019 | – | |
| p | – | – | 0.003 | – | ||
| MBP (mmHg) | B | – | – | – | 0.017 | |
| p | – | – | – | 0.002 | ||
| CAVI0 | Age (years) | B | 0.17 | 0.16 | 0.17 | – |
| p | <0.001 | <0.001 | <0.001 | – | ||
| SBP (mmHg) | B | – | 0.031 | – | – | |
| p | – | 0.001 | – | – | ||
| MBP (mmHg) | B | – | – | 0.028 | – | |
| p | – | – | 0.042 | – | ||
CAVI: Model 1 = age; Model 2 = age, SBP; Model 3 = age, DBP; Model 4 = age, MBP; CAVI0: Model 1 = age; Model 2 = age, SBP; Model 3 = age, MBP.
Linear multiple regression for CAVI and CAVI0
Median CAVI and CAVI0 was set as the cut-off point for the logistic regression analysis. Results of these models can be found in Table 2. The odds ratio and confidence interval of having a CAVI and CAVI0 greater than the median cut-off point is shown in Table 3.
| Model 1 | Model 2 | Model 3 | Model 4 | |||
|---|---|---|---|---|---|---|
| CAVI | Age (years) | OR (CI) | 1.14 (1.09 − 1.19) | 1.13 (1.08 − 1.19) | 1.14 (1.09 − 1.20) | 1.14 (1.09 − 1.19) |
| p | <0.001 | <0.0001 | <0.0001 | <0.0001 | ||
| SBP (mmHg) | OR (CI) | – | 1.01 (0.99 − 1.03) | – | – | |
| p | – | 0.1368 | – | – | ||
| DBP (mmHg) | OR (CI) | – | – | 1.09 (0.99 − 1.06) | – | |
| p | – | – | 0.1540 | – | ||
| MBP (mmHg) | OR (CI) | – | – | – | 1.02 (0.99 − 1.05) | |
| p | – | – | – | 0.1260 | ||
| CAVI0 | Age (years) | OR (CI) | 1.17 (1.11–1.23) | 1.16 (1.10 − 1.22) | 1.16 (1.11 − 1.23) | – |
| p | <0.0001 | <0.0001 | <0.0001 | – | ||
| SBP (mmHg) | OR (CI) | – | 1.01 (0.99 − 1.03) | – | – | |
| p | – | 0.1517 | – | – | ||
| MBP (mmHg) | OR (CI) | – | – | 1.007 (0.97 − 1.03) | – | |
| p | – | – | 0.6457 | – | ||
CAVI: Model 1 = age; Model 2 = age, SBP; Model 3 = age, DBP; Model 4 = age, MBP; CAVI0: Model 1 = age; Model 2 = age, SBP; Model 3 = age, MBP.
Logistic regression analysis of CAVI and CAVI0 greater than median cut-off point
4. DISCUSSION
This study performed on 163 community dwelling individuals suggesting that CAVI is significantly correlated with age, SBP, DBP, MBP and CAVI0 is significantly correlated with age, SBP and MBP. CAVI0 is not correlated with DBP. CAVI and CAVI0 are significantly correlated with BUN and also with HBA1c. None of blood pressure indices were associated with high CAVI and high CAVI0 independent of age.
Results of this study confirms that CAVI and CAVI0 are associated significantly and independently only to age. The fact that only age has independent effects on these indices can help to build reliable models to define individuals at the risk of atherosclerosis and CVD events, cfPWV although other studies had shown non consistent results. Bayes et al. [17] showed that CAVI is significantly different in men and women, also cardiovascular risk factors are associated with CAVI. Our results are not consistent with their study. In the study of Tabara et al. [18] the correlation of CAVI and age, SBP and BMI was 0.58, 0.17 and −0.20 respectively. These results are consistent with our study results except our study found no significant correction between CAVI and BMI. They also found CAVI higher in males but we found this difference not significant. It might be due to the smaller sample size of our study.
Our study showed a significant correction between CAVI and CAVI0 with BUN and HBA1c. Gomez-Marcos et al. [19] found out that CAVI is correlated positively with age, HBA1c, SBP, and DBP, and negatively correlated with waist circumference and BMI. Although they found out that there are more diabetic patients in the high CAVI group, HBA1c was not assessed in their study. However, the significant correlation between CAVI and HBA1c was also observed and confirmed by our study. About BUN serum levels, we found it significantly correlated to CAVI (r = 0.20, p = 0.009) and CAVI0 (r = 0.22, p = 0.004). The Literature is ambiguous regarding this relationship, Park et al. [20] found no difference between BUN serum levels and different levels of CAVI, on the other hand Liu et al. [14] found them significantly correlated (r = 0.231, p < 0.05). The relationship also might be because of other factors in the study.
Although the effects of body weight reduction and exercise have been shown to have an important effect on reduction of arterial stiffness [21] our study just confirmed a negative nonsignificant relationship between BMI and CAVI. Beneficial effects of exercise on anti-oxidation state, blood glucose level, angiogenesis and endothelial functions can be a reason for the negative relationship between these measures [22].
Although anxiety has been shown to have an important effect on CVD mortality [23], its role in the arterial stiffness and atherosclerosis is controversial [19]. Our study showed the significant and negative correlation (−0.15, p = 0.041) between GAD and CAVI and a negative correlation (−0.18, p = 0.019) between GAD and CAVI0. Yeragani et al. [24] showed that arterial stiffness is significantly higher in the patients with high anxiety. Our study results are in contrast with their findings. However, after controlling for the other risk factors in the regression models, anxiety showed no significant independent association with CAVI.
There are some differences between how CAVI0 is calculated and the most important one is that CAVI0 do not use SBP in its formula. It is worth noting that CAVI0 has been doubted because it has high cross-sectional dependency on the DBP [25]. This dependency, however, can potentially be explained from the typical increase in pulse pressure that is associated with an increase in arterial stiffness [26]. This might explain the fact that CAVI0 does not have a significant correlation with SBP in our study. In a study Shirai et al. [27] observed a negative correlation between DBP and CAVI0 which could be explainable as the subjects of their study with stiffer arteries had normal SBP, thus should have lower DBP because of the fact that people with stiffer arteries have larger pulse pressure [26]. This cannot be applicable for our study, therefore there is no significant correlation between DBP and CAVI0 in our study. The other fact that should be taken into account is that SBP and DBP are both important in the evaluation of the risk assessment of hypertension complications. As uncontrolled DBP is associated with a greater risk of CVD events and uncontrolled SBP is more associated with poorer prognosis [28], when evaluating the results of CAVI0, we should consider that this index maybe not reflective of DBP in the patient.
5. CONCLUSION
Among all the factors that have some association with CAVI in community dwelling individual, only age could be served as independent factors influencing CAVI and CAVI0. As SBP and DBP are not independently associated with CAVI and CAVI0, these indices could be considered reliable in differentiating people with high risks of CVD, as it is not dependent on other risk factors. As CAVI0 is not correlated with DBP, when evaluating the results of CAVI0, we should consider that this index maybe not be reflective of DBP in the patient.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
CB and LL contributed in conceptualization. JA and AA contributed in data curation and writing the original draft. JA contributed in formal analysis. CB and TT contributed in investigation. JA and CB contributed in methodology. SVW contributed in resources and validation. JA and TT contributed in writing the review and editing. SW contributed in visualization. NH and CB contributed in funding acquisition. JA and NH contributed in software. CB contributed in supervision and project administration.
FUNDING
No financial support was provided.
SUPPLEMENTARY MATERIALS
Supplementary data related to this article can be found at
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Li-Ju Lin AU - Nan-Chen Hsieh AU - Shu-Fang Vivienne Wu AU - Tan-Hsu Tan AU - Azadeh Alizargar AU - Chyi-Huey Bai AU - Javad Alizargar PY - 2020 DA - 2020/12/08 TI - Factors Associated with Cardio Ankle Vascular Index (CAVI) and its Mathematically Corrected Formula (CAVI₀) in Community Dwelling Individuals JO - Artery Research SP - 53 EP - 58 VL - 27 IS - 2 SN - 1876-4401 UR - https://doi.org/10.2991/artres.k.201124.002 DO - 10.2991/artres.k.201124.002 ID - Lin2020 ER -
