Venous thromboembolism risks and prophylaxis in King Fahad Hospital, Madinah, Saudi Arabia
- DOI
- 10.1016/j.jegh.2017.09.003How to use a DOI?
- Abstract
Objective: To evaluate the risk factors, physician’s compliance, and implementation of the American College of Chest Physicians (ACCP) guidelines for venous thromboembolism (VTE) prophylaxis at our hospital.
Methods: A retrospective cohort study was conducted in King Fahad Hospital, Madinah, Saudi Arabia, from July 2015 to September 2015. We used the ACCP 2012 guidelines to assess the VTE risk and to determine whether patients had received the recommended prophylaxis. All hospital inpatients aged 14 years or older were assessed for risk of VTE by reviewing the hospital chart. The primary endpoint was the rate of appropriate thromboprophylaxis.
Results: A total of 414 patients were studied. Their mean age was 47.74 ± 20.4 years, and 208 (50.2%) were female. There were 292 (70.5%) patients at high risk and 73 (17.6%) at moderate risk. As per the ACCP criteria, 375 (90.5%) patients were at risk for VTE and qualified for prophylaxis. Although 227 (60.5%) received some form of prophylaxis, only 144 (38.4%) of them received ACCP-recommended VTE prophylaxis.
Conclusion: In our hospital, most of the patients are at high risk for developing VTE. The VTE prophylaxis guideline is not properly implemented and is underutilized. Strategies should be developed and implemented to ensure patient safety.
- Copyright
- © 2017 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Introduction
Venous thromboembolism (VTE) is a potential life-threatening complication that can arise during hospitalization for surgery or for medical illness [1,2]. The vast majority (80%) of hospitalized patients with symptomatic VTE are nonsurgical patients [3–5]. Furthermore, 70% to 80% of cases of fatal pulmonary embolism in the hospital occur in medical patients [6–8].
The worldwide incidence of VTE is difficult to quantify, as clinical symptoms can be nonspecific and screening techniques can fail to properly assess nonsymptomatic patients. Even so, it is thought that at least 5–15% of hospitalized medical patients will develop VTE, making it the most common preventable cause of in-hospital death [1,2].
The incidence of hospital-acquired deep venous thrombosis with confirmed objective diagnosis is 10–40% among surgical and medical patients. However, this incidence rises to 40–60% after major orthopedic surgery [7–9].
The American College of Chest Physicians (ACCP) released the latest updated guidelines in 2012, which defined the patient’s risk and recommendation of prophylaxis accordingly. Patients who fall into the high-risk group are estimated to have between 40% and 80% risk of developing VTE if no prophylaxis is provided [10]. Recommended prophylaxis measures include: treatment with low molecular weight heparin (LMWH), low-dose unfractionated heparin (UFH), or fondaparinux for patients undergoing major surgery. Mechanical methods of prophylaxis are urged for patients with a high bleeding risk [10]. Unfortunately, numerous international and national studies suggest that there is gap between guideline and practice. The ENDORSE study found that more than 50% of hospitalized patients should have received VTE thromboprophylaxis, but in fact only half of them actually received it [11]. The International Medical Prevention Registry on Venous Thromboembolism (IMPROVE) registry, an ongoing international registry of prophylaxis patterns in the medically ill, has shown that only 60% of potentially at risk patients are receiving any prophylaxis [12]. We conducted a retrospective study in order to determine the prevalence of the high-risk medical and surgical patient in our hospital and to evaluate the utilization of prophylaxis in this patient group. The primary endpoint was the rate of appropriate thromboprophylaxis.
2. Methods
2.1. Study design
We conducted a retrospective cohort study at King Fahad Hospital (Madinah, Saudi Arabia), a tertiary referral hospital with 400 beds. It manages all type of surgical (general surgery, orthopedic surgery, vascular surgery, and neurosurgical patients) and medical patients excluding obstetrics and gynecology. We reviewed all patients admitted to the hospital including critical care department between July 2015 and September 2015. The study protocol was approved by the Ethics Committee.
2.2. Patients
Inclusion criteria included: age 14 years and older; admitted to the hospital with medical and surgical problems for more than 3 days. Exclusion criteria included any patients on anticoagulation for therapeutic purpose or missing chart.
2.3. Data collection
The following data were collected from the medical charts: age, sex, and risk factors for VTE. We also included surgical or medical patients risk assessment and VTE prophylaxis given and compliance as per ACCP guidelines. We used the Caprini score for surgical patients and Padua score for medical patients.
2.4. Statistical analysis
Continuous variables were described as mean ± standard deviation for normally distributed variables and categorical variables as percentages. χ2 test was used to compare between categorical variables.
3. Results
A total of 460 patients admitted to King Fahad Hospital from July 1, 2015 to September 30, 2015 were initially screened; 46 patients were excluded for receiving therapeutic anticoagulation. Overall, 414 patients were included in the study.
The mean age of patients was 47.74 ± 20.4 years, and 208 (50.2%) were female. Thirty-one (7.5%) patients were younger than 20 years. Their baseline characteristics are shown in Table 1.
| N (%)/mean | |
|---|---|
| Mean age (y) | 47.74 ± 20.4 |
| Sex | |
| Male | 206 (49.8%) |
| Female | 208 (50.2%) |
| Risk factor | |
| DM | 143 (34.5%) |
| HTN | 148 (35.7%) |
| Stroke | 60 (14.5%) |
| Heart failure | 58 (14.0%) |
| Smoking | 65 (15.7%) |
| Venous catheter | 109 (26.3%) |
| Ischemic heart disease | 146 (35.3%) |
| COPD | 57 (13.8%) |
| Renal failure | 70 (16.9%) |
| Endocrine | 132 (31.9%) |
| Connective tissue disease | 22 (5.3%) |
| Surgery | 131 (31.6%) |
| Immobilized | 163 (39.4%) |
| Multiple trauma | 81 (19.6%) |
| Obesity | 137 (33.1%) |
COPD =; DM = diabetes mellitus; HTN =.
Patients’ baseline characteristics.
A total of 210 (50.7%) of patients were identified as surgery patients and 204 (49.3%) were medical patients Table 2.
| Risk classification | Surgical, 210 (50.7%) N (%) |
Medical, 204 (49.3%) N (%) |
|---|---|---|
| High | 173(82.3%) | 118 (58%) |
| Moderate | 24(11.4%) | 49 (24%) |
| Low | 13 (6.1%) | 37 (18.1) |
Distribution of patients according to risk stratification.
As per ACCP risk categorization, 173 (82.3%) surgical patients were classified as high risk and 24 (11.4%) as moderate risk.
A variety of prophylaxis methods were used including pharmacological “UFH” or “LMWH” (45.6%), intermittent pneumatic compression devices (2.4%), combination of intermittent pneumatic compression devices with pharmacological (6.8%), and no therapy (45.1%). These results are summarized in Fig. 1.
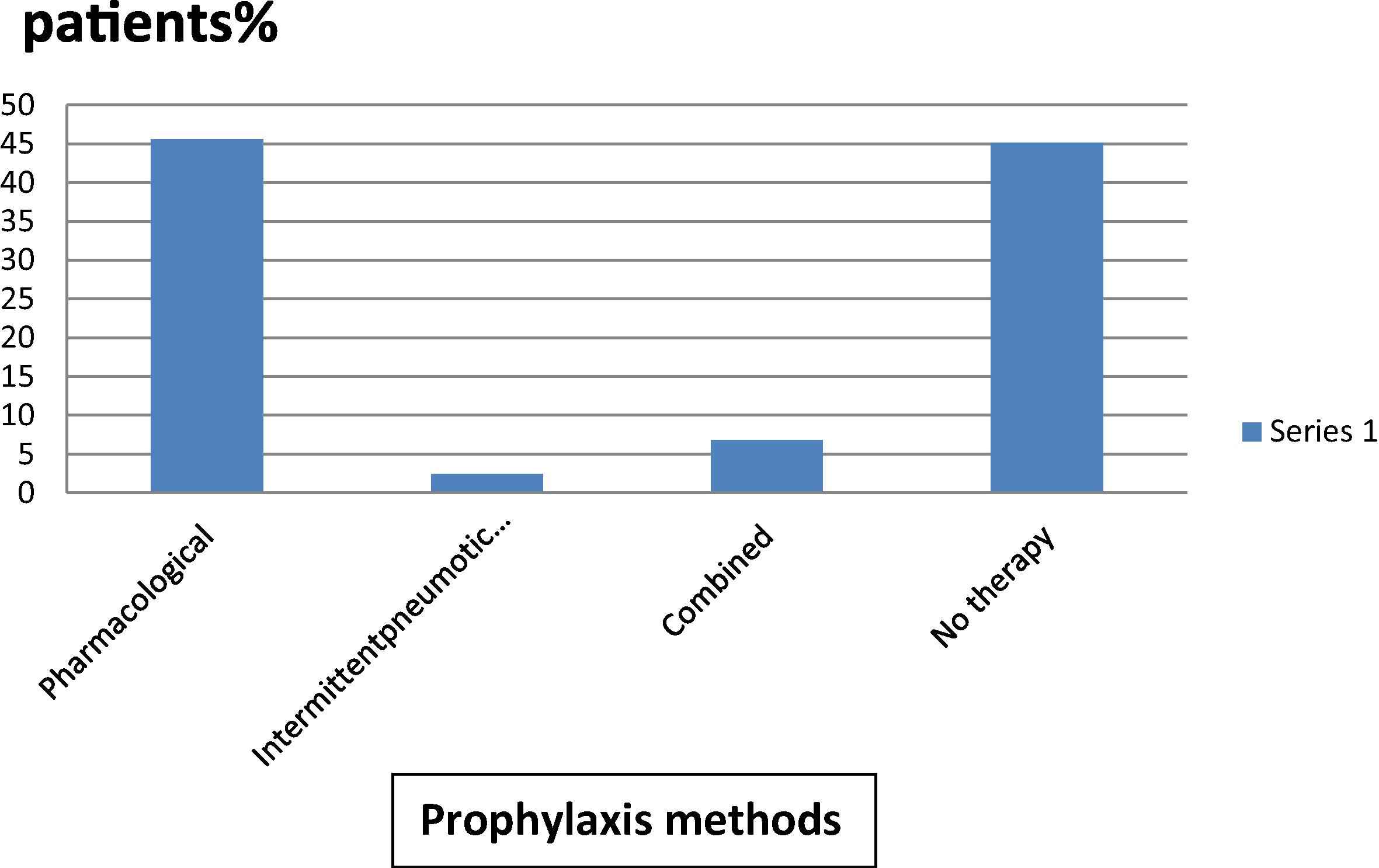
Prophylaxis methods used in the study group.
According to the ACCP criteria, 375 (90.5%) among surgical and medical patients were at risk of VTE and qualified for prophylaxis. Although 227 (60.5%) received some form of prophylaxis, only 144 (38.4%) of them received ACCP-recommended VTE prophylaxis.
More medical patients (112; 55%) received ACCP-recommended prophylaxis compared with surgical patients 32 (15%; p > 0.0001) (Fig. 2). Furthermore, patients in the high-risk group received prophylaxis more than patients in moderate- and lower-risks groups did. Indeed, 102 (35%) of high-risk patients and 46% of moderate-risk patients received no therapy (Fig. 3).
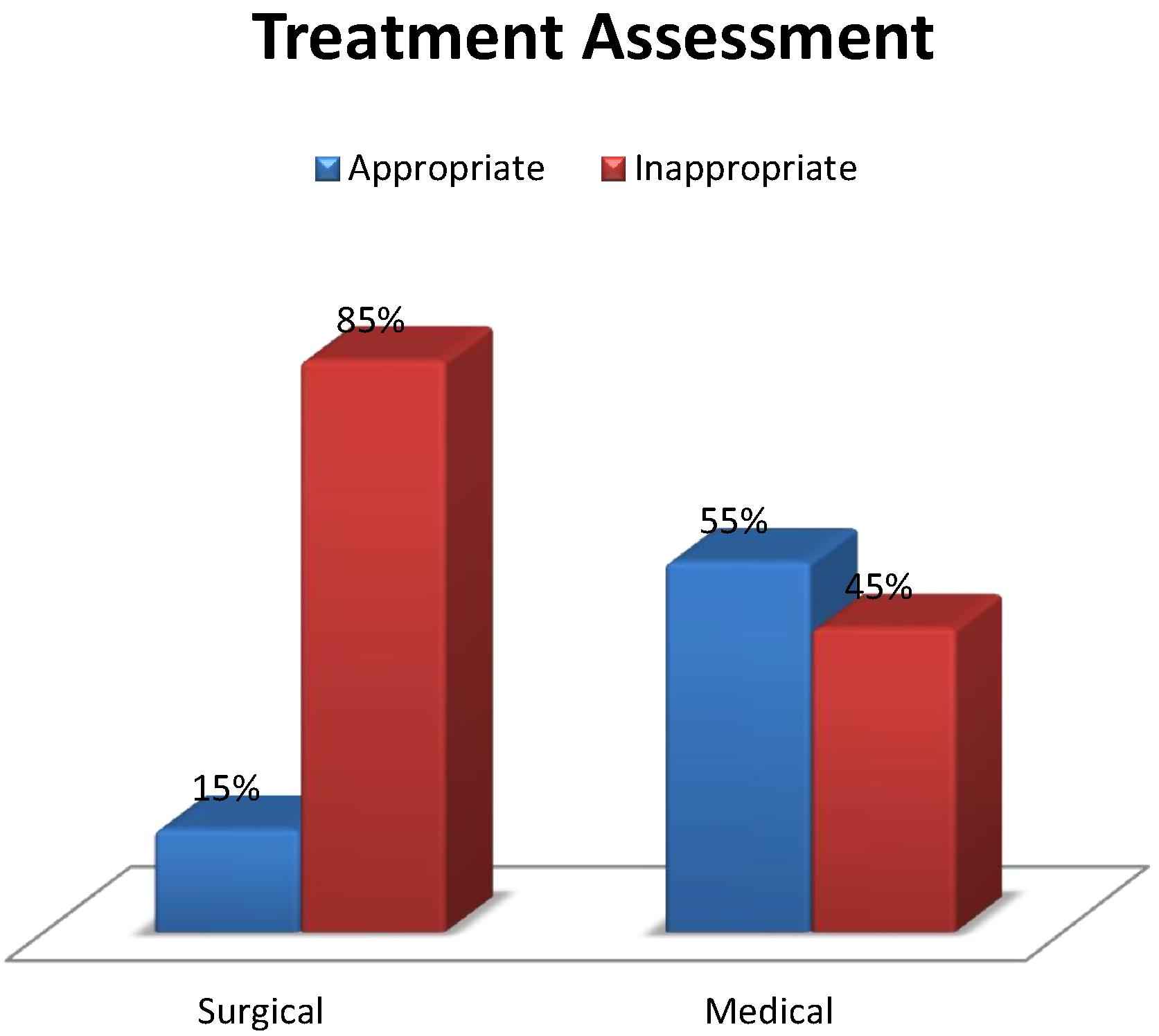
Caption.
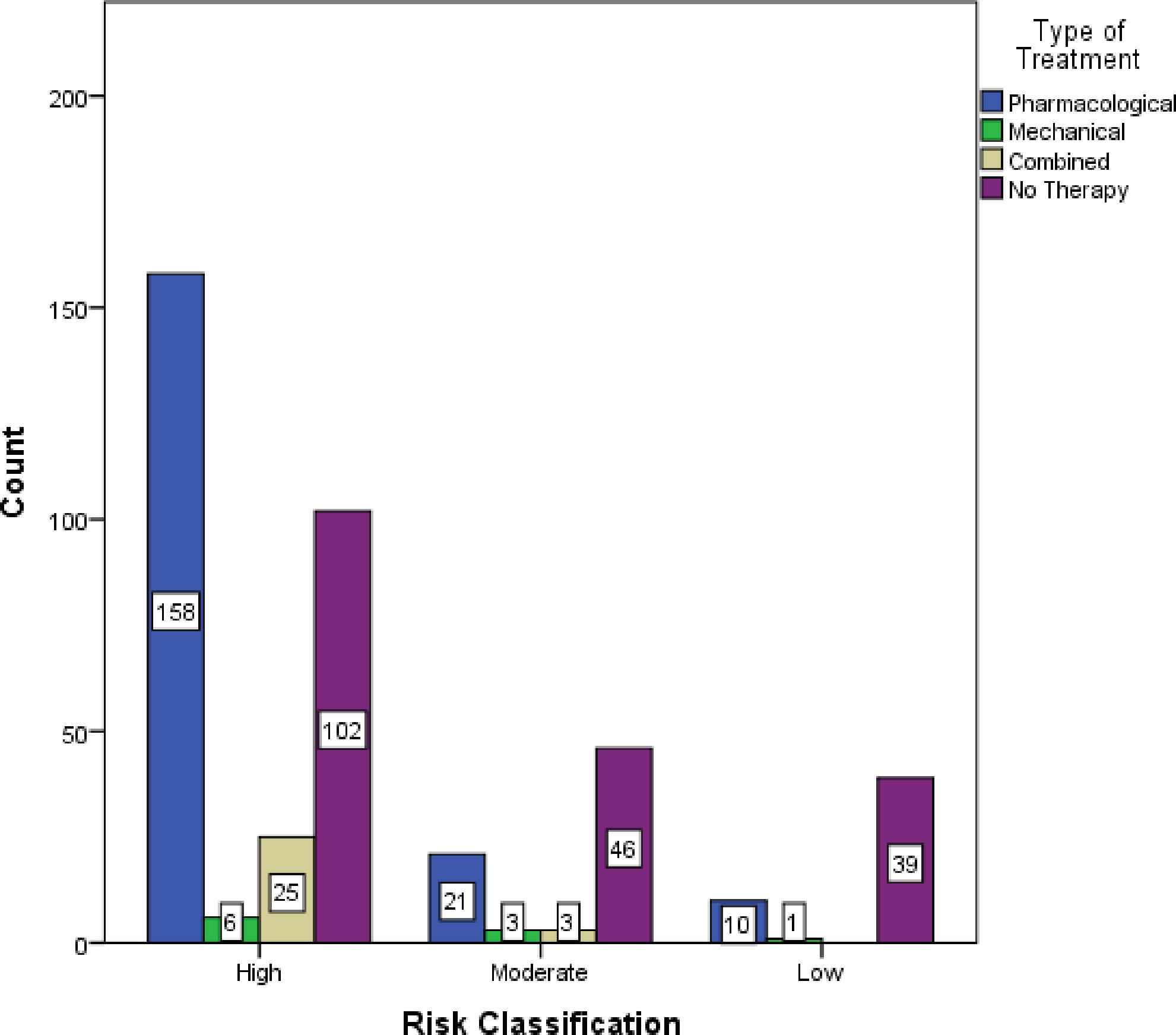
Prophylaxis among different risk categories.
4. Discussion
This is the first study conducted in our institute to evaluate the prevalence of at-risk medical and surgical patients. Our finding that 90.5% of our patients are at risk for VTE is consistent with the Canadian CURVE study and other studies, where 78–90% of all hospitalized patient groups had at least one major risk factor for VTE [9,13,14].
In our study, we found that only 38.4% of the patients who were eligible for prophylactic antithrombotic therapy actually received it. This is very closely similar to the finding of the national AVAIL ME study, which included 200 patients from Saudi Arabia, and found VTE prophylaxis and guideline applications ranging from 24% to 84% among different subgroups [15].
Overall, significantly more medical patients in our study received prophylactic antithrombotic therapy compared with surgical patients (p > 0.0001; 55% vs. 15%, respectively).
The multinational IMPROVE study [12] showed that only 60% of medical patients who are eligible for prophylactic antithrombotic therapy actually received it. This is almost similar to the 55% rate among the medical patients in our study.
Our medical patients received prophylaxis at a higher rate compared with the patients in the Canadian CURVE study, which showed that 90% of acutely ill medical patients had an indication for thromboprophylaxis; however, only 16% received appropriate prophylaxis [15].
The surgical patients in our study received prophylactic antithrombotic therapy at a significantly lower rate (15%) than the surgical patients in a similar local study from Jeddah (44.1%) [16].
Although our figures for thromboprophylaxis are, in general, lower than the reported numbers in the literature outside the Middle East region, the low incidence stays in accordance with many studies conducted in different countries, indicating the underutilization of thromboprophylaxis. Our study highlights the necessity of improving awareness regarding VTE risk and implementing the ACCP guidelines.
Finally, the retrospective data collection in a single hospital could be perceived as a methodological weakness. However, prospective patient data collection would have required informed consent at our institution. This could have affected the validity of our results by introducing potential bias, in that patients being asked to enroll in the study prospectively may have been more likely to ask their prescribing physicians about VTE prevention. This, in turn, could have led to increased prophylaxis rates that would not be an accurate reflection of real-world practice or of our intervention.
5. Conclusion
VTE is a major public health issue [17,18]. It is an easily preventable disease with a substantial risk of morbidity and mortality in patients hospitalized for acute medical and surgical illnesses [19,20].
Our data show that a large proportion of hospitalized individuals—both surgical and medical—are at risk for VTE, and that recommended VTE prophylaxis is underused. Hospital-wide strategies to assess patients’ VTE risk should be implemented, together with measures that ensure that at-risk patients receive the appropriate VTE prophylaxis. Among these are hospital accreditation programs that consider VTE risk assessment as one of the essential safety measures. As a result of this study, VTE risk assessment is mandatory for all patients admitted to our hospital.
References
Cite this article
TY - JOUR AU - Ayman Kharaba AU - Mohammad Al Aboud AU - Madinah Reham Kharabah AU - Khaled Alyami AU - Amal Al Beihany PY - 2017 DA - 2017/09/22 TI - Venous thromboembolism risks and prophylaxis in King Fahad Hospital, Madinah, Saudi Arabia JO - Journal of Epidemiology and Global Health SP - 295 EP - 298 VL - 7 IS - 4 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2017.09.003 DO - 10.1016/j.jegh.2017.09.003 ID - Kharaba2017 ER -
