MicroResearch: Finding sustainable local health solutions in East Africa through small local research studies
- DOI
- 10.1016/j.jegh.2014.01.002How to use a DOI?
- Keywords
- MicroResearch; Research capacity; Developing countries; Community health; Maternal child health; Global health
- Abstract
Background: Sub-Saharan African countries have urged grassroots input to improve research capacity. In East Africa, MicroResearch is fostering local ability to find sustainable solutions for community health problems. At 5 years, the following reports its progress.
Methods: The MicroResearch program had three integrated components: (1) 2-week training workshops; (2) small proposal development with international peer review followed by project funding, implementation, knowledge translation; (3) coaching from experienced researchers. Evaluation included standardized questions after completion of the workshops, 2013 online survey of recent workshop participants and discussions at two East Africa MicroResearch Forums in 2013.
Results: Between 2008 and 2013, 15 workshops were conducted at 5 East Africa sites with 391 participants. Of the 29 projects funded by MicroResearch, 7 have been completed; of which 6 led to changes in local health policy/practice. MicroResearch training stimulated 13 other funded research projects; of which 8 were external to MicroResearch. Over 90% of participants rated the workshops as excellent with 20% spontaneously noting that MicroResearch changed how they worked. The survey highlighted three local research needs: mentors, skills and funding – each addressed by MicroResearch. On-line MicroResearch and alumni networks, two knowledge translation partnerships and an East Africa Leaders Consortium arose from the MicroResearch Forums.
Conclusion: MicroResearch helped build local capacity for community-directed interdisciplinary health research.
- Copyright
- © 2014 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Background
In 2013, the United Nations proposed the Action Agenda for Sustainable Development Goals (Action Agenda) [1] as a means of building on the achievements of the Millennium Development Goals (MDG), including those in health [2]. In limited resource countries, developing local capacity to improve on health gains as proposed in the Action Agenda will continue to be a major challenge since these countries bear 25% of the global disease burden but have less than 1% of its healthcare professionals [3]. Local research could help by finding local solutions for community health problems. However, capacity and resources for research within these countries are often limited. The 2008 Bamako “Call to Action” from the Global Ministerial Forum on Research for Health highlighted three critical objectives to enhance the capacity of the world’s poorer nations to improve health for their citizens through research: (1) achieve greater equity in research; (2) make knowledge translation linking evidence to policy-making a priority; (3) create stronger institutions for research [4]. The research gap for limited resource countries remains a major problem as they receive only 2% of global research funding. In addition, much of the research undertaken in these countries is driven by the needs of industrialized countries for access to patient populations and data collection at modest cost [5].This research model fails to expand local research capacity and to find the evidence needed to drive local policy.
Both the MDG and the Action Agenda encourage national and/or regional strategies and collaborations to address complex health problems. However, local health problems need sustainable, culturally appropriate community solutions to improve local health outcomes if the objectives of the Action Agenda are to be achieved.
MicroResearch (http://microresearch.ca/) is an innovative program developed in 2008 in East Africa aimed at enhancing the capacity of local healthcare professionals to find local solutions for community health problems that can then influence health programs and/or government policy [6]. MicroResearch has borrowed the principles of microfinance (train, coach and provide capital) while trying to avoid microfinance program problems, such as the negative impact of repayment of high interest loans and the focus on the poorest of the poor rather than on poor local entrepreneurs [7]. In place of small loans, MicroResearch provides small non-repayable research grants to teams of healthcare professionals keen to address community health problems through the development of their own scientifically credible research proposals. The MicroResearch program has three integrated components: (1) 2-week long training workshops; (2) small grant proposal development with international peer review followed by project funding, implementation and knowledge translation; (3) coaching throughout the entire process from experienced researchers (Fig. 1). As MicroResearch in East Africa is now five years old, the following study reports on its early outcomes and lessons were learned.
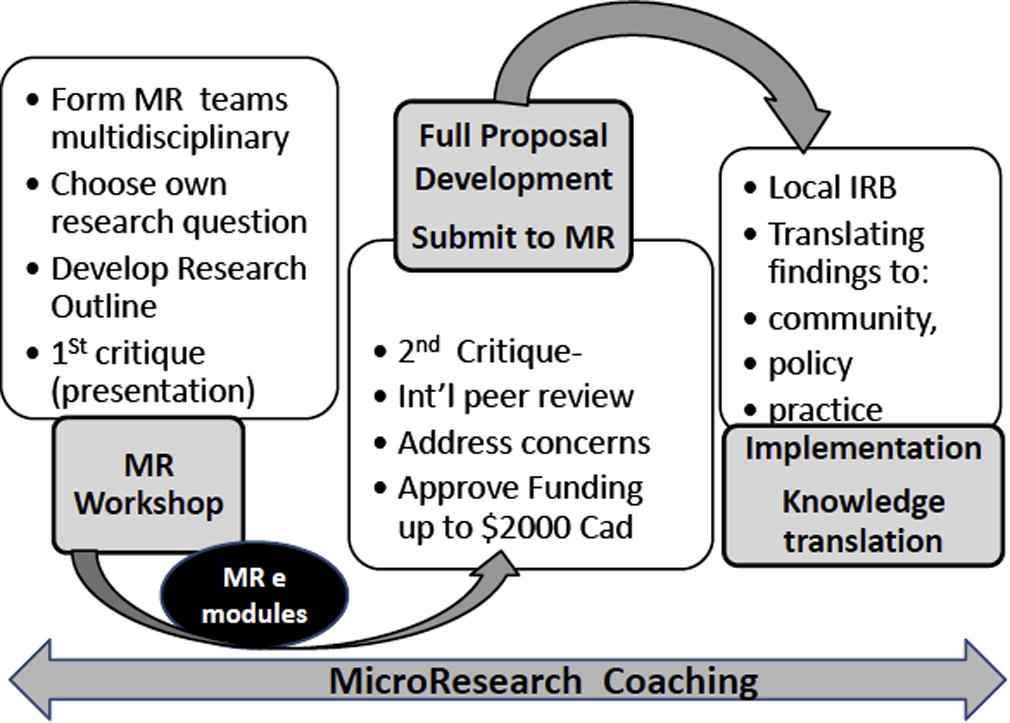
MicroResearch program overview.
2. Methods
Initially in 2008, then annually since 2010, 2-week long training workshops were carried out at each participating MicroResearch site in East Africa. Based upon initial local advice, these 10-day workshops were limited to half days to allow participating healthcare professionals to attend to clinical responsibilities in the off time. Participants were recruited through local posters, word of mouth, and direct invitations developed by the local MicroResearch site leaders. Participation from any one discipline, such as nursing or medicine, was limited to no more than 50% of participants in a workshop. Professionals from non-health disciplines (e.g., engineering, information technology, library sciences, etc.) were encouraged to participate in the training if their interests complimented healthcare needs.
At each workshop, participants were divided into interdisciplinary teams of 6–8 to learn the principles of health research, community engagement, and knowledge translation through “hands on” development of a research proposal outline (Table 1). As homework from Day 1, each participant was invited to formulate a community-directed research question to propose to their team on Day 2. Each team then reviewed the proposed questions and selected the best one, based on criteria learnt on Day 1. Over the remainder of the workshop, each team refined their chosen question, developed a draft research outline and prepared a 10-min oral presentation of their outline. Each team was supported by a team workshop coach, and the daily lectures focused on knowledge and skills needed to develop a research proposal. On Day 10, the first formal critique and feedback on the research outlines occurred after each team presented their 10-min summary and answered questions. A panel of senior faculty from the host site offered constructive criticisms of each research outline and judged whether the research outline should be developed into a full MicroResearch application and, if so, how it might be enhanced. The workshop curriculum was supplemented with on-line MicroResearch modules covering different research aspects to support the development of research knowledge and skills.
| Week 1 | Week 2 | ||
|---|---|---|---|
| Day 1 | Welcome and introduction of faculty and participants Introduction to the Workshop and Objectives Introduction to the Web program Defining the research question Team activity: Each course participant challenged to identify a community-directed research question from their own experience |
Day 6 | Writing an Abstract Exercise Oral and Poster exercise Team activity: Refine outline, consider budget |
| Day 2 | Principles of Clinical Research Pitfalls in Research Getting started on writing a proposal Team activity: The team selects one of the questions to develop into a research outline |
Day 7 | Principles of Knowledge- Translation Moving Research into Policy Exercise Team activity: Further refine outline |
| Day 3 | What editors are looking for Team Reports – question selected and why Team activity: Refine research question; introduction team to their local coach |
Day 8 | Principles of Knowledge-Translation Moving Research into Policy** Team activity: Refine outline, develop oral presentation |
| Day 4 | How a manuscript is reviewed Basics and Local Research Ethics Team activity: Develop proposal background outline |
Day 9 | Career Documentation Team activity: “Polish” outline for presentation |
| Day 5 | Grant proposal review Writing a report Team activity: Refine background, looks at methodology, consider ethics for outline |
Day 10 | Each MicroResearch Team presents research outline to judges Team Activity: constructive critique of each presentation, Awards and Graduation Ceremony |
MicroResearch workshop outline.
After the workshop, a local East African and an online Canadian or American MicroResearch coach helped each team judged worthy of moving on to develop a full research application to one of the twice yearly MicroResearch grant opportunities (grants up to $2000 CAD). All submissions underwent an international (Canadian, American and East African) peer review. If ranked in the fundable range, the team, with the help of their coaches, then had the opportunity to further improve their proposal by addressing reviewers’ comments and concerns. When the proposal was refined sufficiently to merit grant support, funding was approved pending local institutional ethics board approval at their site. The team then carried out the project with coach support. If a proposal was not deemed to be in the fundable range at peer review, the team was encouraged to work with their coach to revise the proposal for submission to the next MicroResearch grant opportunity. Each participating East Africa MicroResearch grant administering site was provided with overhead support ($400 per grant) to cover local ethics board review and grant administration costs. Initially funds were also given to cover the material costs of each workshop, but in 2013, based upon local site advice, each site began charging a workshop fee of $25–50 CAD per participant. Of note, participants were never paid to attend the workshops and local site teachers and coaches received only small honorariums.
As knowledge translation is a key component in MicroResearch to ensure that the local community benefits from the research findings, each application required a knowledge translation plan. Once the study was completed, their coaches helped the team implement their plan. Plans might have included feedback to communities, reports to government departments, curriculum changes, healthcare program changes, etc. The MicroResearch program also provided coaching and extensive internal peer review support upon project completion for the team to write an extended project abstract for submission to one of the four Pub Med journals that have abstract publication agreements with MicroResearch.
Feedback from the East African MicroResearch participants and site leaders was solicited in several ways. To assess workshops, participants were invited to complete an anonymous standardized evaluation questionnaire after each workshop. The questionnaire included both closed- and open-ended questions, and findings were used to modify the next workshop’s content, lectures, participant exercises, and to evaluate impact. To assess perceived local health problems, research needs and obstacles in East Africa, recent (2012) workshop participants and the local MicroResearch site and other leaders at the five East African sites were invited to complete an online survey in February 2013.
In order to enhance the sharing of MicroResearch project ideas and results locally within East Africa and to develop a local sustainability plan, two East African MicroResearch Forums were held with invitees from the five sites, one organized with Makerere University in March 2013 [8] and one with the University of Nairobi in November 2013 [9]. These were followed by standardized evaluation questionnaires.
3. Results
Between 2008 and 2013, 15 MicroResearch workshops were conducted at five East African locations: in Uganda at Mbarara University of Science and Technology (MUST) (5 workshops) and at Makerere University (MU) (4 workshops), in Kenya at the University of Nairobi (3 workshops), Aga Khan University (1 workshop) and in Tanzania at the Tanzanian Training Centre for International Health (TTCIH) (2 workshops) (Table 2). By the end of 2013, a total of 391 participants from a wide range of disciplines had been trained (Fig. 2). Physicians, nurses and midwives made up about 45–50% of the participants of each workshop. The addition of the small workshop fee charged in 2013 did not appear to change workshop diversity nor hamper participant recruitment. Daily workshop attendance ranged from 80% to 100%. With the workshop fee charge, daily attendance rates were over 90%.
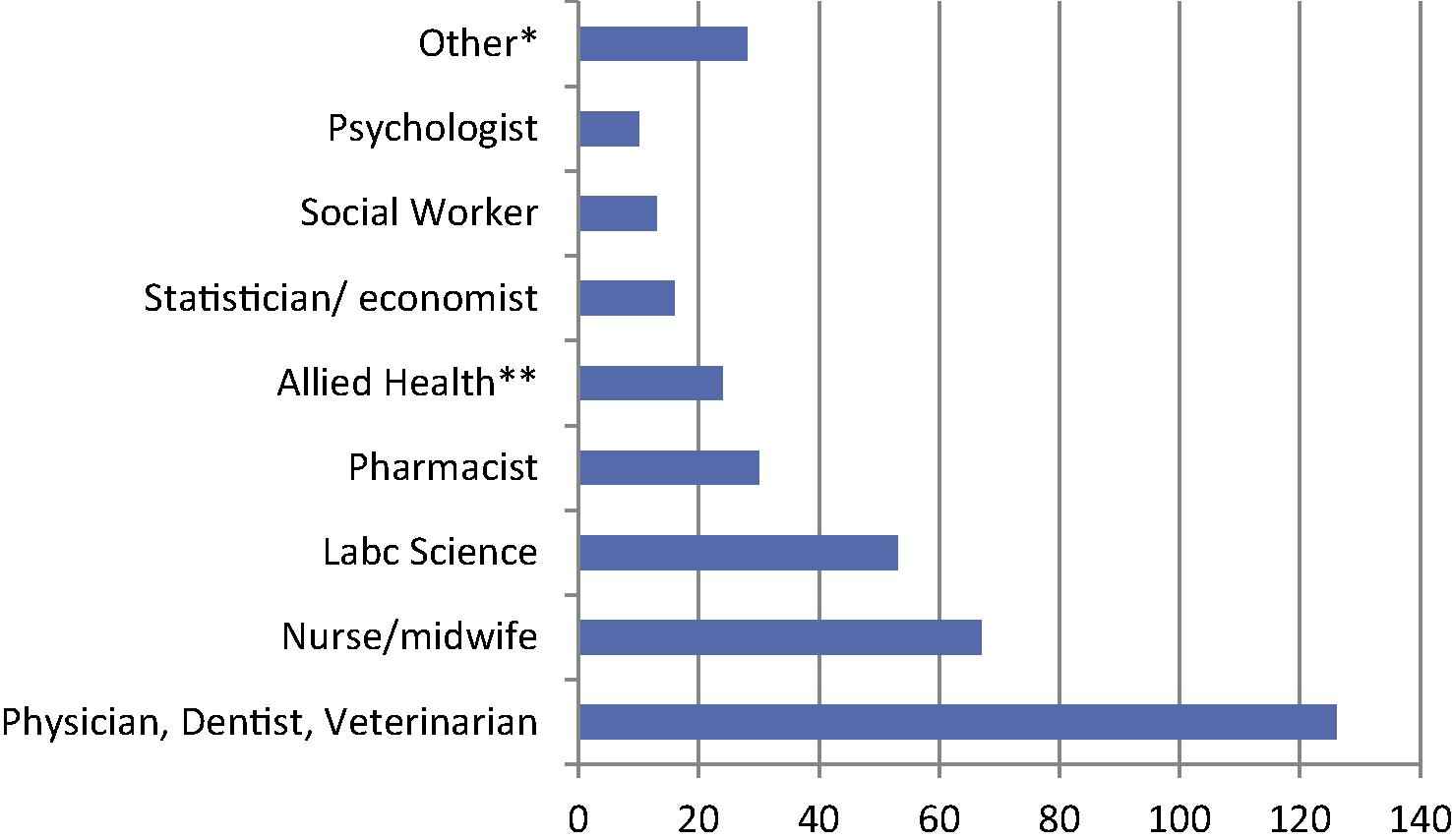
Disciplines of 368 of 391 MicroResearch workshop participants (excludes 23 where discipline not stated). *Other = information technologists, computer science, ethno-botanists, librarians, accountants, engineers, etc. **Allied health: occupational therapy, physiotherapy, nutritionist, dental technician, etc.
| Number | 2008 | 2010 | 2011 | 2012 | 2013 | Total |
|---|---|---|---|---|---|---|
| Healthcare professionals and others trained | 22 | 48 | 64 | 152 | 105 | 391 |
| Training sites | 1 | 2 | 3 | 5 | 4 | NA |
| MicroResearch team proposal outlines developed in workshops | 3 | 7 | 10 | 20 | 16 | 56 |
| Full MicroResearch proposals submitted for international peer review | 1 | 6+2* | 10+1* | 13+2* (3**) |
2 N/A (2**) | 37 |
| Proposals approved for funding in principle | 1 | 8*** | 9*** | 11 | N/A | 29 |
| Projects completed as of Sept 2013 | 1 | 6 | N/A | N/A | N/A | 7 |
N/A: not applicable as insufficient time since workshop to submit a full proposal or complete the funded project.
Additional proposals from previously successful MicroResearch workshop graduates who formed new teams with proposals not originating from a MicroResearch workshop; attributed to year proposal was submitted.
Proposals submitted to November 2013 competition.
Includes 3 projects funded in part or in full outside of MicroResearch.
Summary of 15 workshops and outcomes by year up to 2013: MicroResearch team projects attributed to year team formed.
Table 2 summarizes the workshops and the outcomes of the research outlines developed in the workshops. In the first four years, i.e., including the 2012 workshop teams, 40 research outlines were started in workshops with 30 (75%) that were further refined and submitted to a MicroResearch grants competition. Of note, all but 3 teams required at least a year to expand their outline into a full MicroResearch application. Although teams formed in the 2013 workshops had little time to develop an application for the November 2013 competition, 2 managed to do this. For these 32 proposals, the principal investigator for each was a woman in 18 (56%) of the 32 proposals. In addition to these 32 applications, a further 5 previously successful MicroResearchers formed new teams to address other community-directed research questions through new applications. Thus altogether, 37 applications had been submitted for funding by the end of 2013 with the 5 from November 2013 newly under review. Of 32 with peer review and refinement processes completed, 29 (91%) were approved for MicroResearch grants based upon scientific merit. Three were sent back with recommendations to reapply after deficiencies were addressed. Two of the 29 did not need MicroResearch grants as funds were obtained externally, and a third obtained additional support to supplement their MicroResearch grant. In addition to the 2 fully out-funded projects coached by MicroResearch, at least 8 other projects developed by MicroResearch training graduates had been undertaken and were completed external to MicroResearch by 2013.
Of the 29 MicroResearch grant-supported projects, 14 (48%) were from Mbarara University of Science and Technology in Uganda, the longest running MicroResearch program. Of these 29, 10 (35%) focused on child health, 12 (41%) on maternal health, and 7 (24%) on both mothers and children. Table 3 presents 12 examples of MicroResearch projects: 5 completed, 5 funded and underway, and 2 reviewed in the fundable range undergoing minor refinement.
| Year team started | Title | Site and principle investigator | Project status |
|---|---|---|---|
| 2008 | Assessment of activities and impact of community-owned resource persons (CORPS) on families and communities in Healthy Child Uganda Bwizibwera Project Area | Mbarara University of Science and Technology, Uganda Basil Tibanyendera |
Completed Reported [10] and used to change policy |
| 2010 | No benefit of glutamine supplementation on persistent diarrhea in Ugandan children | Makerere University, Uganda Justine Kamuchaki |
Completed Published [11] Supported no change in health practice |
| Knowledge and practices of women regarding prevention of mother-to-child transmission of HIV (PMTCT) in rural south-west Uganda | Mbarara University of Science and Technology, Uganda Barnabas Atwiine |
Completed Extended Abstract Published [12] Knowledge translation in progress |
|
| Healthy Child Uganda survey on village health team knowledge, attitudes and behavior of VHTs towards their responsibilities in Mbarara District | Mbarara University of Science and Technology, Uganda Ashaba Scholastic |
Completed Extended Abstract Published [13] Led to changes in training, support programs |
|
| The practice of traditional rituals and customs in newborns by mothers in selected villages in south–west Uganda | Mbarara University of Science and Technology, Uganda Florence Beinempaka |
Completed Extended Abstract published [14] Led to newborn cord care program changes |
|
| The impact of the VHT newborn strategy in reducing perinatal deaths in a rural district of Uganda | Makerere University, Uganda Isha Grant |
Funded, data collection complete Extended Abstract accepted for publication [15] Led to newborn cord care program changes |
|
| 2011 | Knowledge, attitudes and practices about blood donation in rural communities of Kiruhura District, South Western Uganda | Mbarara University of Science and Technology, Uganda Natukunda Peace |
Funded, data collection underway |
| Pilot project: impact of in-service training of midwives on partogram use | University of Nairobi Jennifer Oyieke |
Funded, intervention study underway | |
| 2012 | Use of mobile phones to improve the antenatal care attendance of pregnant women in semi-urban south eastern Tanzania | Tanzanian Training Centre for International Health, Tanzania Zabron Abel |
Funded, project started |
| Determinants of maternal health utilization by adolescents in informal settlements in Nairobi | University of Nairobi Fred Mochache |
Funded, project started | |
| Assessing tools, knowledge and practices of the health providers at the antenatal clinic in optimizing maternal health services in Kilombero District | Tanzanian Training Centre for International Health, Tanzania Boniphace Jullu |
Fundable – in revision phase | |
| Reasons for and determinants of non-adherence to the UNEPI vaccination schedule among children in Kyabugimbi sub-country in Uganda | Mbarara University of Science and Technology, Uganda Barnabas Atwiine |
Fundable – in revision phase |
Twelve examples of MicroResearch projects.
With respect to the impact of completed MicroResearch projects, 6 of 7 (83%) have had observable outcomes. The first funded project (2008), on immunization gaps, led to changes in village health team training in South West Uganda [10]. A study on glutamine supplementation for persistent diarrhea showed that this was ineffective in the East African setting [11] and should not be promoted as a local intervention. A study of women 15–45 years old in rural Uganda revealed gaps in knowledge about prevention of mother to child transmission of HIV and highlighted the need for different education strategies [12]. Following the publication of the extended abstract, the questionnaire was requested by an American team for adaptation for use in another African country. Findings from a study of knowledge gaps and retention factors for volunteer village health teams in South West Uganda [13] stimulated further local discussions and changes in support of village health team retention. Two Ugandan teams from different sites discovered congruence in their research findings at the 2nd MicroResearch Forum. One had assessed negative aspects of traditional birthing customs in the south–west region [14] while the other had found cord-related sepsis as a major cause of neonatal deaths in villages in a central rural district [15]. Following the 2nd Forum, together the two MicroResearch team leaders presented their findings to the Ministry of Health in Uganda. The Ministry then proposed a new neonatal chlorhexidine cord care program to be delivered in villages. Beyond policy and practice outcomes, completion and/or publication of the MicroResearch study findings, at least five successful MicroResearchers went on to career development or advancement based upon their work.
From the onset, local site East African faculty members were involved in teaching two modules in the workshops – ethics of research and community engagement. Over time, local faculty took on larger roles. At Mbarara University of Science and Technology the 2012 and 2013 workshops were delivered entirely by local faculty with the support from a Canadian trainer/observer.
Feedback from workshop participants over the five years was positive with over 90% rating their MicroResearch workshop experience as a 5 out of 5 and over 90% stating they would strongly recommend it to colleagues. In spontaneous comments, about 1 in 5 participants in any given year noted that MicroResearch would change their usual activity, e.g. their teaching, clinical work, goals, etc. (www.microresearch.ca/workshops). Participants commented that they were now capable of being more than just a supplier of research patients and/or a research data collector for studies designed and executed by external researchers from overseas. As one 2012 participant noted: “We now have the courage to develop our own proposals and submit them elsewhere.” Another noted that “….MicroResearch provides the forum for ordinary individuals to work to nurture relevant novel ideas with big [potential] impact on population health.”
Twenty-six and 27 participants from the 5 sites were invited to the MicroResearch Forums to discuss research projects either completed, under way or in development. Much interest in new research ideas and in sharing of protocols and potential collaborations was generated. At the 1st Forum, to facilitate further discussions, one participant developed an online closed LinkedIn network for MicroResearchers that has been well-subscribed to and at all 5 sites. The online survey (response rate 63% [43/68]) results were also presented at the 1st Forum. The top three East Africa health challenges identified were: (1) access to care, (2) social determinants and poverty; (3) health service and infrastructure gaps. The top three research challenges reported were: (1) capacity-building gaps (lack of mentors, and clear career paths); (2) research skills and knowledge gaps; (3) lack of access to research funding. In response to the survey and Forum discussions, the MicroResearch site leaders at the 1st Forum formed an East Africa MicroResearch Leaders Consortium aiming to enhance support for MicroResearch as it addresses the top three research gaps, e.g. “several small projects are effective and are sustainable”; “small projects are the cornerstone on which research skills are built and wider spectrum of potential of researchers are reached with excellent outcomes” [8]. The 1st Forum learning session on abstract writing was such a success that this became part of subsequent workshops. Following the 2nd Forum, a MicroResearch alumni directory program was developed and knowledge translation collaboration was formed between the two Ugandan teams working on cord sepsis as noted above. Two other teams, each from a different country, working on ways to increase prenatal visits, also discussed joining forces in knowledge translation in the future. The 2nd Forum learning exercise on knowledge translation was recommended to be included in the workshops. The Forum evaluations were positive with participants highly valuing the opportunity to meet other East Africa MicroResearchers with similar research interests. Many commented that such local opportunities for sharing were rare.
Beyond local site support for MicroResearch workshops and projects, as of 2013, three of the five sites had formally incorporated MicroResearch principles into their undergraduate healthcare education programs. At Mbarara University of Science and Technology, small interdisciplinary teams of healthcare students in their senior year address a community-directed healthcare problem and write up a report that includes recommendations and a poster presentation. At the Tanzanian Training Centre for International Heath both senior medical students and senior associate medical officers in training at the St. Francis University form small teams to address community-directed healthcare problems with report development and an oral presentation of their findings. At the Kenyan Medical Training College, where a number of faculties have received training through the University of Nairobi MicroResearch workshops, several senior program leaders have incorporated MicroResearch principles into their course programs for training allied health professionals. Additionally, following the 2nd MicroResearch Forum, the College also pledged to help financially support successful MicroResearch teams where the project was led by one of their faculty and the proposal was relevant to the College.
4. Discussion
The main goal of MicroResearch was to determine if this program would help build the capacity of local healthcare professionals in East Africa to find sustainable solutions for local community-focused health problems that then influenced government policy and/or local practice. MicroResearch success required strong local uptake; research proposals to be developed, funded and implemented; then research findings to be locally relevant and translated into action.
At five years, MicroResearch has been well accepted in the five participating East Africa sites. The MicroResearch experience was that front-line healthcare workers readily saw problems that needed urgent attention; were keen to address the problems when given the research skills, coaching and small grant support; and then worked to translate the findings into health policy, program and/or practice changes. Of the research outlines developed by the interdisciplinary MicroResearch teams during the training workshops in the first 4 years, 75% went on to be submitted, and of these 91% were sufficiently scientifically credible to be accepted and funded by MicroResearch. Gender equity was seen in the leadership of these successful MicroResearch teams. 6 of 7 completed projects had observable practice or policy outcomes. Participating in the MicroResearch program also supported career advancement. The joining up of MicroResearch teams from different sites/countries to develop collaborative knowledge translation strategies when their projects were synergistic was unanticipated. The MicroResearch Forums appear to have provided important opportunities to nurture collaborative research relationships.
Similar to the experiences of microfinance participants, MicroResearch graduates demonstrated a sense of independence and empowerment. At least eight went on to develop and garner funding for further research projects independent of MicroResearch. They no longer see themselves simply as suppliers of research patients or as research data collectors, but rather as researchers with important questions to ask and the skills to answer them. Like the wide range of microfinance products, the range of MicroResearch questions tackled has been broad [16]. Given the past history of research in these locales, external donor-initiated research would be unlikely to ever cover this diversity of maternal child health community-directed research.
A formal external auditing and evaluation program for MicroResearch is needed to document its successes and failures. Potentially this would also provide a better understanding of prerequisites for site and MicroResearch team success. These evaluations were not done due to lack of funding, as well over 90% of all monies in grants and donations have gone to support workshop training and the small MicroResearch grants. However, even with the lack of formal evaluation, the high workshop attendance rates, the positive workshop evaluations, the high rate of proposal outline to full successful grant application, the follow through on knowledge translation and the stimulation of research project development beyond MicroResearch suggest that MicroResearch is valued locally at the 5 sites in East Africa and that capacity for community-directed health research is growing locally.
To ensure that the local MicroResearch sites continue to thrive in East Africa, more funding support and more highly qualified local and international teachers, reviewers and coaches are needed to ensure program quality. The problems seen with too rapid early expansion of microfinance must be avoided. Like microfinance, MicroResearch requires close interaction and contact with participants. More resources are needed locally. The East African MicroResearch Leaders Consortium will be the key to find qualified local expertise to support the MicroResearch training and to finding local funding for projects. Development of partnerships by local MicroResearch with local nongovernmental organizations and government agencies may be a way forward. Links to nongovernmental organizations might also provide more knowledge translation avenues for change in practice, too. For governments, supporting local MicroResearch programs would well fit with the Bamako “call to action.” To further enhance local MicroResearch, further opportunities for more analytic, writing and knowledge translation skills development for graduates are needed. Expansion of the MicroResearch educational online modules or other tools and access to more advanced training opportunities for some would be helpful. The latter might be developed through links to more sophisticated research training programs offered in the region, such as the Consortium for Advanced Research Training in Africa (CARTA) [17].
In summary, at 5 years, MicroResearch has successfully started to grow capacity for community-directed research in East Africa. As one East African MicroResearch leader noted: “MicroResearch teaches us how to fish, shows us where to fish, then puts fish in the lake so we are sure to catch some”……. “We can make a difference in the health of our own communities through MicroResearch.”
Conflict of interest
There is no conflict of interest to declare.
Acknowledgements
MicroResearch has received funding from the International Development Research Centre of Canada; Dalhousie Medical Research Foundation, Halifax, Canada; Canadian Child Health Clinician Scientists Program, Toronto, Canada, and private donations via www.microresearch.ca plus in-kind donations and support from Dalhousie University, Halifax, Canada; IWK Health Centre, Halifax, Canada, Canadian Paediatric Society, Ottawa, Canada; Mbarara University of Science and Technology, Mbarara, Uganda; Healthy Child Uganda, Mbarara, Uganda; Makerere University, Kampala, Uganda; University of Nairobi, Nairobi, Kenya; Tanzanian Training Centre for International Health, Ifakara, Tanzania and Aga Khan University, Nairobi, Kenya.
References
Cite this article
TY - JOUR AU - N.E. MacDonald AU - R. Bortolussi AU - J. Kabakyenga AU - S. Pemba AU - B. Estambale AU - K.H.M. Kollmann AU - R. Odoi Adome AU - M. Appleton PY - 2014 DA - 2014/02/21 TI - MicroResearch: Finding sustainable local health solutions in East Africa through small local research studies JO - Journal of Epidemiology and Global Health SP - 185 EP - 193 VL - 4 IS - 3 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2014.01.002 DO - 10.1016/j.jegh.2014.01.002 ID - MacDonald2014 ER -
