Chikungunya outbreak in Al-Hudaydah, Yemen, 2011: Epidemiological characterization and key lessons learned for early detection and control
World Health Organization.
- DOI
- 10.1016/j.jegh.2014.01.004How to use a DOI?
- Keywords
- Chikungunya; Dengue; Al Hudaydah
- Abstract
Little is known about the occurrence of chikungunya fever in the Eastern Mediterranean Region of the World Health Organization (WHO). In January 2011, the Ministry of Public Health and Population (MoPH&P) of Yemen reported to WHO an increasing number of “dengue-like” acute febrile illnesses of unknown origin from one of its coastal governorates. An epidemiological investigation was conducted in Al-Hudaydah governorate between 23 and 26 January 2011 by a joint team of WHO, the MoPH&P of Yemen and the U.S. Naval Medical Research Unit (NAMRU-3) in Cairo, Egypt. The investigation led to the detection of an outbreak of chikungunya in Yemen which was the first time ever from any of the 22 countries in the Eastern Mediterranean Region of WHO. Appropriate public health control measures were strengthened following the investigation, and the outbreak was contained. This paper provides a short description of the outbreak and its epidemiological characteristics and highlights the important lessons that were learned for early detection and control of chikungunya in countries where competent vectors for transmission of the virus exist.
- Copyright
- © 2014 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Introduction
Chikungunya is a viral disease which was first reported in humans in Tanzania in 1952–1953 [1]. The disease is caused by chikungunya virus (CHIKV), which is an arbovirus of the genus Alphavirus (Togaviridae). The disease has been widely reported from many tropical countries in Africa and Asia in the past decades [2] causing widespread epidemics with significant public health problems [3]. The CHIKV is primarily transmitted to humans by the bite of infected Aedes species of mosquitoes. Since late 2004, CHIKV caused several major outbreaks globally that first spread from Kenya in Eastern Africa to South-Asia, including to the Indian Ocean islands in 2005–2006 [4]. The outbreak reported from the Indian Ocean island of Reunion notably infected one third of its estimated 770,000 inhabitants [5]. The disease is almost self-limiting and rarely fatal [5].
1.1. Situation in the Eastern Mediterranean Region
Outbreaks of chikungunya have not been reported from any of the 22 countries of the Eastern Mediterranean Region (EMR) of World Health Organization (WHO) in the past. Although dengue virus (DENV) and CHIKV share the same vector for transmission and dengue fever is indigenous in many countries of the WHO Eastern Mediterranean region causing geographically wide-ranging epidemics in the past [6], the evidence for the presence of CHIKV from the region came fortuitously through serological surveys conducted in Pakistan in 1983 [3] and from Sudan in 2005 [7]. Since 2004, Yemen has reported several dengue fever outbreaks [6], but chikungunya was never reported from the country. The first outbreak of chikungunya in Yemen was identified following a field investigation conducted at Al-Hudaydah governorate. This paper documents the epidemiological characteristics of this outbreak and highlights important lessons learned for early detection and control of chikungunya in countries where competent vectors for transmission of the virus exist.
2. Context and objectives
In January 2011, WHO was notified by the Ministry of Public Health and Population (MoPH&P) of Yemen of a suspected outbreak of “dengue-like” acute febrile illness of unknown origin from Al-Hudaydah governorate. Cases were reported from 20 of the 26 districts of the governorate, and the illness was characterized by acute onset of fever with severe incapacitating illness accompanied by arthralgia, skin rash and headache. According to the MoPH&P sources, some serum samples collected from the initial patients had been tested negative for DENV by serological test done at its Central Public Health Laboratory (CPHL) in Sana’a, Yemen. As cases continued to rise, the MoPH&P requested WHO’s support for conducting a field investigation in order to determine the cause of this outbreak and recommend appropriate public health control measures. In response to the request, an investigation was conducted in some of the districts of Al-Hudaydah governorate where recent cases were reported.
3. Methods
3.1. Investigation team and timing
The investigation team was comprised of members of the MoPH&P/Yemen, WHO Eastern Mediterranean Regional Office and the U.S. Naval Medical Research Unit No. 3 (NAMRU-3) based in Cairo, Egypt. The team was joined by staff members from the WHO Country Office in Yemen, as well as from the National Malaria Control Programme of MoPH&P/Yemen. The field investigation was carried out during the period 23–26 January 2011, and epidemiological, entomological and laboratory data were collected to determine the cause of this outbreak.
3.2. Investigation settings
The field investigation was carried out at Al-Hudaydah city, which is comprised of three districts – Al-Maina’a, Al-Hali and Al-Hawak – as well as in Al-Khawkha and Al-Munirah districts of Al-Hudaydah governorate where the most recent cases were reported. Al-Hudaydah governorate is the 4th largest governorate of Yemen covering an area of 13,250 km2 and with an estimated population of 2.5 million [8]. The governorate has more than 400 km of coast along the Red Sea (Fig. 1). Its capital city is comprised of three districts – Al-Maina’a, Al-Hali and Al-Hawak – with an estimated population of 488,772 which is an important port city of the country for the export of coffee, cotton, dates and hides and is also considered a crossing point for many migrant populations coming from abroad. The city is also a favorite stopover for domestic tourists owing to its long coast, climate, administrative and business centers and markets. The governorate is subdivided into 26 districts. The topography of the governorate includes coastal plains, fertile wadis (valleys) and islands scattered around the Red Sea, as well as hot springs. The climate of the governorate is semi-equatorial, warm and humid in the summer and moderate in the winter. The highest temperature reaches 40 °C during the summer and the highest temperature in winter may reach up to 24 °C. The governorate was the epidemic foci for several vector-borne outbreaks in the past, e.g. Rift Valley Fever in 2000 [9], malaria in 2004 and dengue fever in 2005 [MoPH&P Yemen, personal communication].
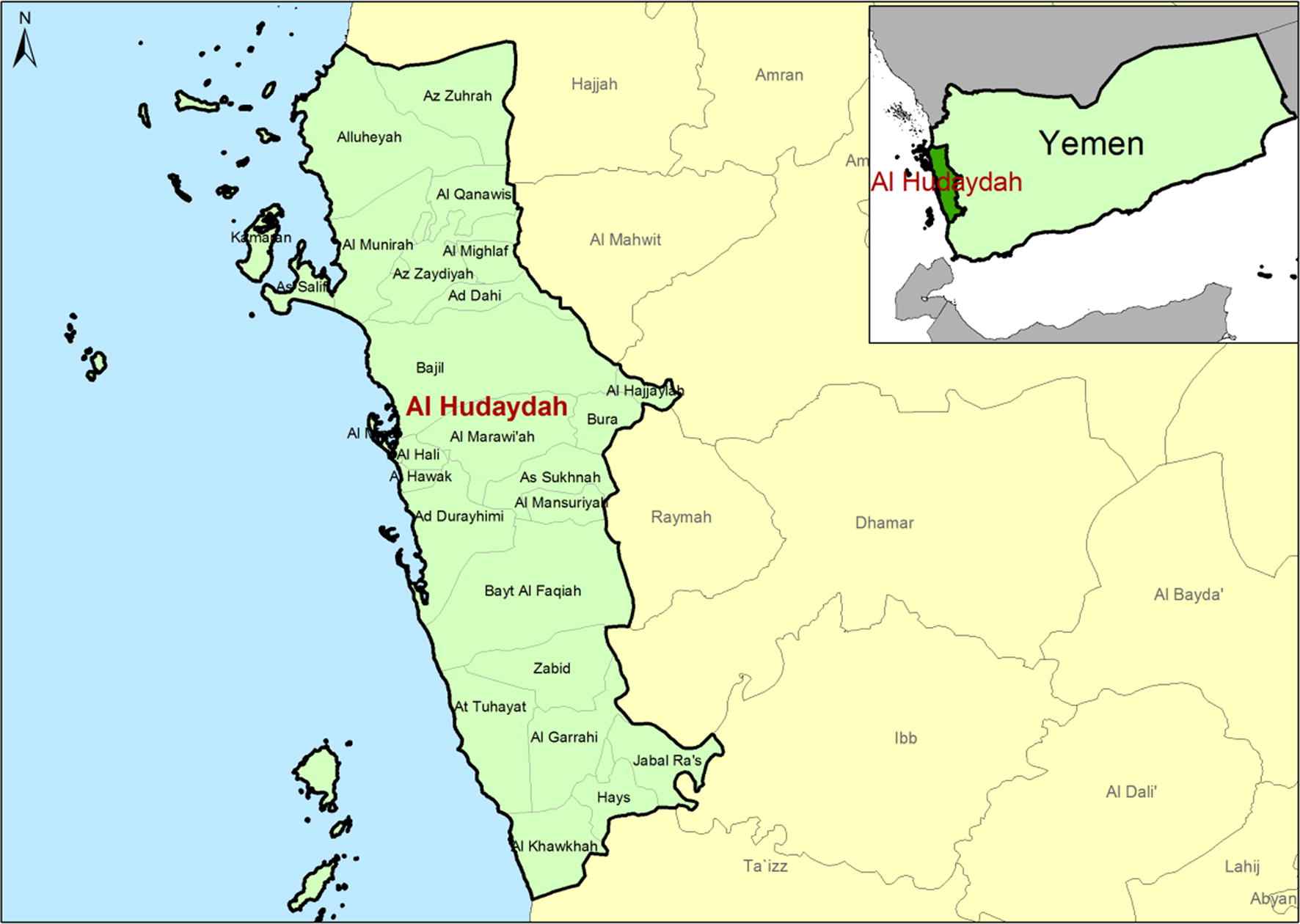
Al Hudaydah governorate in Yemen.
3.3. Epidemiological data collection
The team reviewed the hospital records of patients presenting with “dengue-like” acute febrile illness of unknown origin since the first week of October 2010 that were reported from a number of primary and secondary health care centers in the districts where the investigation was conducted. In addition, the team visited the households where recent cases were reported, examined the cases and interviewed the patients and their family members. A chikungunya fever was considered a possibility as almost all cases presented with similar clinical features, such as acute onset of fever with severe joint pains in a particular time interval. It was also revealed following interviews with the patients that all cases had a common history of mosquito bites. Following such case review, a working definition for chikungunya was developed for the purpose of collecting epidemiological data as any person with acute onset of fever >38.5 °C characterized by at least one of the following additional signs or symptoms: headache, severe joint pain, body aches and skin rash which could not be explained by any other medical condition and that were reported from any of the 20 districts of the governorate since the beginning of October 2010.
All cases that met the working case definition were included in a line-list. Descriptive epidemiological and clinical data of cases were collected retrospectively and included in the line list from all primary and secondary level public health facilities of the districts in the governorate that reported cases of “dengue-like” acute febrile illness of unknown origin until the time the field investigation was conducted.
3.4. Entomological data collection
The entomology team of the National Malaria Control Program of the MoPH&P and U.S.NAMRU-3 visited the houses of recently reported cases in two districts of the governorate: Al Khawkhah and Al-Munirah. Adult mosquitoes were collected indoors from 6 to 11 a.m. using a chargeable insect vacuum (Bioquip), BG traps baited with the non-toxic skin lure (Biogent) and knock-down pyrethroid spray. Larval indices were monitored in all possible containers per house or per inhabited premises. The Breteau and Container Indices were calculated. Later on, the viral RNA was extracted from vectors and tested by rRT-PCR for DENV and CHIKV using established procedures [10].
3.5. Laboratory data collection
Serum samples were collected during the field investigation from acutely ill patients presenting to health facilities with signs suggestive of dengue/chikungunya infection. Samples were initially screened at the CPHL in Yemen and then shipped to Cairo for further testing at the laboratory of U.S. NAMRU-3 (Cairo, Egypt). In addition, samples collected previously during the 42nd and 43rd epidemiological week, and also later, after the field investigation, during February–March 2011 were sent to U.S. NAMRU-3 for further testing. All samples were tested serologically using an in-house ELISA for chikungunya, yellow fever, Rift Valley fever and West Nile virus to detect IgM antibodies and by the commercial kit (Panbio, Australia) for dengue fever IgM. Samples were also tested for dengue IgG antibodies using Panbio commercial kit. Viral RNA was extracted from all samples using an extraction kit from Qiagen. The extracted RNA was tested by rt-RT-PCR for the four different dengue serotypes (1, 2, 3, 4) using a CDC protocol [11], and for yellow fever (YF) using published protocol [12]. Chikungunya virus samples with enough volume were also inoculated in Vero cells for virus isolation using established procedure as well [13]. Sequencing attempts were conducted following published procedures [14].
4. Data analysis
A line list which included information about demographic, epidemiological and clinical descriptive data of all suspected cases was reviewed by the investigation team and checked for consistency prior to analysis. Data were entered into Microsoft excel, and a descriptive analysis was conducted. The population projections for the affected districts were obtained from the census and used to compare disease attack rates by age-groups as well as by districts. Epidemic curves were drawn using the dates of onset of suspected cases to determine outbreak trends.
5. Result
5.1. Epidemiological and clinical description of cases
By the time the field investigation was concluded, a total of 10,715 suspected cases of chikungunya were reported from the Al-Hudaydah governorate between 1 October 2010 and 01 February 2011 signifying an outbreak for the first time ever in the country. The outbreak spanned over a period of 28 weeks, and by the end of April 2011, over 15,000 suspected cases of chikungunya were believed to have occurred in this outbreak. The suspected cases were first reported sporadically in early October from a few health centers in the Bayt Al Faqiah district. In the subsequent weeks, there was a gradual increase in the number of reported cases, also from the nearby districts. The outbreak had two peaks (Fig. 2). The first peak was observed during the third and fourth week of October 2010 corresponding to the 42nd and 43rd epidemiological weeks, respectively. The second peak was observed during the last week of February and the first week of March 2011 corresponding to the epidemiological weeks 8 and 9 of 2011, respectively. By the end of February 2011, all the 26 districts in the governorate reported suspected cases. There were also some mixed co-infections of dengue fever, including 104 deaths which were mostly reported during the second peak of this outbreak (MoPH&P Yemen, personal communication).
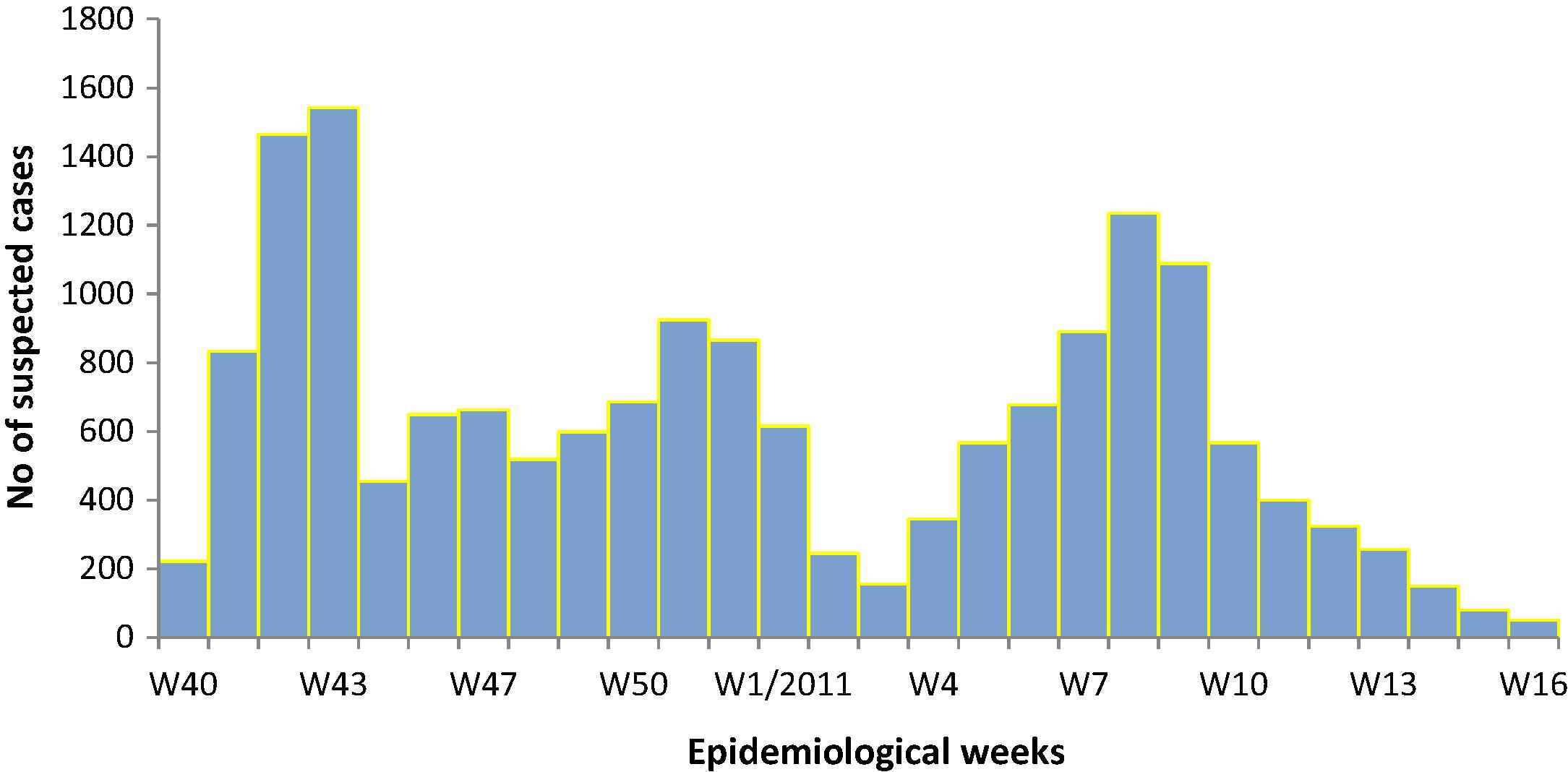
Epidemic curve for reported chikungunya/dengue fever in Al-Hudaydah governorate, Republic of Yemen, 01 October 2010 to 30 April 2011.
Males (52.9%) accounted for the majority of cases, while most cases (over 58%) were reported in the below-25-years-of-age group (Table 1). While the 15–25 year age group (27.1%) was the most at-risk age group for cases, the majority of deaths occurred in the over-40 years old age group.
| Characteristics | n (%) |
|---|---|
| Total reported cases | 10, 715 |
| Deaths | 0 |
| Sex | |
| Male | 5668 (52.9%) |
| Female | 5047 (47.1% |
| Age (Years) | |
| 0–4 | 867(8.1%) |
| 5–14 | 2507 (23.4%) |
| 15–25 | 2903 (27.1%) |
| 25–35 | 1071 (10%) |
| 35–45 | 1167 (10.9%) |
| ⩾45 | 2200 (20.5%) |
| Clinical features | |
| Fever (temperature, >38.5 °C)Fever | 10 715 (100%) |
| Arthalgia | 10,500 (98%) |
| Myalgia | 10,286 (96%) |
| Vomiting | 9964 (93%) |
| Retro-orbital pain | 9536 (89%) |
| Skin rash | 7714 (72%) |
| Headache | 5464 (51%) |
Demographic and clinical characteristics of suspected chikungunya fever cases reported from Al Hudaydah governorate of Yemen between 01 October and 01 February 2011.
While all cases presented with fever (100%), the other most common clinical presentations reported in this outbreak were arthralgia (98%), myalgia (96%) and vomiting (93%). About 89% of cases exhibited retro-orbital pain, while skin rash was present in 72% of cases. Just over half of the cases (51%) had headache.
The overall attack rate (cases per 1000 population) for chikungunya in the 20 districts where the cases were reported up until the time of investigation was 7 per 1000 with a range of 1 to 24 per 1000 cases (Table 2).
| Districts | Date of first reported case | Cases | Population | Attack rate (cases/1000) |
|---|---|---|---|---|
| Bayt-Al Faqih | 8-Oct-10 | 2532 | 284,341 | 9 |
| Zabid | 8-Oct-10 | 2188 | 182,072 | 12 |
| Al-Hudaydah city* | 8-Oct-10 | 822 | 488,772 | 2 |
| Al Mansuriyah | 22-Oct-10 | 100 | 52,102 | 2 |
| Az Zaydiyah | 29-Oct-10 | 663 | 112,231 | 6 |
| Al-Garrahi | 29-Oct-10 | 118 | 105,071 | 1 |
| At Tuhayat | 5-Nov-10 | 512 | 81,999 | 6 |
| Ad Durayhimi | 12-Nov-10 | 310 | 64,694 | 5 |
| Hays | 19-Nov-10 | 341 | 52,774 | 6 |
| Bajil | 26-Nov-10 | 645 | 202,727 | 3 |
| Al Marawi’ah | 3-Dec-10 | 269 | 151,806 | 2 |
| Al Munirah | 3-Dec-10 | 515 | 44,361 | 12 |
| Az Zuhrah | 10-Dec-10 | 851 | 161,933 | 5 |
| Al Qanawis | 10-Dec-10 | 313 | 84,565 | 4 |
| Al Khawkhah | 24-Dec-10 | 235 | 39,730 | 6 |
| As Salif | 31-Dec-10 | 179 | 7503 | 24 |
| Jabal Ra’s | 7-Jan-11 | 27 | 52,055 | 1 |
| Alluheyah | 15-Jan-11 | 95 | 122,468 | 1 |
| Total | 10,715 | 2,291,204 | 7 |
Al-Hudaydah city comprises of three districts- Al-Maina’a, Al-Hali and Al-Hawak.
Distribution of suspected case of chikungunya by district, Yemen, 2010–2011.
5.2. Entomological findings
A total of 30 adult mosquitoes belonging to Ae. aegypti and 17 to Culex spp. were collected. Larval densities/100 ml were 141 (STD = 48.8) and 93 (STD = 6.7), in Al Khawkhah and Al-Monirah districts, respectively. Samples of female Ae. aegypti collected from Al Khawkhah district yielded 40% positive pools (4 out of 10) for chikungunya, as indicated in the previous outbreak-related work [10]. The mosquitoes were infected as well as infectious as their mid-gut parts including the salivary glands were also CHIKV positive. Minimum and maximum infection rates of Ae. aegypti females were 20–72%, respectively. Apart from CHIKV, no other arboviruses (including RVF) were isolated from these samples. Ae. aegypti larvae were abundant in containers, and in a few containers they co-existed with larvae of Culex spp. Container indices were 66.7, 100 and 66.7 in Eritrean Camp site 1, site 3 of Al Khawkhah and Al Monirah district, respectively. The total container index of all sites was 53.8. The calculated Breteau index was 100 and the house index was 57.
5.3. Laboratory test results
Between October 2010 and March 2011, a total of 136 serum samples (including those collected during the field investigation) were tested at U.S.NAMRU-3. The samples were collected from Al Mounira, Zabeid, Al-Zaydela and Hays. The CHIKV and DENV reactive IgM antibodies were detected in 38 (28%) and 11 (8%) of the samples respectively. DENV IgG was positive in 119 (88%) of the samples. RT-PCR was positive in 55 (40%) and 4 (2.9%) of the samples for CHIKV or DENV-1 RNA, respectively. One sample was positive for both CHIKV and DENV-1 RNA. Samples from only 2 patients had positive PCR and IgG and negative IgM for Dengue and were therefore considered secondary Dengue infection. CHIKV was isolated from 27 (22%) samples. No DENV was isolated. Samples also tested negative by rt-RT-PCR for other flaviviruses. A high degree of similarity was identified between the Indian Ocean outbreak strains and the Italian, Indian, and Yemeni strains, with less than 1/100 substitutions per residue. A mutation generating a single amino acid change in the E1 gene of CHIKV was detected in the isolates from the outbreak. A detailed presentation of the patients’ results and the full virus sequence analysis will be presented elsewhere.
6. Discussion
This is the first documented outbreak of chikungunya ever reported from Yemen or any of the other 22 countries in the Eastern Mediterranean Region of WHO. The epicenter of this outbreak remains unknown, although purely circumstantial evidence backed up by available surveillance data suggest that cases were first reported during the first week of October 2010 from a semi-urban area of Bait-Al Faqih district before spreading to other nearby districts. The governorate experienced heavy rainfall and subsequent flooding in late July that year just after the dry season from June to mid-July. These flood water levels might have favored the hatching of Aedes eggs and subsequently provoked the vector development. This can probably explain the onset of this outbreak in October 2010. The presence of competent vector Ae. Aegypti in high densities following this record rainfall in the area possibly maintained the local transmission of CHIKV while intense human activities and continuous population movement between the districts helped its spread. The entomological findings of highly infected adult mosquitoes in rooms where recent cases were reported and the presence of breeding sources emphasized the risk of rapidly circulating CHIKV among the inhabitants. The late detection of the outbreak, almost 16 weeks after its onset, and ineffective vector control measures may have also contributed to the geographic spread of this outbreak. The delay in the detection of this outbreak may be attributed to several factors; apart from the lack of in-country laboratory diagnostic capacity for CHIKV, cases were also misdiagnosed as “dengue-like” as the area was a known endemic focus for dengue fever and many of the clinical symptoms of chikungunya resembled dengue fever. However, such overlap is not uncommon and may mask the clinical symptoms of chikungunya, particularly in dengue endemic countries as has been observed elsewhere [15,16]. It was observed during the field investigation that effective vector control measures for Aedes mosquitoes were lacking as the strategy of control measures was to target mainly the malaria vector breeding sites and therefore focused on space spraying only and that too only in outdoors. Given that Aedes mosquitoes are peri-domestic and have breeding sites close to human dwellings, often in backyards, reduction of mosquito breeding sites at the source was crucial to interrupt the transmission of virus circulation. Another observation was that the water scarcity in the outbreak area further compounded the problem of regular cleaning of potable water containers and discarding water off the infested ones at the household level. All these factors might have contributed to the sustained transmission of CHIKV during this outbreak.
After the laboratory confirmation of the outbreak in January 2011, effective vector control measures were instituted that might have resulted in the decline of the first wave of the outbreak. The co-circulation of both DENV-1 and CHIKV as seen particularly during the later part of the outbreak may possibly explain the second wave observed in the epidemic curve. There were 104 deaths reported from this outbreak among severe cases which were all reported during the second wave of the outbreak during the period February–March after the field investigation. The reasons for these deaths were unclear. Almost all these deaths preceded acute renal failures. Such a late surge in severe cases with impaired renal functions, as seen during the second wave of this outbreak in Yemen, was also reported from the chikungunya outbreak in Reunion Island [17]. Unexpectedly, there were also reports in the 2005–2006 outbreaks of deaths associated with CHIKV infection in Mauritius, India and also in Reunion Island [18–19]. It is not clear if the severe cases that mostly resulted in deaths were due to mixed CHIKV and secondary DENV infections as the percentage of severe cases found during the second wave of this outbreak coincided with the percentage of laboratory detection of mixed DENV/CHIKV infections. In the absence of other laboratory and clinical data, a direct causal link between these deaths and CHIKV infection could not be established. Although dengue virus was isolated, it did not account for the high severe presentations observed. Genotyping of the virus may help understand the severity observed in a number of cases.
The reported number of cases of chikungunya probably does not represent the true extent and magnitude of the outbreak as under diagnosis and underreporting were common. Due to the lack of active surveillance and active case detection, it is plausible that many suspected cases that preferred to be self-treated at home were missed out and not reported. This might explain the reason for a relatively low attack rate observed during this outbreak (7 cases per 1000) compared with what was seen elsewhere [15,16].
The clinical presentations of cases seen during this outbreak of chikungunya, such as fever, arthralgia, myalgia, skin rash and headache, were also commonly seen in other outbreaks [15,16]. Hemorrhagic manifestations were rare (0.4%), which were also generally uncommon in other outbreak episodes [3].
6.1. Limitations
One of the major limitations of this investigation was that compared with a number of cases reported, only a few cases could be laboratory-confirmed due to logistical reasons of collection and shipment of a large number of samples from Yemen to the U.S. NAMRU-3 laboratory in Egypt. The other limitation was the lack of full genome sequence data of the virus isolated from this outbreak to determine any similarity between the CHIKV strain isolated from Yemen and that with other outbreak episodes reported elsewhere. This could also explain if the virus was introduced to Yemen for the first time from outside. A detailed presentation of the patients’ results and the full virus sequence analysis will, however, be presented elsewhere.
7. Conclusion
The emergence of chikungunya in Yemen underscores the risk of the virus becoming established in the country owing to the presence of competent vectors. The risk of expansion of chikungunya to the neighboring countries of Yemen in the Red Sea rim is also high as these countries are dengue prone, cross-border population movement is rampant between these countries and competent vectors for transmission of CHIKV exist. The location of this outbreak in a coastal area of the country makes the spread of the disease a further possibility. Global evidence clearly shows that with the increase in international travel, the risk of spreading CHIKV to regions in which the virus is not endemic has increased [20].
Several lessons have been identified during this outbreak. The key strategy for improved outbreak prediction and detection for chikungunya in areas of high dengue and malaria endemicity should be to enhance routine sentinel-based surveillance systems for acute febrile illness, integrating both the epidemiological, entomological and laboratory surveillance components and routinely sharing the surveillance and other disease intelligence data between all departments within the Ministry and other agencies working in these hotspots. Any early sign of an impending outbreak, such as cluster of acute febrile illness, fortuitous isolation of epidemic arbovirus, or sudden high densities of competent vectors detected from any of these sentinel surveillance sites may trigger an appropriate investigation and rapid control. Such an early warning system may also allow the disease control programs to prepare for an appropriate pro-active response rather than waiting for cases to wait first and provide a reactive response.
An integrated vector control management should be considered for all dengue and malaria endemic countries for effective vector control. Vector control interventions should seek to reduce the potential breeding sites and as such should not wait until an outbreak occurs; rather they should be directed to keep the vector populations as low as practically possible throughout the year, particularly in its habitats. Effective household water management in water-unsecured areas and appropriate social communication to achieve the desired behavioral outcomes at the community and household level should also be linked to effective vector control measures both during an epidemic and the inter-epidemic period.
In all high dengue and malaria endemic areas, the use of a sensitive clinical algorithm for acute febrile illness may increase the precision of the clinical diagnosis of suspected chikungunya and other arboviral diseases early on and trigger appropriate investigation. This may be particularly helpful in areas where laboratory support is not readily available.
As for the current period, regional and international collaboration between all countries in the Red Sea rim and other agencies that are involved in outbreak detection, prevention and control efforts will be important in preventing and reducing the threat of chikungunya from being a major public health problem sweeping the region.
Competing interests
None declared.
Conflict of interest
None declared.
Acknowledgements
The authors thank Dr. Maria Morales and Iman Medhat from U.S.NAMRU-3, Cairo, Egypt for their assistance with testing diagnostic samples. The authors also acknowledge with appreciation the support received from Kira Christian from the Global Disease Detection Operations Center, Division of Global Disease Detection and Emergency Response, Center for Global Health, Centers for Disease Control and Prevention (Atlanta, USA), for facilitating the work between different departments. Dr. Guhlam Popal, the WHO Representative in Yemen and Dr. Mustafa Kamal, Technical Officer of WHO for Malaria Control Programme in Yemen provided valuable advice and guidance during the field investigation in Al-Hudaydah, Yemen.
References
Cite this article
TY - JOUR AU - Mamunur Rahman Malik AU - Abraham Mnzava AU - Emad Mohareb AU - Alia Zayed AU - Abdulhakeem Al Kohlani AU - Ahmed A.K. Thabet AU - Hassan El Bushra PY - 2014 DA - 2014/03/15 TI - Chikungunya outbreak in Al-Hudaydah, Yemen, 2011: Epidemiological characterization and key lessons learned for early detection and control JO - Journal of Epidemiology and Global Health SP - 203 EP - 211 VL - 4 IS - 3 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2014.01.004 DO - 10.1016/j.jegh.2014.01.004 ID - Malik2014 ER -
