The association between development assistance for health and malaria, HIV and tuberculosis mortality: A cross-national analysis
- DOI
- 10.1016/j.jegh.2014.10.001How to use a DOI?
- Keywords
- Development assistance for health; Aid; Health aid; Malaria; HIV/AIDS; Tuberculosis
- Abstract
Development assistance for health (DAH) and foreign aid have been criticized for being poorly associated with health and economic outcomes on a national level. This study is an attempt to examine whether DAH targeted specifically to malaria, HIV and tuberculosis (TB) is associated with changes in malaria, HIV and TB mortality, respectively. A dataset of DAH targeted to malaria, HIV and TB and corresponding malaria-, HIV- and TB-specific mortality was compiled for 120 low- and middle-income countries. Regression analysis was performed using country and time-period fixed effects and control variables. While malaria and HIV DAH were associated with reductions in malaria and HIV mortality, respectively, TB DAH was not significantly associated with reductions in TB mortality. Estimates were consistent in various sensitivity analyses, including generalized method of moments estimation, addition of extra controls and analysis of a multiply imputed dataset. In conclusion, targeted DAH is associated with reduction of HIV and malaria mortality on a national level.
- Copyright
- © 2014 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Introduction
The effect of foreign aid on population-level outcomes is controversial. Numerous aid projects have been demonstrated to have a positive effect at a micro-level in both the economic and health spheres. Interventions such as vitamin A supplementation, insecticide-treated nets and vaccinations have been shown to reduce mortality in randomized trials and are widely funded by foreign donors [1].
In contrast, macro-level studies on aid have been largely inconclusive. While a highly cited study concluded that aid could be effective at promoting the economic growth in the presence of good policies [2], recent analyses have found no relationship between aid and growth regardless of the presence of “good” policies [3]. Similarly, econometric studies that have attempted to identify whether development assistance for health (DAH) is associated with improvements in health outcomes have produced conflicting results. A cross-national analysis of health aid and overall mortality found that the provision of DAH to developing nations had no effect on population mortality [4]. An analysis of DAH provided to African nations for HIV control similarly found that the provision of targeted HIV aid had no significant spillover effects on overall mortality [5]. In contrast, a cross-national analysis of health aid and infant mortality found that increasing per capita health aid by $1.60 was associated with a 1.5 fewer infant deaths per thousand births [6]. Similarly, in a cross-national analysis of the association between health aid, and life expectancy and under-5 mortality, a 1% increase in health aid was associated with a 0.24 month greater increase in life expectancy and a 0.14 per 1000 live births faster decline in the probability of under-5 deaths per 1000 live births [7].
These inconclusive results contrast with modeling studies that find that donor-supported interventions improve health outcomes on an individual and regional level. DAH targeted toward malaria was found to have increased coverage rates of insecticide treated nets in Sub-Saharan Africa from 2003 to 2008 [8]. Similarly, an analysis of individual patient data found that individuals living within districts receiving large amounts of HIV assistance in Sub-Saharan Africa had lower mortality than individuals outside such districts [9].
There are a number of possible reasons for the discrepancy between the positive findings of individual and micro-level studies and the inconclusive findings of macro-level studies. One possibility is that DAH is fungible, and that the provision of DAH to developing nations does not lead to an increase in overall health spending [10]. Alternatively, the relationship between aid and improved outcomes may not be linked tightly enough for poorly powered macro-analyses to detect. While DAH may improve health outcomes on a macro-level, broad variation in health outcomes due to confounding factors and measurement error may prevent regression analyses from revealing a significant relationship. As a result, the ability of health aid to improve health outcomes may be falsely discounted.
This possibility was examined by using a cross-country regression analysis of development assistance for health targeted specifically to malaria, HIV and TB. It was hypothesized that the close linkage between targeted DAH and the overall mortality of its targeted disease would allow for a consistent association to be observed through fixed-effects regression analysis with various sensitivity analyses.
2. Methods
2.1. Data and definitions
In order to estimate the association of targeted DAH with specific health outcomes, comprehensive datasets for both DAH and health outcomes were aggregated. For DAH (disbursements), the Institute for Health Metrics and Evaluation (IHME) dataset from 1990 to 2010 was used [11]. This dataset aggregates DAH from multiple sources, including the Organization for Economic Cooperation and Development’s (OECD) aid database and databases of bilateral aid agencies. Additionally, the database separates DAH into that targeted toward malaria, HIV and TB. For malaria mortality, the IHME estimates from 1990 to 2010 were used [12], while for TB mortality, WHO estimates from 1990 to 2010 were used. For HIV mortality, estimates aggregated by UNAIDS and reported by the WHO from 1990 to 2010 were used [13]. To control for potential country-specific confounding factors, a governance index (the total of six World Bank governance indicators: control of corruption, rule of law, regulatory quality, political stability and absence of violence, voice and accountability and government effectiveness), total DAH disbursements, total population, population density, GDP per capita, proportion of population aged 0–14, proportion of population that is female, proportion of population living in a rural area, fertility, enrollment in a primary school, proportion of population with access to adequate sanitation, natural disasters, public health expenditures, out-of-pocket health expenditures, DTP immunizations and measles immunizations were included in the dataset [14,15]. Logarithmic transformations were used for disease mortality, DAH, GDP per capita, population, population density and total affected by natural disasters. Data sources are summarized in Supplementary Tables 1, 2 and 3.
Countries were included in the analysis if they had a population larger than 200,000 in 2010 and were classified as a low income, low-middle income or upper-middle income by the World Bank. Furthermore, this analysis includes only countries with time-series data on malaria, HIV and TB mortality that was at least 50% complete (Supplementary Table 2). The concern of selection bias arising from this criterion was addressed in a sensitivity analysis. As World Bank governance indicators and other cross-country data were only available after 1996, this analysis was from 1996 to 2010 (inclusive).
2.2. Model specification
To study the association between targeted development assistance for health and disease mortality, a longitudinal panel analysis was used. It is noted that an ordinary least squares regression may yield biased estimates because of determinants of mortality that are unobserved in this dataset. To reduce this source of bias, a country and time-period fixed-effects model was used to capture country-specific and time-period-specific characteristics that account for disease mortality. The following model was used for malaria mortality:
Similar models were used for HIV and TB. The dependent variable for all models was disease mortality (for malaria, HIV or TB) in time period t; the independent variables included DAH (malaria, HIV and TB all included) for time period t − 1 and controls for time period t. The lagged time period for DAH is consistent with the literature and was chosen on the assumption that a certain amount of time would be necessary to disburse DAH and therefore affect disease mortality. Additionally, a lagged independent variable is sequentially exogenous to disease mortality, reducing potential bias.
For all analyses, malaria, HIV and TB mortality per capita and DAH per capita were averaged over 3 year period in order to minimize year-to-year variation and reduce measurement error, as consistent with other cross-country analyses of foreign aid [2,3]. Logarithmic transformations of disease mortality, DAH, GDP, population, population density and lagged mortality were used to satisfy normality assumptions of regression. The main regression analysis was performed with the removal of outliers in development assistance for health, defined as the largest 1% of values. A summary of the data points used is provided (Table 1 ).
| Variables | (1) | (2) | (3) |
|---|---|---|---|
| log(Malaria mortality) | log(HIV mortality) | log(TB mortality) | |
| log(Lagged Malaria DAH per capita) | −0.257***(0.0804) | 0.0263 (0.139) | 0.0918 (0.104) |
| log(Lagged HIV DAH per capita) | −0.0623** (0.0289) | −0.245*** (0.0556) | −0.000971 (0.0365) |
| log(Lagged TB DAH per capita) | −0.0468 (0.120) | 0.218 (0.220) | −0.119 (0.144) |
| Governance1 | 0.00293 (0.00751) | −0.00153 (0.0152) | 0.00396 (0.0108) |
| log(GDP) | −0.0674 (0.0652) | 0.405*** (0.132) | −0.227** (0.0949) |
| log(Population) | 0.745 (1.193) | −1.988 (1.279) | 1.359 (0.998) |
| log(Population Density) | −1.289 (1.177) | 1.413 (1.403) | −1.581 (1.061) |
| log(Previous Mortality) (Lagged) | 0.779*** (0.0425) | 0.685*** (0.0367) | 0.624*** (0.0711) |
| Country fixed effects | Yes | Yes | Yes |
| Period fixed effects | Yes | Yes | Yes |
| Country-periods | 474 | 460 | 584 |
| R-squared | 0.998 | 0.99 | 0.988 |
| Number of countries | 99 | 94 | 120 |
Standard errors (in parentheses) are heteroskedasticity and autocorrelation robust, clustered by country.
Total of six World Bank governance indicators.
p < 0.05.
p < 0.01.
Country and time-period fixed effects regression analysis of disease mortality and targeted DAH with control variables and lagged mortality.
2.3. Sensitivity analyses
A series of sensitivity analyses were performed to test the robustness of the results. First, generalized method of moments (GMM) estimation was used to address the concern that the inclusion of a lagged dependent variable in a fixed-effects model yields biased estimates across all estimated coefficients. The issue arises because fixed-effects estimation requires demeaning at the country level, and the demeaned error term necessarily depends on the error terms from each time period; the lagged dependent variable is correlated with the lagged error term and thus not exogenous to the demeaned error term. GMM estimation relies on the weaker assumption of predetermination to estimate the effect using lagged variables as instruments. GMM’s instrumental-variable approach also addresses bias arising from time-varying, country-specific unobservables (i.e., those not captured by country and time-period fixed effects), as well as classical measurement error. Mishra and Newhouse implement a similar application of GMM estimation [7]. This system was used over first-difference GMM because of the persistent nature of the dependent variable [16,17].
Secondly, a series of extra controls (proportion of the population aged 0–14, proportion that is female, proportion living in rural areas, fertility rate, school enrollment, proportion of the population with access to adequate sanitation, log of population affected by a natural disaster, percentage of public expenditures on health, percentage of private expenditures on health, percentage of children aged 12–23 months with DPT immunization and percentage of children aged 12–23 months with measles immunization) were introduced into the model to address further concerns of omitted variable bias. Thirdly, total DAH disbursements were added to account for the investment in the health system infrastructure at large, as well as to assess the relative contribution of disease-specific DAH. Fourthly, the model was tested with the inclusion of the 1% outliers in DAH excluded in the main regression analysis. Fifthly, the time period under investigation was restricted to 2000–2010, as much of the early IHME DAH dataset is imputed [18]. Sixthly, potential selection bias arising from missing data was addressed using multiple imputation based on chained equations; ten imputed datasets were generated, fixed-effects regression was performed on each and estimates were pooled. Finally, to address the concern of bias resulting from the fact that modeled estimates of malaria, TB and HIV mortality indirectly rely upon DAH, further analyses were performed using an alternative set of outcome measures: reported malaria deaths (World Health Organization/World Malaria Report), reported TB cases (World Health Organization/Global Tuberculosis Report) and estimated HIV prevalence (UNAIDS/World Health Organization).
All analyses were performed using STATA version 12 (STATA Corp.).
3. Results
Within this sample of 120 low- to middle-income countries, DAH increased rapidly from 1990 to 2000. In 1991, DAH for HIV and malaria was less than $0.01 per capita and DAH was $0.013 per capita for TB (Fig. 1 ). By 2010, DAH targeted to malaria was $0.25 per capita, a more than 50-fold increase. These trends were paralleled in HIV and TB, with DAH for TB increasing to $0.11 per capita by 2010 and HIV DAH increasing to $0.88 (Fig. 1B and C). For all three diseases, mortality declined in the period from 2005 to 2010, over which the largest increase in DAH was observed. However, for both malaria and HIV, this decline in mortality followed a significant increase in mortality from 1990 to 2005 (Fig. 1A and C).
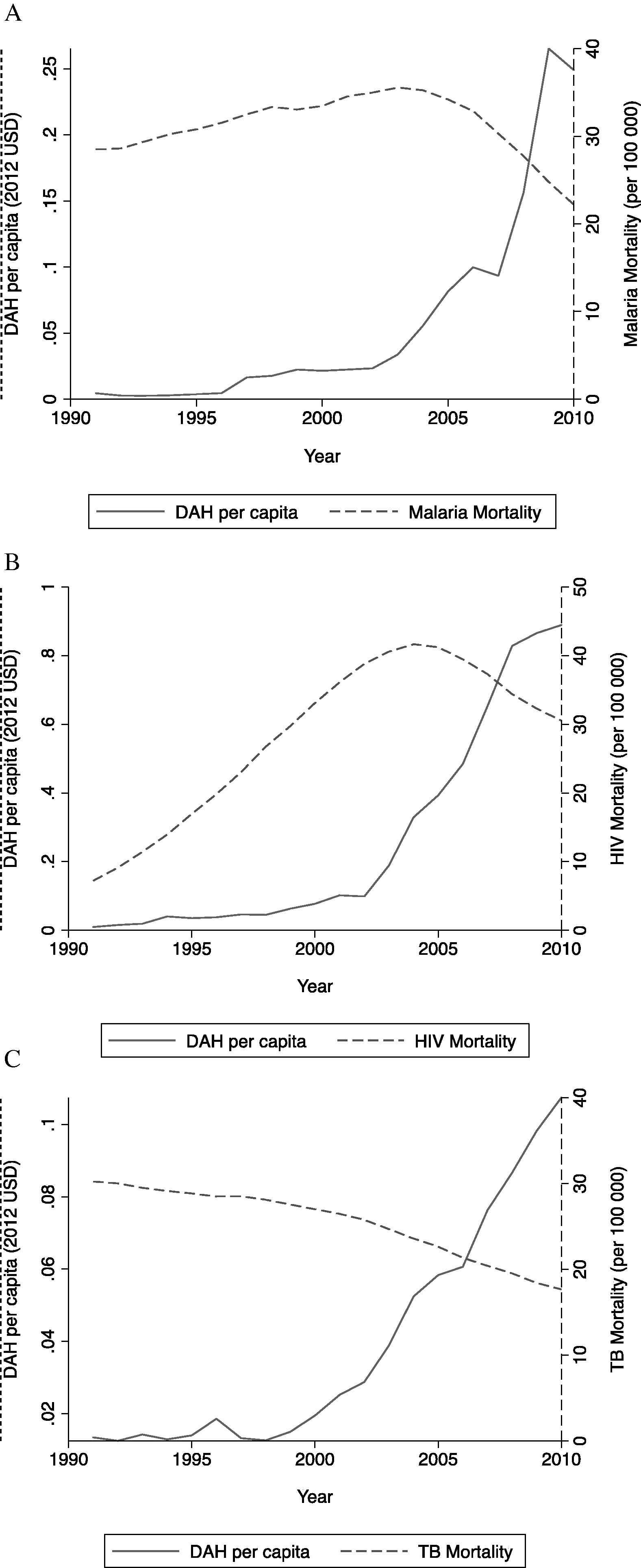
Development assistance for health (2005 $US per capita) and disease mortality (per 100,000 population) for (A) malaria, (B) HIV and (C) tuberculosis from 1990 to 2010.
In order to further examine the relationship between DAH and mortality, a country and time period fixed effects regression analysis was implemented.
3.1. Association between targeted DAH and disease mortality
It was examined whether or not DAH was associated with a decrease in mortality with country-level controls (governance, GDP, population and population density). For malaria mortality (column 1, Table 1), it was found that malaria DAH is highly predictive of a decrease in mortality (p = 0.002), while HIV DAH is significant but less strongly correlated, and tuberculosis DAH is insignificant. For HIV mortality (column 2, Table 1), only HIV DAH is predictive of a decrease in HIV mortality (p < 0.001). Conversely, TB DAH is not predictive of a decrease in TB mortality (p = 0.41). Thus, it appears that while malaria DAH and HIV DAH are associated with a decrease in malaria mortality and HIV mortality on a country level, TB DAH is not. A 50% increase in DAH targeted to malaria would be associated with a 9.9% (95% CI 4.0%, 15.5%) decrease in malaria mortality. A 50% increase in DAH targeted to HIV would be associated with a 9.5% (CI 5.4%, 13.4%) decrease in HIV mortality.
3.2. Sensitivity analyses
A series of sensitivity analyses were performed to test the robustness of the results. When GMM regression analysis was performed using two further lags of DAH and control variables, malaria DAH and HIV DAH were again associated with reductions in malaria and HIV mortality, respectively (Table 2). Specifically, one-period lagged malaria DAH was significantly associated, while three-period lagged HIV DAH was significant for HIV mortality (i.e., HIV DAH from 6 to 9 years prior). Although three-period lagged TB DAH was significant in this specification, this was not observed in further analyses.
| Variables | (1) | (2) | (3) |
|---|---|---|---|
| log(Malaria mortality) | log(HIV mortality) | log(TB mortality) | |
| log(One-period lagged DAH per capita) | −0.228** (0.111) | −0.0403 (0.0891) | −0.215 (0.236) |
| log(Two-period lagged DAH per capita) | 0.0799 (0.184) | 0.00476 (0.131) | 0.0286 (0.215) |
| log(Three-period lagged DAH per capita) | −0.0209 (0.134) | −0.259** (0.127) | −0.265** (0.129) |
| Hansen test(p-value) | 0.156 | 0.498 | 0.491 |
| Number of instruments | 67 | 67 | 67 |
| Number of countries | 97 | 93 | 119 |
| Number of observations | 285 | 279 | 352 |
Standard errors (in parentheses) are heteroskedasticity robust and finite-sample corrected.
p < 0.05.
Arellanno-Bond GMM regression analysis of disease mortality and targeted DAH. Model includes current, single-lagged and double-lagged log(GDP), governance, log(population) and log(population density) as control variables. DAH per capita refers to targeted DAH, i.e., malaria DAH for specification 1 and HIV DAH for specification 2.
When extra controls (proportion of the population aged 0–14, proportion that is female, proportion living in rural areas, fertility rate, school enrollment, proportion of the population with access to adequate sanitation, log of population affected by a natural disaster, public expenditure on healthcare, out-of-pocket expenditure on healthcare, DPT immunization and measles immunization) were introduced, malaria DAH and HIV DAH remained significantly associated with decreases in malaria and HIV mortality, respectively (Supplementary Table 4). Estimates were consistent when total DAH was introduced into the model as a covariate (Supplementary Table 5). Estimates were also consistent when outliers were included (Supplementary Table 6) and when the period of analysis was restricted to 2000–2010 (Supplementary Table 7). When multiple imputation using chained equations was used to impute missing data points, HIV and malaria DAH remained significantly negatively associated with HIV and malaria mortality (Supplementary Table 8). When reported malaria deaths, reported TB cases and estimated HIV prevalence were used in place of estimated mortality, malaria DAH and HIV DAH were associated with reduced reported malaria deaths and estimated HIV prevalence with the addition of extra controls (Supplementary Table 9). Malaria DAH was imprecisely estimated with reported deaths in the basic specification, but the estimated coefficient took the expected sign and was significant with extra controls. Throughout all specifications, TB DAH remained insignificant.
4. Discussion
These results illustrate that at the country level DAH targeted to malaria and HIV are associated with reductions in malaria and HIV mortality, respectively. These results are the first demonstration that targeted DAH on a national level that is associated with reduced disease mortality. These results contradict previous studies that found no evidence of a relationship between aggregate health aid and population-level mortality [4,5] and support an analysis by Mishra and Newhouse which demonstrated a significant association between DAH and decreased infant mortality [6]. It is acknowledged that the lack of an association between targeted aid and health outcomes is not implausible. A previous analysis found that for every $1 provided in the form of DAH, governments reduced their domestic health spending by $0.46 [10]. It is possible that nations that received targeted DAH reduced domestic spending on target diseases to such a degree that no improvement in health outcomes could be observed. However, these results indicate that, at least for HIV and malaria, this hypothesis is not supported.
Interestingly, the GMM estimates suggest that three-period lagged HIV DAH (i.e.,6–9 years prior to current HIV mortality) was significantly associated with decreased HIV mortality, while single-period lagged malaria DAH was associated with reduced malaria mortality. This is consistent with the known epidemiology of malaria and HIV. Unlike malaria, in which the increased uptake of insecticide treated nets and anti-malarials would immediately reduce mortality, changes in the incidence of HIV via greater uptake of antiretroviral therapy would lead to a delayed impact on HIV mortality (in addition to an immediate benefit from the treatment of the HIV-positive) [19].
However, unlike DAH for malaria and HIV, DAH for TB was not associated with reductions in TB mortality. One explanation is the proportion of domestic spending allocated to TB relative to international support. In 2011, 90% of spending on TB control in developing countries was provided by domestic sources [20]. By contrast, for HIV only 50% of spending in developing countries was provided by domestic sources, and only 36% in Africa [21]. Similarly, domestic malaria financing was estimated to make up only 25% of global funding for malaria control in 2010 [22]. Unlike the effects of malaria and HIV DAH on mortality, the effect of TB DAH on TB mortality would be heavily outweighed by changes in domestic spending on TB. In this way, the observed heterogeneity of the aid-mortality effect further supports the need to examine the data at the disease-specific level.
In spite of these positive findings, these results cannot be interpreted as having demonstrated causality between increased DAH and improvements in health outcomes. Although this study has demonstrated an association between malaria and HIV DAH and reductions in their respective mortality, a causal relationship is not the sole explanation. Another possibility is that DAH follows improvements in outcomes rather than the other way around. Although lagged DAH was utilized relative to mortality and GMM estimation in an attempt to address this possibility, lagged DAH may still be associated with past performance, which itself may be associated with future performance. A second potential source of bias is time-associated measurement error in DAH. If reporting of DAH systematically improved over time, the effect of measured DAH on mortality may be underestimated, as the observed increase in DAH over a given period would be an overestimate of the true increase in DAH. Finally, unobserved confounding and selection bias may also have impacted these results, although the GMM analysis represents a modest attempt to address these concerns as well.
In sum, unlike previous aid-growth studies that have found a negative association between aid and growth before the addition of controls and a non-significant relationship after the addition of controls [3], it was found that targeted DAH for malaria and HIV are associated with reductions in mortality (columns 1 and 2, Table 1) and that this effect is robust to a variety of sensitivity checks, including GMM estimation, expanded controls, and multiple imputations of missing data. It is also consistent with numerous case studies that have found that donor funding saves lives [1] and that the withdrawal of donor funding has led to the resurgence of disease [23].
In light of these findings, the global slowdown in DAH is concerning. While DAH grew at a rate of 17% from 2007 to 2008, this rate slowed to 4% from 2010 to 2011 (1% if loans are excluded). Since 2000, broad gains have been made in the fight against malaria, HIV and TB, as shown in Fig. 1 [24]. However, significant budgetary shortfalls exist for the control of all three diseases, a trend that will be exacerbated by both the slowdown in funding and the continuing increase in the prevalence of HIV. As these findings and a larger body of work suggest, development assistance for health may be associated with reductions in preventable mortality from infectious disease.
Ethical approval
No ethical approval was needed.
Funding
No funding was received for this study. AH and CE are supported by the Rhodes trust.
Conflict of interest
AH and CE have no conflicts of interest to declare.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jegh.2014.10.001.
References
Cite this article
TY - JOUR AU - Allan J. Hsiao AU - Connor A. Emdin PY - 2014 DA - 2014/11/10 TI - The association between development assistance for health and malaria, HIV and tuberculosis mortality: A cross-national analysis JO - Journal of Epidemiology and Global Health SP - 41 EP - 48 VL - 5 IS - 1 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2014.10.001 DO - 10.1016/j.jegh.2014.10.001 ID - Hsiao2014 ER -
