Rheumatoid Arthritis in the Lebanese Adults: Impact on Health-Related Quality of Life
- DOI
- 10.2991/jegh.k.190820.001How to use a DOI?
- Keywords
- Rheumatoid arthritis; quality of life; health-related quality of life; SF-36; Lebanese population
- Abstract
Rheumatoid Arthritis (RA) is a chronic inflammatory disabling disease with significant impact on the Quality of Life (QOL) of patients. Information on the effects of RA on Health-related Quality of Life (HRQoL) is lacking in the Lebanese population. The objective of this study was to evaluate QOL of RA patients compared with non-RA subjects and to suggest possible predictors of their QOL in Lebanon. We conducted a case–control observational study among individuals visiting the external clinics at three hospitals and different private clinics; the QOL was measured using the SF-36 questionnaire administered face to face to the study population, applied to RA (N = 90) and non-RA (N = 180) groups. RA presented lower Physical Component Scores (PCS) and Mental Component Scores (MCS) as well as overall QOL scores. Among RA patients, MCS and QOL were significantly decreased with morning stiffness duration (β = −9.211, p = 0.013 and β = −9.190, p = 0.009, respectively). The frequency of practicing sport per week increases PCS and QOL (β = 6.692, p = 0.002 and β = 6.148, p = 0.003, respectively). Workability has a positive effect on PCS (β = 5.546, p = 0.022) and time between blood transfusion and the onset of the disease has a positive impact on MCS (β = 8.415, p = 0.007). To improve QOL of patients with RA, health professionals have to take these results into consideration while treating their patients.
- Copyright
- © 2019 Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Rheumatoid arthritis (RA) is a chronic inflammatory autoimmune disease characterized by pain, stiffness, swelling, and tenderness of synovial joints [1]. There is an estimated prevalence of RA in the world population from 0.5 to 1%, with mean annual incidence of 0.02–0.05%. Women are more likely to develop RA than men [2]. Predominance is two to three times higher in females, whose peak is observed around the age of 50 years [3]. Being overweight increases the risk of RA for women but actually decreases the risk for men [2]. Prolonged smoking has a role in increasing the concentration of rheumatoid factor, “which is an antibody”. Moderate consumption of alcohol does not seem to increase women’s risk and may even lower it. In addition, specific diet rich in antioxidants and poor in red meat and sugars may decrease the risk of RA [4].
According to the World Health Organization (WHO), quality of life (QOL) is defined as “the individuals’ perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” [5]. Ever since this definition was given by the WHO in 1948, there has been a major emphasis on the impact of diseases on the QOL of patients [5]. Health-related quality of life (HRQoL) refers to the extent to which patient’s usual or expected physical, emotional, and social well-being are influenced by their medical condition and/or by the treatment they receive [3,6,7]. QOL is a concept increasingly used in the assessment of health care outcome of a given population (diet habits, housing, employment, recreation, and so on) and of the impact of therapeutic applications associated with different groups of diseases [3]. Historically, the impact of chronic diseases on the patients’ lives has been defined in terms of three different levels stated by the WHO: impairment, disability, and handicap [8]. As other chronic diseases, RA is a chronic inflammatory disabling disease with significant impact on the QOL of patients [5,9]. Although RA primarily affects the joints and leads to physical impairment, many patients with RA also experience psychological effects such as: depression, anxiety, feelings of helplessness, low self-esteem, loss of energy, and fatigue [1,2,8,10]. Pain and stiffness can last for more than 30 min in the morning or after a long period of rest. Higher pain levels in patients with RA have been shown to correlate with disability as well as depression, which all contribute significantly to a reduction in QOL [2,8]. Besides, permanent work disability and instability are common among patients with RA and have a significant impact on patients’ financial and social well-being that may lead to QOL deterioration [6,11,12].
For the Lebanese population, the prevalence of rheumatic diseases was found to be about 15% by Chaaya et al. [6]. Nevertheless, no study has been previously conducted regarding the HRQoL of RA patients and its significance in the Lebanese population. As “adding years to life is an empty victory without adding life to years” as WHO states [13], the objective of this study was to evaluate QOL of RA patients compared with non-RA patients in Lebanon and to suggest possible predictors of QOL in the two groups.
2. MATERIALS AND METHODS
2.1. Study Design
This is an observational case–control study carried out in RA patients undergoing treatment and non-RA patients. A convenient sample of patients was randomly selected from those visiting external clinics at three hospitals (AL Rasool Hospital, Bahman Hospital, and Saint George Hospital), and patients visiting rheumatologists’ private clinics in Beirut, Lebanon. Cases and controls were recruited based on the presence or absence of RA as a diagnosis in their medical files.
The scheme of this study maintains the total anonymity of the patients and does not violate human rights. Even though it was not an interventional study and therefore did not require any definite ethical approval, however, verbal consent was obtained from all participants before administering the questionnaire, which was completed in the waiting room before the clinical assessment. An approval was taken from the Institutional Review Board to carry out the study at each hospital as well as from each doctor to carry out the study at his/her clinic. The patients were informed about the objective of the study and asked to provide an oral consent before they started with the procedure. Data were collected from August until the end of September 2017.
2.2. Study Population
All outpatients aged 32–60 years of both genders with confirmed RA disease duration of 1–20 years were recruited as cases. The diagnosis had to be confirmed by a clinical rheumatologist. Patients who did not have any official confirmation of RA, heavily handicapped patients, patients with language limitations (who did not speak Arabic or English), non-Lebanese patients, pregnant women, patients who did not provide verbal consent, as well as patients suffering from neurological problems were all excluded from the study.
Controls were selected by simple random sampling from the patients aged 32–60 years of both genders who were visiting outpatient clinics situated close to rheumatology clinic at the same study period: patients attending clinics of respiratory, endocrinology, urology, cancer, pre-surgery consultation, and gastroenterology. For every case included in the study up to two controls were recruited.
2.3. Data Collection
Data were acquired through a structured face-to-face interview. The questionnaire was administered in Arabic, the main language in Lebanon, and included: sociodemographic characteristics of patients including sex, age, education level, marital status, monthly income, Body Mass Index (BMI), district of residence, employment and work demand (mental, physical, or both physical), work disability, and the source of insurance; life style data such as smoking, alcohol consumption, and physical exercise. Detailed health history was also included in relation with the onset of RA, the presence of associated complications and comorbidity (e.g., cardiovascular diseases, diabetes mellitus, psychological disorders, obstructive pulmonary disease, osteoporosis, and so on), and medication use.
2.4. QOL Measurement
The QOL of patients was assessed using an Arabic version of the SF-36 generic questionnaire as described by Sabbah et al. [7]. It consists of 36 questions that are distributed across eight scales: Physical Functioning (PF) (10 items), Role Physical (RP) limitation (four items), Bodily Pain (BP) (two items), General Health (GH) (five items), Vitality (VT) (four items), Social Functioning (SF) (two items), Role Emotional (RE) limitation (three items), and Mental Health (MH) (five items). From these eight scales, it is possible to calculate two summary scores, Physical Component Summary (PCS – physical functioning, role physical limitation, bodily pain, and general health), which takes into account all aspects of the physical daily activity or at work outside home, and Mental Component Summary (MCS – social functioning, role emotional limitation, RA mental health, and vitality), and the overall QOL. The answer for each question corresponds to a score as a percentage as stated by Hays et al. [9]. Data are presented as means; statistical significance was tested using t-test, all p-values <0.05 are statistically significant. Higher scores represent higher levels of functioning or well-being.
2.5. Sample Size
Sample size was calculated using Epi Info 7, assuming a type I error of 5%, study power of 80%, and confidence interval of 95%. Taking Lebanese RA prevalence as 14.3% [12], the result was 90 cases and 180 controls with cases/control ratio of 1/2. Hence, the total study population size was 270 participants. This minimal sample size was necessary to show a threefold increase in the risk for most of the associations with frequency of exposure about 0.6 in the control group.
2.6. Statistical Analysis
Data were entered and analyzed using Statistical Package for Social Sciences (SPSS, IBM,USA), version 21. No missing data were obtained. A p-value ≤0.05 was considered significant in all tests. Descriptive analysis was done first to evaluate the distribution of the sociodemographic characteristics of the patients, their life style behaviors, and their past medical history. The results are expressed in frequency and percentage [n (%)] for all the qualitative variables and in mean (±) Standard Deviation (SD) for quantitative variables. An appropriate bivariate analysis was done for every explanatory variable. For comparing continuous variables, we used Student’s t-test or one-way ANOVA for variables with adequate normal distribution to compare between mean. For non-normally distributed continuous variables, the Mann–Whitney U or Kruskal–Wallis test was used. For categorical variables, the Chi-square and Fisher exact tests were used to compare percentages.
Similarly, a multivariable analysis using linear regression was carried out to determine predictive factors affecting the QOL. The major dependent variables were PCS scores, MCS scores, and the overall QOL, which is the sum of all individual domains of SF-36 items (physical functioning, physical role limitation, pain, general health perception, vitality, social functioning, emotional role limitation, and mental health) in addition to one item to compare current health status and that of the previous year (perceived health change). The analysis sought to explore factors associated with general physical and mental health using regression analysis. However, the independent variables are all potential confounding variables that had p-value <0.2 in bivariate analysis including: sociodemographic, life style, adherence, patient health, and disease status. Conditions of normality, linearity, adequacy, and homoscedasticity for data were checked for the linear regressions using Hosmer and Lemeshow test.
3. RESULTS
Only 270 patients were solicited to fill the questionnaire. All patients agreed to participate in this study. Among them, 90 patients (33.3%) diagnosed with RA were included as cases and 180 patients (66.7%) who were not diagnosed with RA were included in the control group.
3.1. Sociodemographic Characteristics of the Study Population
The comparison of characteristic differences between RA and control groups is shown in Table 1. Female patients (62.2%) were significantly more affected by RA than male patients (37.8%, p = 0.025). Patients with RA were older than control group (p = 0.02). Significant difference was found between RA and control in the place of living (p < 0.001), such that most of the cases were found living in Beirut (77.8% versus 62.8% of the controls), 7.8% of the cases were living in Bekaa and 7.8% in South Lebanon, whereas it was 22.8% and 14.4% for the control group, respectively. Greater number of jobless participants were found in RA group (p = 0.031). There was no significant difference between RA and controls regarding marital status (p = 0.059), education level, monthly income, and the type of medical insurance (p > 0.05).
| Variables | RA* [n (%)] | Control [n (%)] | p-Value |
|---|---|---|---|
| Sex | 0.025 | ||
| Male | 34 (37.8) | 94 (52.2) | |
| Female | 56 (62.2) | 86 (47.8) | |
| Age | 0.020 | ||
| 24–35 | 23 (25.6) | 48 (26.7) | |
| 36–50 | 39 (43.3) | 47 (26.1) | |
| >50 | 28 (31.1) | 85 (47.2) | |
| District | <0.001 | ||
| Beirut | 70 (77.8) | 113 (62.8) | |
| Bekaa | 7 (7.8) | 41 (22.8) | |
| South | 7 (7.8) | 26 (14.4) | |
| North | 6 (6.7) | 0 (0) | |
| Marital status | 0.059 | ||
| Single | 17 (18.9) | 18 (10) | |
| Married | 64 (71.0) | 150 (83.3) | |
| Divorced | 9 (10) | 12 (6.7) | |
| Education level | 0.258 | ||
| Not educated | 16 (17.8) | 49 (27.2) | |
| Primary school | 32 (35.6) | 49 (27.2) | |
| Middle education | 19 (21.1) | 42 (23.3) | |
| High education | 23 (25.6) | 40 (22.2) | |
| Occupation | 0.031 | ||
| Jobless | 49 (54.4) | 74 (41.1) | |
| Employee | 33 (36.7) | 70 (38.9) | |
| Retired | 8 (8.9) | 36 (20) | |
| Work demand | 0.260 | ||
| No | 46 (51.1) | 108 (60) | |
| Mental | 10 (11.1) | 21 (11.7) | |
| Physical | 17 (18.9) | 32 (17.8) | |
| Mental + physical | 17 (18.9) | 19 (10.6) | |
| Work ability | 0.152 | ||
| No | 32 (35.6) | 59 (32.8) | |
| Fully | 20 (22.2) | 60 (33.3) | |
| Partially | 38 (42.2) | 61 (33.9) | |
| Income (LP/Month) | 0.080 | ||
| 0 | 48 (53.3) | 76 (42.2) | |
| <10,00,000 | 21 (23.3) | 38 (21.1) | |
| ≥10,00,000 | 21 (23.3) | 66 (36.7) | |
| Insurance | 0.157 | ||
| No | 29 (32.2) | 71 (39.4) | |
| Social security | 21 (23.3) | 27 (15) | |
| Cooperative staff | 6 (6.7) | 17 (9.4) | |
| Insurance | 6 (6.7) | 7 (3.9) | |
| Ministry of Public Health | 22 (24.4) | 34 (18.9) | |
| Military | 6 (6.7) | 24 (13.3) | |
| Total (N) | 90 (33.3) | 180 (66.7) |
RA, rheumatoid arthritis; [n (%)], frequencies (percentages). p < 0.05 is considered significant, 10,00,000 LP (Lebanese pound) ≃ 650 USD.
Rheumatoid arthritis and related sociodemographic variables
3.2. Behavioral Characteristics
Concerning lifestyle factors and habits (Table 2), a significant difference was found between RA and controls regarding smoking (p = 0.048) and alcohol consumption (p = 0.033), knowing that the majority of the participants did not consume alcohol, were significantly higher for controls than for cases. In addition, practicing sport regularly (p = 0.04), frequency of practicing sport (p < 0.001), and duration of sport each time (p = 0.015) were significantly higher for cases than for controls. Nonsignificant difference was found between cases and controls regarding BMI, specific diet, and smoking (p > 0.05).
| Variables | RA* [n (%)] | Control [n (%)] | p-Value |
|---|---|---|---|
| BMI | 0.262 | ||
| Underweight | 12 (13.3) | 33 (18.3) | |
| Normal | 27 (30) | 37 (20.6) | |
| Overweight | 30 (33.3) | 72 (40) | |
| Obese | 21 (23.3) | 38 (21.1) | |
| Specific diet | 0.900 | ||
| No | 36 (40) | 72 (40) | |
| Yes | 54 (60) | 108 (60) | |
| Smoking | 0.161 | ||
| No | 54 (60) | 98 (54.4) | |
| Yes | 27 (30) | 72 (40) | |
| Past smoker | 9 (10) | 10 (5.6) | |
| Number of cigarettes/day | 0.048 | ||
| 0 | 53 (58.9) | 98 (54.4) | |
| <10 | 6 (6.7) | 23 (12.8) | |
| 10–20 | 11 (12.2) | 38 (21.2) | |
| 20–40 | 9 (10) | 11 (6.1) | |
| >40 | 11 (2.2) | 10 (5.6) | |
| Alcohol | 0.033 | ||
| No | 86 (95.6) | 167 (92.8) | |
| Yes | 4 (4.4) | 13 (5.6) | |
| Sport | 0.040 | ||
| No | 56 (62.2) | 133 (73.9) | |
| Yes | 34 (37.8) | 47 (26.1) | |
| Sport (times/week) | <0.001 | ||
| 0 | 47 (52.2) | 121 (67.2) | |
| <3 | 14 (15.6) | 38 (21.1) | |
| >3 | 29 (32.2) | 21 (11.7) | |
| Duration of sport each time (min) | 0.015 | ||
| 0 | 47 (52.2) | 121 (67.2) | |
| ≤30 | 21 (23.3) | 38 (21.1) | |
| >30 | 22 (24.4) | 21 (11.7) | |
| Total | 90 (33.3) | 180 (66.7) |
RA, rheumatoid arthritis; [n (%)], frequencies (percentages); BMI, body mass index. p < 0.05 is considered significant.
Rheumatoid arthritis and lifestyle-related variables
3.3. Medical and Medication History
Table 3 shows that significant differences were found between RA patients and controls in case of: medication taken, suffering from at least one comorbid condition, duration of morning stiffness (p < 0.001), and taking drug regularly (p = 0.045). Nonsignificant difference was found between the two groups regarding the following variables: perform lab test regularly and regular physician visit (p > 0.05).
| Variables | RA* [n (%)] | Control [n (%)] | p-Value |
|---|---|---|---|
| Medication taken | <0.001 | ||
| Rheumatoid drugs | 88 (97.8) | 0 (0) | |
| Other drugs | 2 (2.2) | 180 (100) | |
| Taking drug regularly | 0.045 | ||
| No | 7 (7.8) | 30 (16.7) | |
| Yes | 83 (92.2) | 150 (83.3) | |
| Perform lab test regularly | 0.214 | ||
| No | 21 (23.3) | 55 (30.6) | |
| Yes | 69 (76.7) | 125 (69.4) | |
| Regular physician consultation | 0.838 | ||
| No | 20 (22.2) | 70 (77.8) | |
| Yes | 42 (23.3) | 138 (76.7) | |
| At least one comorbiditya | <0.001 | ||
| No | 55 (61.1) | 5 (2.8) | |
| Yes | 35 (38.9) | 175 (97.2) | |
| Duration of morning stiffness (min) | <0.001 | ||
| 0 | 1 (1.1) | 137 (96.1) | |
| <10 | 44 (48.9) | 4 (2.2) | |
| 10–30 | 45 (50) | 3 (1.7) | |
| Total | 90 (33.3) | 180 (66.7) |
RA, rheumatoid arthritis; [n (%)], frequencies (percentages).
Cardiovascular diseases, diabetes mellitus, psychological disorders, cancer, obstructive pulmonary disease, and osteoporosis. p < 0.05 is considered significant.
Rheumatoid arthritis and health-related variables
3.4. Health-related Quality of Life
Figure 1 shows differences in SF-36 dimension scores and total QOL between cases and controls. This bivariate analysis showed that for four dimensions (PF, RP, RE, and VT), the two scores PCS (p < 0.001) and MCS (p = 0.031), and the total QOL (p < 0.001) were significantly lower in RA patients than in controls. However, GH was significantly higher for cases than for controls (p = 0.04). Nonsignificant difference was found regarding MH (P = 0.45), SF (p = 0.967), and BP (p = 0.156).
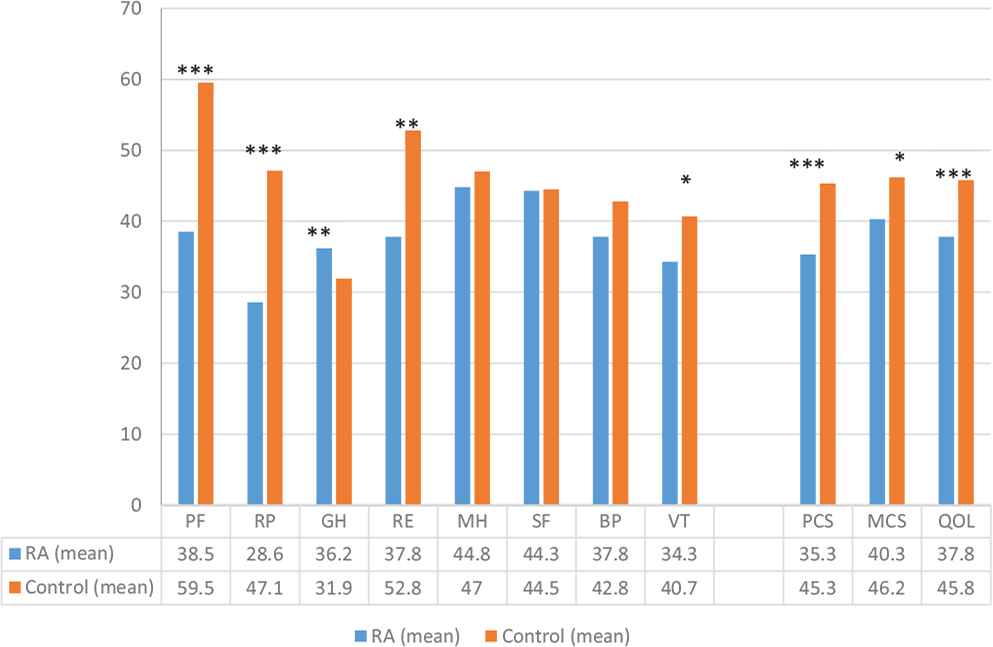
Mean scores of the eight dimensions, physical and mental component summaries, and the overall score of quality of life of the SF36, comparing RA and control groups. *0.01 ≤ p < 0.05, **0.001 ≤ p < 0.01, ***p < 0.001 are statistically significant. BP, body pain; GH, general health perception; MCS, mental component; MH, mental health; QOL, quality of life; PCS, physical component; PF, physical functioning; RA, rheumatoid arthritis; RE, emotional role limitation; RP, physical role limitation; SF, social functioning; VT, vitality. Data are presented as means; statistical significance was tested using t-test.
3.5. Intragroup Analysis of QOL and its Components among Control Group
In the multivariable linear regression model estimating the predictor of PCS (Table 4), we found that age [β = −6.750, p < 0.001, 95% confidence interval (CI): (−10.292; −3.207)], BMI [β = −2.907, p = 0.036, 95% CI: (−5.617; −0.197)], and morning stiffness ≥10 min [β = −26.366, p = <0.001, 95% CI: (−37.575; −15.158)] were negatively associated with PCS. Number of cigarettes per day [β = 3.575, p = 0.001, 95% CI: (1.453; 5.696)], education level [β = 3.425, p = 0.030, 95% CI: (0.345; 6.506)], and workability [β = 5.143, p = 0.003, 95% CI: (1.738; 8.548)] were positively associated with PCS.
| Predictors | Standardized β | Unstandardized β | 95% CI* | p-Value |
|---|---|---|---|---|
| PCS | ||||
| Age | −0.282 | −6.750 | −10.292; −3.207 | <0.001 |
| Number of cigarettes per day | 0.219 | 3.575 | 1.453; 5.696 | 0.001 |
| BMI | −0.147 | −2.907 | −5.617; −0.197 | 0.036 |
| Education level | 0.190 | 3.425 | 0.345; 6.506 | 0.030 |
| Workability | 0.210 | 5.143 | 1.738; 8.548 | 0.003 |
| Morning stiffness | −0.387 | −26.366 | −37.575; −15.158 | <0.001 |
| MCS | ||||
| Income | 0.202 | 4.727 | 0.278; 9.175 | 0.037 |
| Workability | 0.197 | 4.991 | 0.826; 9.155 | 0.019 |
| Morning stiffness | −0.354 | −25.009 | −38.718; −11.200 | <0.001 |
| Comorbidity | −0.285 | −35.941 | −59.988; −11.895 | 0.004 |
| Overall QOL | ||||
| Age | −0.198 | −3.533 | −6.340; −0.726 | 0.014 |
| Number of cigarettes per day | 0.159 | 1.931 | 0.251; 3.612 | 0.025 |
| Workability | 0.278 | 5.067 | 2.370; 7.765 | <0.001 |
| Morning stiffness | −0.505 | −25.688 | −34.568; −16.807 | <0.001 |
| Comorbidity | −0.304 | −27.552 | −43.128; −11.975 | 0.001 |
CI, confidence interval; β, regression coefficient; BMI, body mass index; MCS, mental component score; PCS, physical component score; QOL, quality of life. p < 0.05 is considered significant.
Multivariable analysis of QOL and its components among controls (N = 180)
In the multivariable linear regression model estimating the predictor of MCS (Table 4), our results show that morning stiffness [β = −25.009, p < 0.001, 95% CI: (−38.718; −11.200)] and comorbidity [β = −35.941, p = 0.004, 95% CI: (−59.988; −11.895)] are negatively associated with MCS. However, income [β = 4.727, p = 0.037, 95% CI: (0.278; 9.175)] and work ability [β = 4.991, p = 0.019, 95% CI: (0.826; 9.155)] positively affect MCS.
In addition, we found that age [β = −30.790, p = 0.006, 95% CI: (−52.710; −8.860)], morning stiffness [β = −25.688, p < 0.001, 95% CI: (−34.568; −16.807)], and comorbidity [β = −27.552, p = 0.001, 95% CI: (−43.128; −11.975)] are negatively associated with overall QOL score. However, number of cigarettes per day [β = 1.931, p = 0.025, 95% CI: (0.251; 3.612)] and workability [β = 5.067, p < 0.001, 95%, CI: (2.370; 7.765)] are positively associated with QOL (Table 4).
3.6. Intragroup Analysis of QOL and its Components among RA Group
In the multivariable linear regression model estimating the predictor of PCS (Table 5), we found that the number of times of sport activity per week [β = 6.692, p = 0.002, 95% CI: (2.619; 10.766)] and work ability [β = 5.546, p = 0.022, 95% CI: (0.812; 10.281)] are positively associated with PCS. The lapse of time between blood transfusion and onset of the disease [β = −9.211, p = 0.013, 95% CI: (−17.773; −0.650)] is positively associated with MCS; however, morning stiffness [β = 8.415, p = 0.007, 95% CI: (2.340; 14.490)] is negatively associated with MCS (Table 5).
| Predictors | Standardized β | Unstandardized β | 95% CI* | p-Value |
|---|---|---|---|---|
| PCS | ||||
| Sport times per week | 0.324 | 6.692 | 2.619; 10.766 | 0.002 |
| Workability | 0.264 | 5.546 | 0.812; 10.281 | 0.022 |
| MCS | ||||
| Time between blood transfusion and onset of the disease | 0.257 | 8.415 | 2.340; 14.490 | 0.007 |
| Morning stiffness | −0.227 | −9.211 | −17.773; −0.650 | 0.013 |
| Overall QOL | ||||
| Sport times/week | 0.312 | 6.148 | 2.214; 10.081 | 0.003 |
| Morning stiffness | −0.272 | −9.190 | −16.027; −2.353 | 0.009 |
CI, confidence interval; β, regression coefficient; MCS, mental component score; PCS, physical component score; QOL, quality of life. p < 0.05 is considered significant.
Multivariable analysis of QOL and its components among cases (N = 90)
Table 5 also shows that the number of times of sport activity per week [β = 6.148, p = 0.003, 95% CI: (2.214; 10.081)] is positively associated with the overall QOL among RA patients; however, morning stiffness is negatively associated with the overall QOL [β = −9.190, p = 0.009, 95% CI: (−16.027; −2.353)].
4. DISCUSSION
Quality of life has been the objective of several studies evaluating the impact of chronic diseases [14], cardiovascular diseases [12,13], dyslipidemia [15], and hypertension [16,17]. Any disease, especially chronic, affects QOL, physical, emotional, and social well-being, and the QOL measure is considered an important factor in the assessment of an individual’s health status. RA is a preventable, autoimmune, systemic, and chronic disease. Many studies have evaluated the impact of RA on QOL worldwide [18]; however, there is lack of information in this field in Lebanon.
This is the first study conducted in Lebanon using case–control design to evaluate the impact of RA on the Lebanese patients’ QOL and to suggest possible predictors of their QOL. Controls were selected using some similar criteria as cases and identified during the same time period as the cases. As age and gender are two variables highly associated with changes in QOL, our controls were not matched on these two variables to prevent overmatching that can lead to biased results. In addition, cases were recruited based on diagnosis confirmed by a clinical rheumatologist. However, our study was limited by the fact that the severity of disease and the details on treatments received by the patients, as well as their impacts on QOL, were not taken into account.
In our study, we have used the SF-36 health survey, which is a reliable tool for the assessment of the QOL in Lebanon [15,16] and to assess the HRQoL of patients with RA [18]. Our results indicate that females were more affected by RA than males. These results are similar to those from other studies that demonstrated that women are more likely to develop RA than men and it is two to three times more prevalent in women than in men [2,10]. Most of RA patients in our study were aged between 36 and 50 years. A study conducted in a Dutch nationwide group of 1056 patients showed that the onset of RA reaches a peak between the ages of 40 and 50 years [10].
Suffering from RA deteriorates the physical health status as was seen in a descriptive study with 53 patients from a public rheumatology center in Montevideo, Uruguay. The study showed that RA is associated with higher disease burden, reflected on pain, impact on global health, and functional and working status, as well as the physical and emotional dimensions of the HRQoL [19].
In this study, RA had a negative influence on both physical (p < 0.001) and mental components (p = 0.031), where PCS and MCS for cases were lower than those in controls. These findings are consistent with a US study, where RA patients were taken as civilian non-institutionalized adults aged 18 years or older from 15 states, and conducted over a large population, participants with RA reported lower scores on the overall health perception of SF-36, physical and mental functioning scales as compared with participants without RA [14]. Bivariate analysis shows that five dimensions (PF, RP, RE, MH, and BP) were lower in the RA patients than in the non-RA patients. However, one dimension (GH) was higher in RA patients than in controls. This variability in GH may be due to bias as some controls were taken from those having more severe comorbidities than RA, such as cancer.
In addition, our study shows that RA patients had significantly lower QOL (p < 0.001) and lower level of HRQoL in comparison to non-RA conditions. Similarly, RA negatively impacts HRQoL: pooled scores for the physical domains are somewhat lower than the mental health domains, suggesting that RA has a greater impact on physical HRQoL than mental well-being. This finding can be explained by either the evidence of strong family support and a strong social environment among patients or evidence of suppressed feelings among patients. Similar results were found in previous meta-analysis studies [9,12].
Having morning stiffness deteriorates the physical functions as shown in a European study that was conducted on 1061 patients and concluded that morning stiffness reduces the ability to work in patients with RA [20].
Interestingly, the multivariable analysis of QOL and its components shows that the number of times of exercise performed per week has a positive impact on both PCS as well as overall QOL, especially in RA patients. Exercise and sports are important for RA patients for maintaining healthy and strong muscles, preserving joint mobility, and maintaining flexibility. Exercise can also help people sleep well, reduce pain, maintain a positive attitude, and manage weight as stated in an American study [2]. Another study revealed that exercise improves QOL, where participants reported that sport influenced their mental and physical health positively even if they had mobility limitation [17].
The number of cigarettes per day has a positive impact on PCS in the control group in the multivariate analysis. This may be due to the fact that in Lebanon, smoking is a socially acceptable behavior. Smokers may bond together more strongly and create and maintain social relations of their habit. In addition, smokers may present a healthier group of survivors. This selection effect could suggest a positive health for smokers.
Rheumatoid arthritis impact on work can be profound as permanent work disability is common among patients with RA where their ability to meet work demands is limited. Hence, those patients will become jobless as patients who experience at-work productivity loss are prone to develop sick leave, permanent work disability in the future, and low QOL as seen in a cross-sectional study conducted in Amsterdam [11]. Although a Canadian study stated that reduced physical function due to RA is associated with an increased probability of inability to work or absence from work due to RA-associated sickness [6]. In our study, work ability has a positive impact on PCS in both RA and non-RA patients, as well as on MCS and overall QOL in control group suffering from other diseases such as hypertension, cancer, congestive heart failure, myocardial infarction, clinical depression, type 2 diabetes, and so on. This is consistent with a cross-sectional study carried out on 224 employees in the city of Sao Paulo, Brazil, in 2001. All evaluated dimensions of health were significantly associated with work ability (p < 0.0001). Results showed that, independently of other characteristics, better physical and mental health are associated with greater work ability [21].
According to the National Arthritis Data Workgroup, pain and stiffness in RA patients last for >30 min in the morning or after a long rest [2]. On the other hand, having morning stiffness deteriorates the physical functions as seen in the results of a European study that was conducted on 1061 patients and concluded that morning stiffness reduces the ability to work in patients with RA [20]. Similarly, our study reveals that morning stiffness has a negative impact on both MCS and the overall QOL in RA patients; however, this is not specific to RA patients as it is also valid for non-RA patients where morning stiffness has negative impact on PCS, MCS, and overall QOL.
Finally, the lapse of time between blood transfusion and the onset of RA has a positive impact on MCS of RA patients. This may be due to the fact that RA patients were reassured that the disease was not inoculated to them by blood transfusion.
5. CONCLUSION
Rheumatoid arthritis is a common and major health problem in the adult population. This is the first study in Lebanon to assess the QOL of RA patients. RA patients presented lower QOL scores as compared with control. Therefore, it is essential to find medical and social alternatives that have a favorable effect on QOL of RA patients. To improve QOL of patients with RA, this study highlights the importance of campaigns on educating patients, especially with respect to life style habits such as practicing sports regularly and having good work ability, which is important when supporting patients with RA. In addition, finding alternative treatment that reduces morning stiffness will also improve the QOL of RA patients.
This study was a preamble to organize larger studies at the national level in the future seeking to determine risk factors leading to RA and to suggest possible predictors of QOL and finally that will help to further generalize our results.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHOR CONTRIBUTIONS
S.A., M.S. and W.B. were responsible for planning and design of the study; M.S. was responsible of data collection; M.S., R.A. were responsible for statistical analysis; S.A., A.A-H., S.R. and S.Z. were involved in the preparation of questionnaire; M.S. wrote the first draft; W.A., S.A. and R.A. provided critical revision. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
The authors thank the Lebanese University for supporting this project.
REFERENCES
Cite this article
TY - JOUR AU - Sanaa Awada AU - Roula Ajrouche AU - Mariam Shoker AU - Amal Al-Hajje AU - Samar Rachidi AU - Salam Zein AU - Wafaa Bawab PY - 2019 DA - 2019/09/09 TI - Rheumatoid Arthritis in the Lebanese Adults: Impact on Health-Related Quality of Life JO - Journal of Epidemiology and Global Health SP - 281 EP - 287 VL - 9 IS - 4 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.190820.001 DO - 10.2991/jegh.k.190820.001 ID - Awada2019 ER -
